Lack of Evidence for Routine Functional Testing after PCI

Duk-Woo Park, MD
Asan Medical Center, Korea (Republic of)
The effectiveness of regular stress functional testing after percutaneous coronary intervention (PCI) in improving clinical outcomes is uncertain. The 2019 European guidelines recommend non-invasive stress testing 6 months after high-risk PCI and coronary angiography 3-12 months later, and non-invasive stress testing 1 year after general PCI. However, the recommendations are weak (Class IIB recommendation, Level of evidence C), relying on expert opinions, and the 2021 ACC/AHA guidelines do not mention them.
POST-PCI Trial: Routine Functional Testing vs. Standard Care after High-Risk PCI
From November 2017 to September 2019, the POST-PCI investigators randomly assigned 1,706 patients with high-risk anatomical or clinical characteristics who had undergone PCI to a follow-up strategy of routine functional testing (nuclear stress testing, exercise electrocardiography, or stress echocardiography) at 1 year after PCI (849 patients), or to standard care alone (857 patients). The primary outcome was a composite of death from any cause, myocardial infarction (MI), or hospitalization for unstable angina at 2 years.
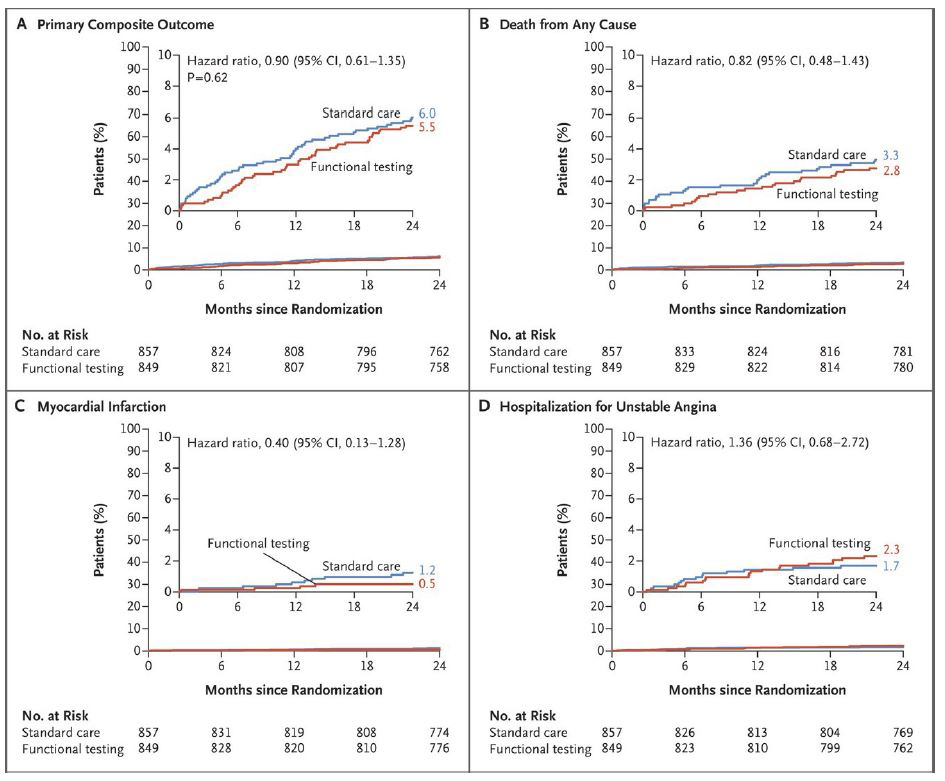
The mean age of the patients was 64.7 years, 21.0% had left main disease, 43.5% had bifurcation disease, 69.8% had multivessel disease, 70.1% had diffuse long lesions, 38.7% had diabetes, and 96.4% had been treated with drug-eluting stents. At 2 years, a primary outcome event had occurred in 46 of 849 patients (Kaplan-Meier estimate, 5.5%) in the functional-testing group and in 51 of 857 (Kaplan-Meier estimate, 6.0%) in the standard-care group (hazard ratio [HR], 0.90; 95% confidence interval [CI], 0.61-1.35; P=0.62) (Figure 1). There were no between-group differences with respect to the components of the primary outcome. At 2 years, 12.3% of the patients in the functional-testing group and 9.3% in the standard-care group had undergone invasive coronary angiography (difference, 2.99 percentage points; 95% CI, -0.01-5.99), and 8.1% and 5.8% of patients, respectively, had undergone repeat revascularization (difference, 2.23 percentage points; 95% CI, -0.22-4.68).
