
Jung-Min Ahn, MD
Asan Medical Center, Korea (Republic of)
Clinical trials in the era of drug-eluting stents (DES) have shown that percutaneous coronary intervention (PCI) including SYNTAX (Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery) and FREEDOM (Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease) has a higher risk of repeat revascularization, spontaneous myocardial infarction, and mortality in multivessel coronary artery disease (MVCAD) patients. Previous trials using first-generation DES and little use of intracoronary imaging have limited applicability in contemporary practice. However, the new-generation DES have a lower incidence of cardiac events and mortality than first-generation stents, and intracoronary imaging can optimize the PCI results.
The BEST (Randomized Comparison of Coronary Artery Bypass Surgery and Everolimus-Eluting Stent Implantation in the Treatment of Patients With Multivessel Coronary Artery Disease) trial, which randomly assigned MVCAD patients to undergo either PCI with everolimus-eluting stents or coronary artery bypass grafting (CABG), demonstrated that CABG significantly reduced the composite rate of death, myocardial infarction (MI), or target vessel revascularization. Nevertheless, there was no significant difference in mortality between the two groups. The present study aims to evaluate longer-term outcomes between the two treatments in MVCAD patients who were followed up for up to 13.7 years.
The BEST trial was a prospective, open-label, randomized trial comparing PCI with everolimus-eluting stents and CABG in MVCAD patients and was conducted at 27 international heart centers. The primary endpoint was the incidence of major adverse cardiac events (MACE), such as death from any cause, MI, or target vessel revascularization. The major secondary endpoints are a safety composite of death, MI or stroke, and a composite of death, MI, stroke, or any repeat revascularization.
A total of 880 MVCAD patients were randomized, with 438 receiving PCI with everolimus-eluting stents and 442 undergoing CABG. The median length of follow-up after randomization was 11.8 years (interquartile range, 10.6-12.5 years; the maximum follow-up, 13.7 years) without significant difference between groups. The mean age of the patients was 64.5±9.4 years; 41% had diabetes; and 77% had 3-vessel coronary artery disease. The baseline demographics and clinical, angiographic characteristics of the patients were well-matched between the two groups. The SYNTAX score was 24.4±7.8 and complete revascularization was achieved in 50.9% and 71.5% of the patients in the PCI group and the CABG group, respectively.
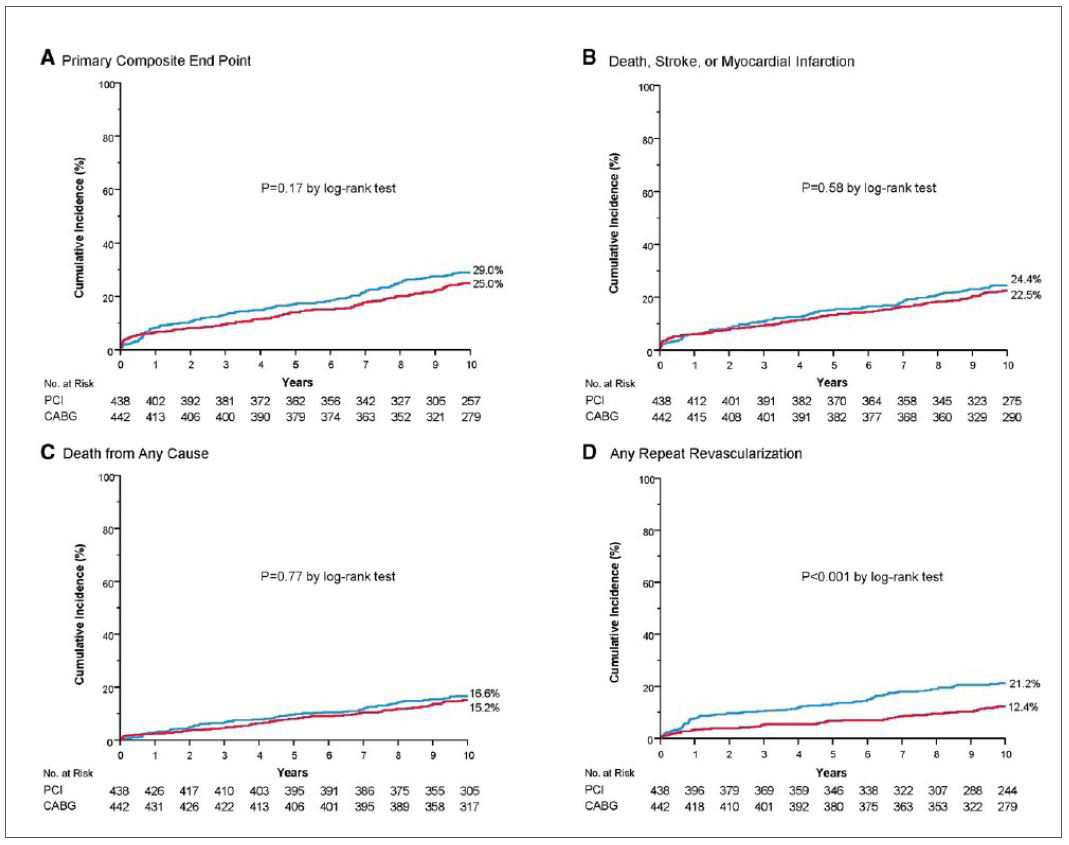
The primary endpoint occurred in 151 patients (34.5%) in the PCI group and 134 patients (30.3%) in the CABG group (hazard ratio [HR], 1.18; 95% confidence interval [CI], 0.88-1.56; P=0.26) (Figure 1A). There was no significant between-group difference in the secondary safety composite endpoint of death, stroke, or MI (28.8% and 27.1%; HR, 1.07; 95% CI, 0.75-1.53; P=0.70) and death from any cause (20.5% and 19.9%; HR, 1.04; 95% CI, 0.65-1.67; P=0.86) (Figure 1B and 1C). However, the incidence of spontaneous MI (7.1% and 3.8%; HR, 1.86; 95% CI, 1.06-3.27; P=0.03) and repeat revascularization (22.6% and 12.7%; HR, 1.92; 95% CI, 1.58-2.32; P<0.001) was higher after PCI than after CABG (Figure 1D).
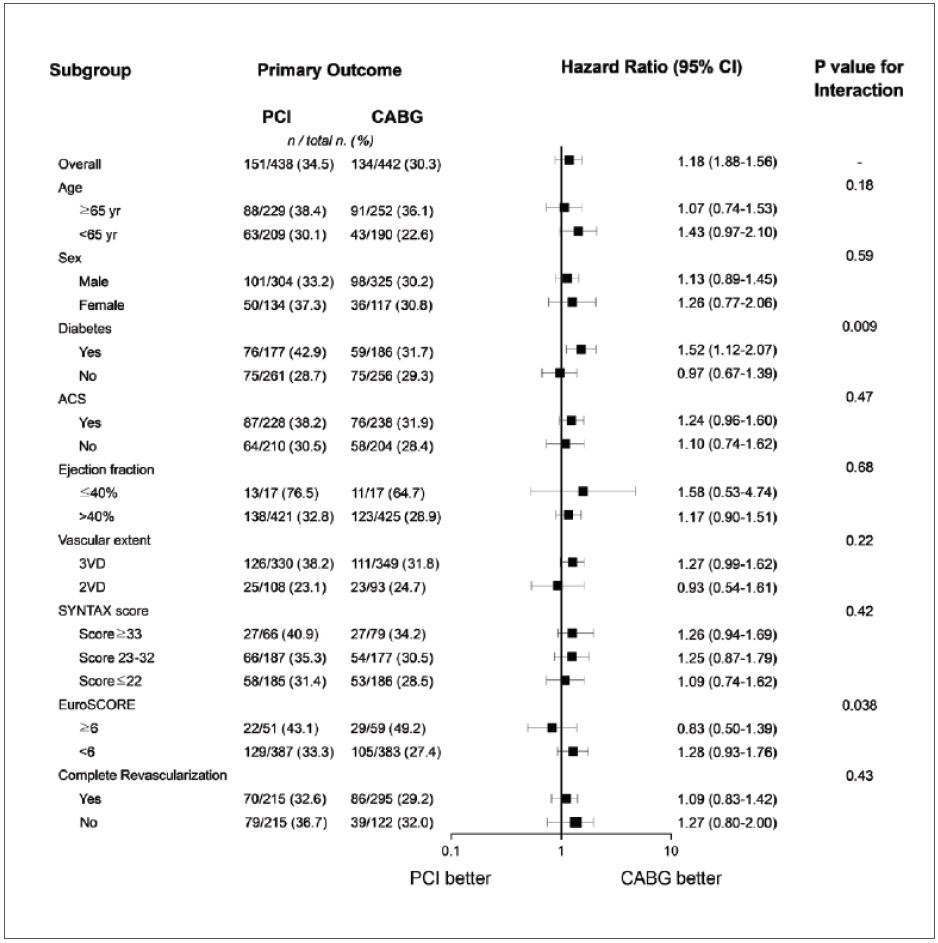
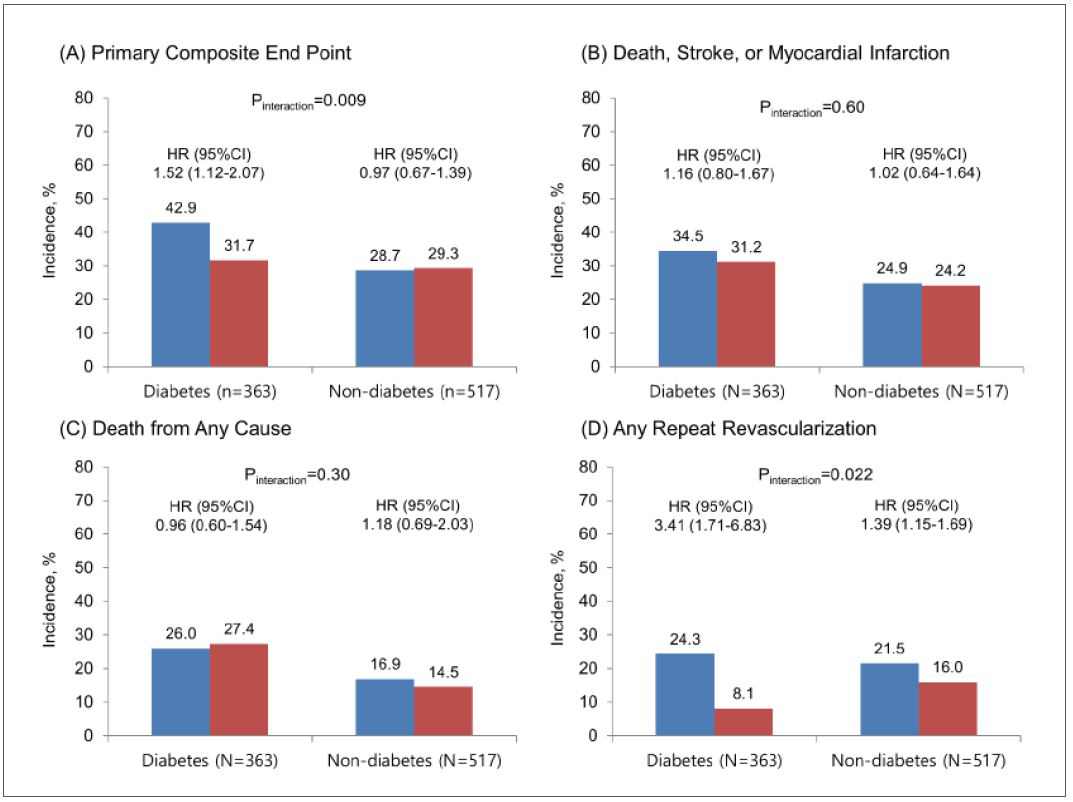
Pre-specified subgroup analyses are presented (Figure 2), and a significant interaction between the treatment assignment and diabetes status was expected (P=0.009). Among patients with diabetes, PCI significantly increased the risk of the primary endpoint (42.9% and 31.7%; HR, 1.52; 95% CI, 1.12-2.07; P=0.007) compared with CABG. In contrast, the primary endpoint did not differ significantly between the two groups in patients without diabetes (28.7% and 29.3%; HR, 0.97; 95% CI, 0.67-1.39; P=0.79). Overall mortality was also similar between groups in patients with diabetes (26.0% and 27.4%; HR, 0.96; 95% CI, 0.60-1.54; P=0.87) (Figure 3).
This study is expected to provide valuable insights into the comparative long-term outcomes of PCI with everolimus-eluting stents and CABG in MVCAD patients.
Clinical Science
Late-Breaking Clinical Trials 2023 in Asia-Pacific
Monday, May 08, 9:30 AM - 10:50 AM
Presentation Theater 1, Vista 3, B2
Edited by
Junghoon Lee, MD
The Catholic University of Korea, Eunpyeong St. Mary's Hospital, Korea (Republic of)

