
Duk-Woo Park, MD
Asan Medical Center, Korea (Republic of)
At TCTAP 2023, Duk-Woo Park, MD (Asan Medical Center, Korea) shared insights from the MAINCOMPARE, SYNTAX, PRECOMBAT, NOBLE, and EXCEL trials and emphasized the importance of discussing the potential benefits, advantages, and disadvantages of the procedures with the cardiac surgeon.
In the past two decades, several trials have been conducted to study left main and multi-vessel disease, including the SYNTAX, PRECOMBAT, EXCEL, and NOBLE trials. These trials have shown significant progress in both percutaneous coronary intervention (PCI) and bypass surgery for these conditions. While the surgery was consistently shown to be better for multi-vessel disease, there were differences in primary endpoints for left main disease among the trials.
The Asan team conducted several registries and clinical trials, including the MAIN-COMPARE registry in NEJM, the PRECOMBAT for left main, and the BEST for multi-vessel disease. Recently, the team performed a 10-year follow-up on the PRECOMBAT trial, which showed no statistical difference in the primary endpoint but did reveal a difference in ischemic-driven target vessel revascularization (TVR).
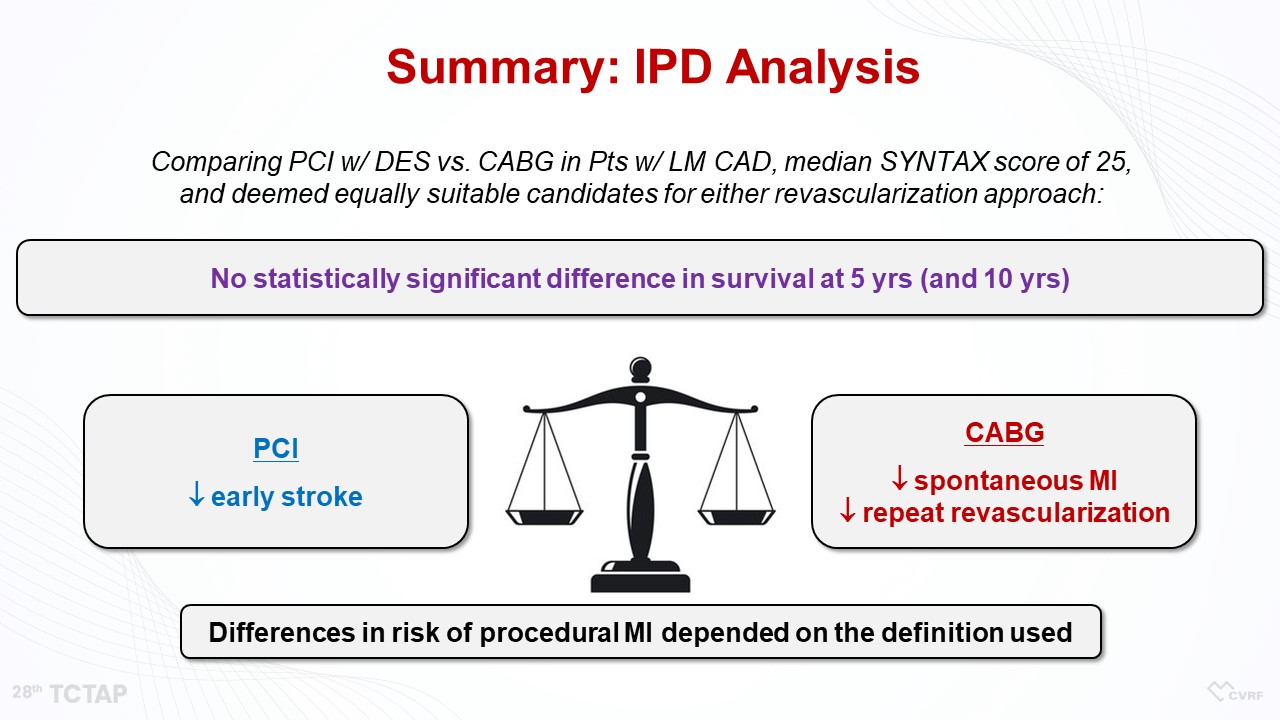
The controversy surrounding left main and bypass surgery is related to the EXCEL trial, where a mortality difference was observed but the primary endpoint of up to five years had some crossover with no statistical difference. An individual participant data (IPD) meta-analysis was conducted and published in the Lancet journal, which showed no difference in overall mortality between PCI and coronary artery bypass graft surgery (CABG) up to 5 years and up to 10 years in the SYNTAX and PRECOMBAT trials (Figure 1).
