
Sripal Bangalore, MD
New York University Grossman School of Medicine, USA
Dr. Sripal Bangalore (New York University Grossman School of Medicine, USA) and Dr. David Paul Taggart (University of Oxford, UK) had a heated debate regarding the treatment of multi-vessel disease (MVD), with Dr. Bangalore advocating for medical treatment and Dr. Taggart favoring surgery.
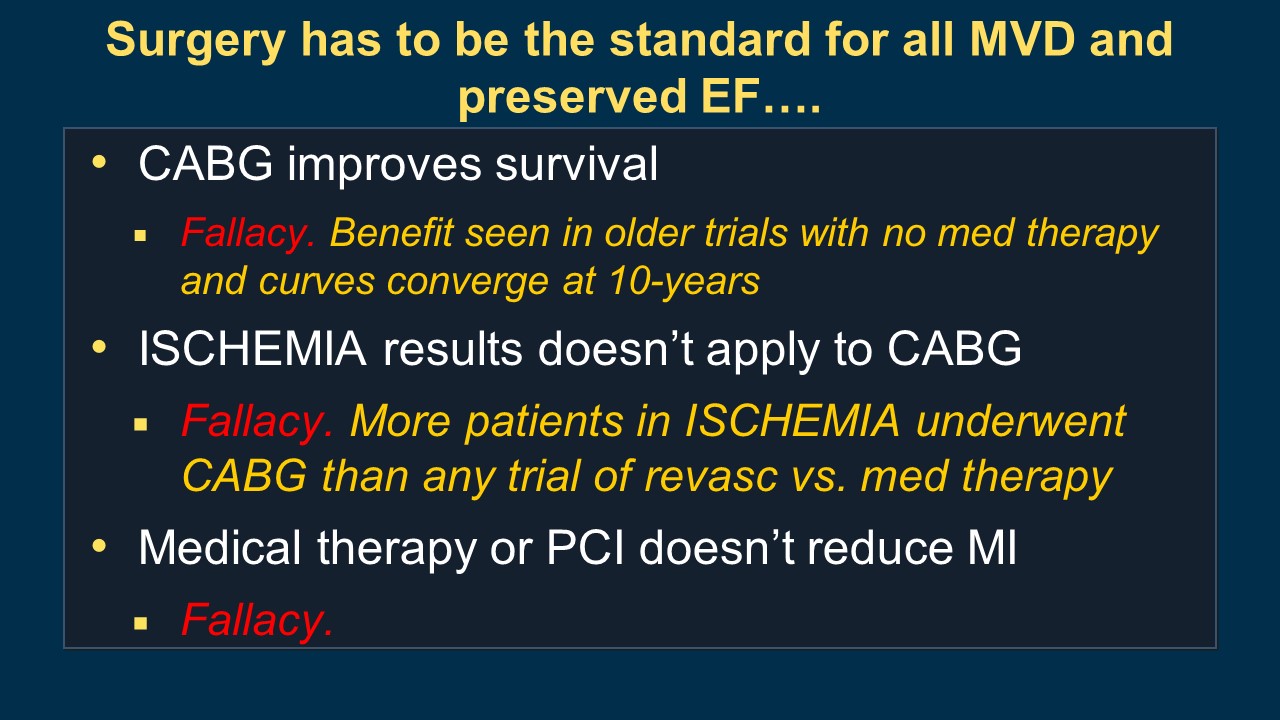
Dr. Bangalore began the debate by acknowledging that coronary artery bypass grafting (CABG) can improve survival rates. He also argued that the results of the ISCHEMIA trial, which studied the effectiveness of different treatments for stable ischemic heart disease (IHD), do not necessarily apply to CABG. Additionally, he asserted that neither medical therapy nor percutaneous coronary intervention (PCI) reduces the risk of myocardial infarction (MI) in patients with MVD.
Thus, he brought up the debate topic of whether CABG improves overall survival in patients with MVD and preserved left ventricular systolic function.
Dr. Bangalore presented a recent meta-analysis showing routine revascularization was not associated with improved survival compared with medical treatment in patients with stable IHD (Figure 1). In addition, he referenced the BARI-2D CABG Stratum and MASS II 10 years follow-up, which did not show the mortality benefit of CABG over guideline-directed medical therapy (GDMT). He also stated that the ISCHEMIA trial included a larger number of patients who underwent CABG than other clinical trials that have compared revascularization with medical treatment, but it did not conclude that revascularization is superior to medical treatment.
Unlike PCI or CABG, advanced medical therapy provides a systemic approach to the treatment of MVD. This approach involves the use of various medications, including beta blockers, ACE inhibitors or ARBs, statins, PCSK9 inhibitors, DOACs, antiplatelet medications, and SGLT2 inhibitors. These medications have been shown to provide survival benefits and improve cardiovascular clinical outcomes in patients with MVD. In some cases, advanced medical therapy may be an alternative to revascularization procedures such as PCI or CABG, especially in patients who are not candidates for these procedures due to various reasons such as comorbidities or personal preferences.
He concluded that medical therapy, with or without PCI, is sufficient for most patients with MVD with CABG reserved for those with complex coronary disease.

David Paul Taggart, MD
University of Oxford, United Kingdom
Dr. Taggart still maintains the view that CABG is still the standard treatment approach for patients with MVD.