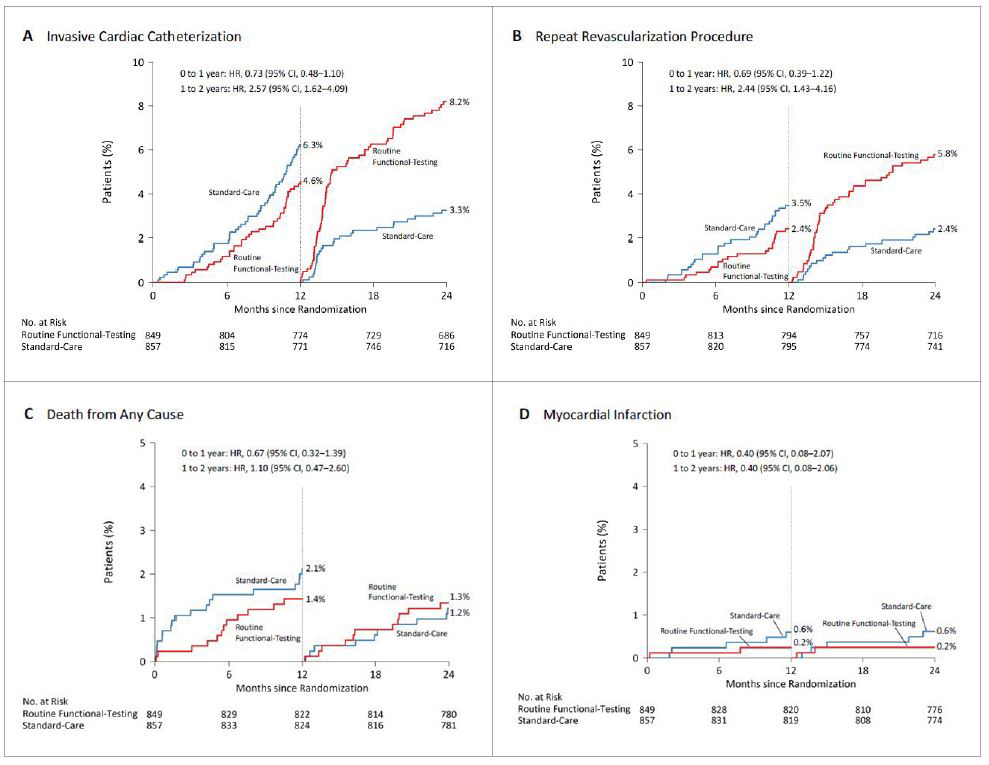
Further, a landmark analysis performed between 1 and 2 years showed a more than twofold higher incidence of coronary angiography (8.2% vs. 3.3%; HR, 2.57; 95% CI, 1.62-4.09) and revascularization (5.8% vs. 2.4%; HR, 2.44; 95% CI, 1.43-4.16) in the functional-testing group compared with the standard-care group. Yet, there were still no meaningful between group-differences in the rate of death or MI (Figure 2).
Despite more testing and repeat procedures based on the regular functional testing results, hard clinical endpoints such as death or MI were not reduced. The result was consistent with the recent ISCHEMIA study, which showed that an initial invasive strategy, as compared with an initial conservative strategy, did not reduce mortality or ischemic events among stable patients with myocardial ischemia. The POST-PCI trial results also showed that more aggressive and invasive testing and treatment did not provide additional clinical benefits over a conservative strategy based on guideline-directed medical therapy.
In this multicenter, pragmatic, randomized trial of high-risk patients who had undergone PCI, routine functional testing did not result in a lower risk of ischemic cardiovascular events or death from any cause at 2 years. Therefore, routine surveillance stress testing for post-PCI patients is not recommended unless they exhibit clinical signs or symptoms of stent failure.
Clinical Science
Late-Breaking Clinical Trials 2023 in Asia-Pacific
Monday, May 08, 9:30 AM - 10:50 AM
Presentation Theater 1, Vista 3, B2
Edited by

Hanbit Park , MD
GangNeung Asan Hospital, Korea (Republic of)