The updated ACC guideline recommends bypass surgery for left main disease as a Class I recommendation, while PCI could be optional and is a Class IIa recommendation. The ESC has not yet updated its guidelines, which still recommends bypass surgery as a consistent Class I and PCI as a Class I, IIA, or III according to the SYNTAX category.
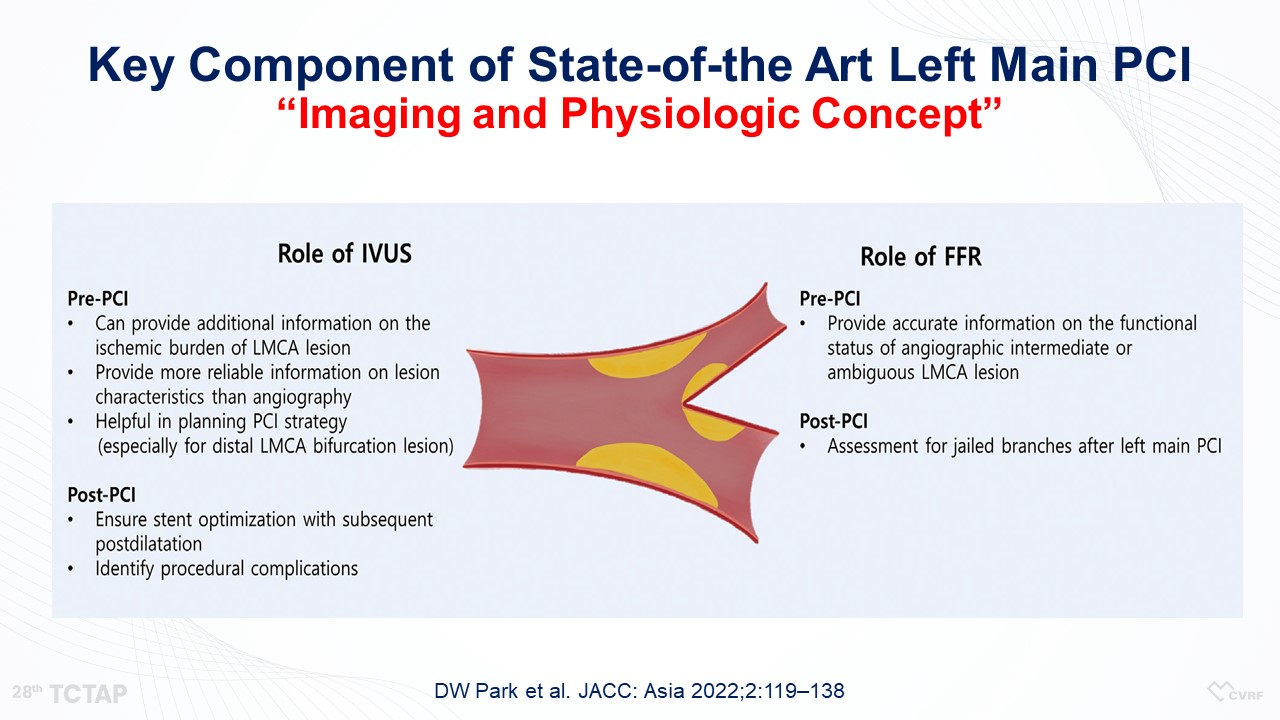
There are still unmet needs, such as no further clinical trial comparing PCI and bypass surgery for left main being planned. The definition of myocardial infarction (MI) is still controversial, and complete and incomplete revascularization, the role of intravascular ultrasound (IVUS) and fractional flow reserve (FFR) in left main revascularization, and all-cause mortality versus cardiac mortality still require adjudication. Long-term follow-up data of big trials beyond five years up to 10 years is absolutely required, and the SYNTAX score is still questionable.
One major issue is how to equalize left main PCI technique, as data shows that left main PCI procedures only make up 1.0% of all procedures in the United States over time in daily practice, which indicates a need for more operator training.
The latest development in state-of-the-art PCI is the incorporation of imaging and physiology. This involves the use of IVUS and FFR, which play important roles in improving the outcomes of PCI. The future of PCI for left main disease could involve adopting this imaging and physiologic concept (Figure 2).
Hot Topics
Left Main & Multi-Vessel (Concept Changes After ISCHEMIA)
Sunday, May 7, 3:54 PM - 4:10 PM
Presentation Theater 1, Vista 3, B2
Edited by

Jinho Lee, MD
Kyung Hee University Medical Center, Korea (Republic of)