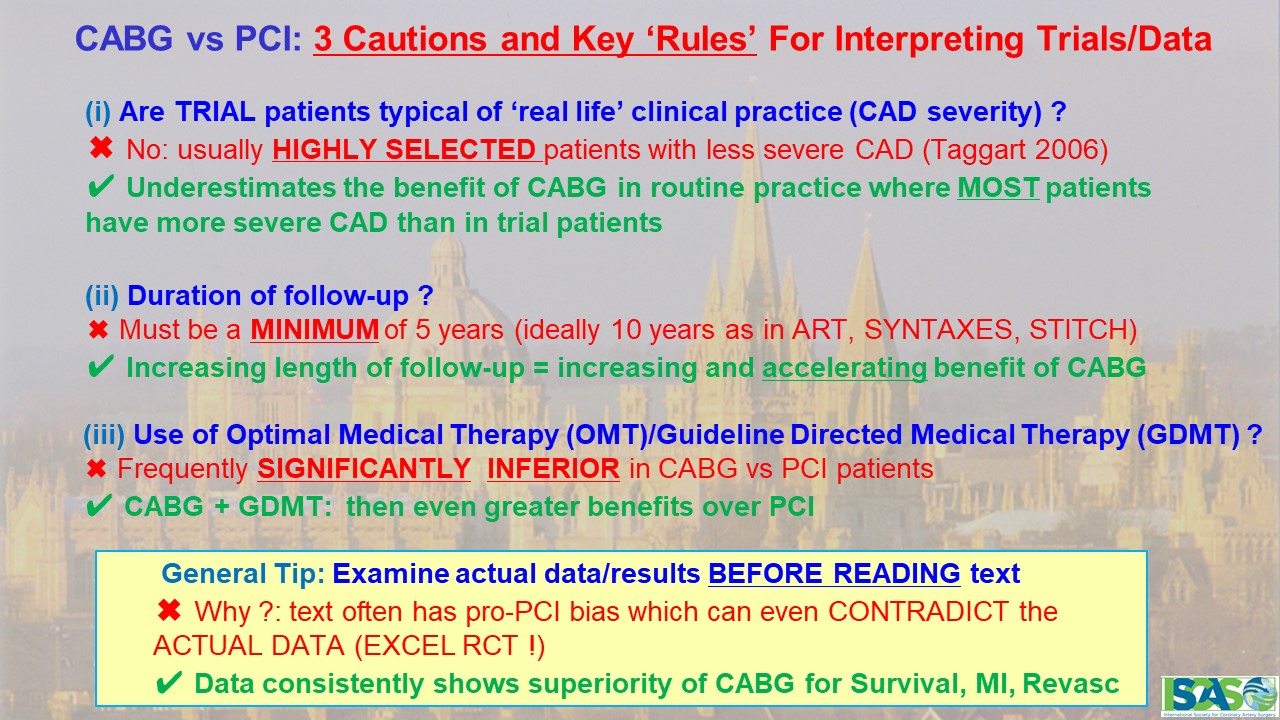
First of all, he emphasized three cautions and key rules for interpreting trials and data of PCI vs. CABG; 1) the trial patients may not represent the typical patient population encountered in routine clinical practice (Figure 2). In other words, the patients in clinical trials may have less severe coronary artery disease (CAD) than patients encountered in routine practice. Therefore, the benefits of CABG observed in clinical trials may be underestimated in routine practice where most patients have more severe CAD. 2) the duration of follow-up is critical when interpreting data from trials comparing PCI and CABG. He noted that a minimum of 5 years of follow-up is necessary, with an ideal follow-up period of 10 years, as seen in trials such as ART, SYNTAXES, and STITCH. The longer the follow-up period, the greater and more accelerated the benefit of CABG becomes. 3) the use of CABG with GDMT has been shown to have even greater benefits over PCI. Therefore, it is important to ensure that patients undergoing CABG receive optimal medical therapy to maximize the benefits of the procedure.
Dr. Taggart presented various clinical trials, including SYNTAX, FREEDOM, FAME III, and STITCH trials, as well as observational studies, to demonstrate that CABG provides superior mortality and cardiovascular outcomes compared to PCI or medical treatment alone. He stressed the effectiveness of CABG by citing the 2018 guidelines on myocardial revascularization which classified CABG as Class I and highlighted that CABG could be more beneficial with more arterial grafts and optimal medical treatment.
Dr. Taggart also gave three reasons for the persisting survival benefit of CABG over PCI. Firstly, anatomically, atheroma is mainly located in the proximal coronary arteries, which makes CABG more effective because it bypasses the diseased segment. Secondly, the internal mammary artery is known to elute nitric oxide (NO) into the coronary circulation, which has a beneficial effect on the endothelium and reduces the risk of further disease. On the other hand, drug-eluting stents used in PCI can impair reendothelialization and downstream endothelial function, which creates a pro-thrombotic environment and may increase the risk of further cardiovascular events. Lastly, PCI can sometimes result in incomplete revascularization, meaning that not all blocked or narrowed vessels are treated during the procedure. In contrast, CABG aims to provide complete revascularization by bypassing all significant blockages in the coronary arteries.
He concluded that CABG is considered the standard, but PCI or medical treatment may be considered in cases of multiple comorbidities, frailty, or reduced life expectancy.
Hot Topics
Left Main & Multi-Vessel (Concept Changes After ISCHEMIA)
Sunday, May 7, 3:54 PM - 4:10 PM
Presentation Theater 1, Vista 3, B2
Edited by

Osung Kwon, MD
The Catholic University of Korea Eunpyeong St. Mary's Hospital, Korea (Republic of)

