
Nico Pijls, MD
Catharina Hospital, Netherlands
In the early days of coronary intervention, some pioneers in coronary intervention recognized the value of coronary artery pressure measurement. However, reliable techniques and devices to measure coronary pressure did not accurately exist at that time. With the development of the true pressure wire and hyperemic method, fractional flow reserve (FFR) was introduced in the 1990s. FFR is a fraction of mean distal coronary pressure (Pd) to mean aortic pressure (Pa) at maximal coronary hyperemia.
Today, FFR is used widely in clinical practice. Furthermore, many non-hyperemic methods to measure coronary pressure also have been developed to avoid the inconvenience that occurs during hyperemic stimulation. However, there are clear distinctions between FFR and non-hyperemic indices. FFR is linearly related to maximum achievable blood flow and this linearity is only present under maximum hyperemic circumstances. Clinically, leaving out hyperemia can miss significant stenosis, especially in younger patients with proximal lesions in large coronary arteries.
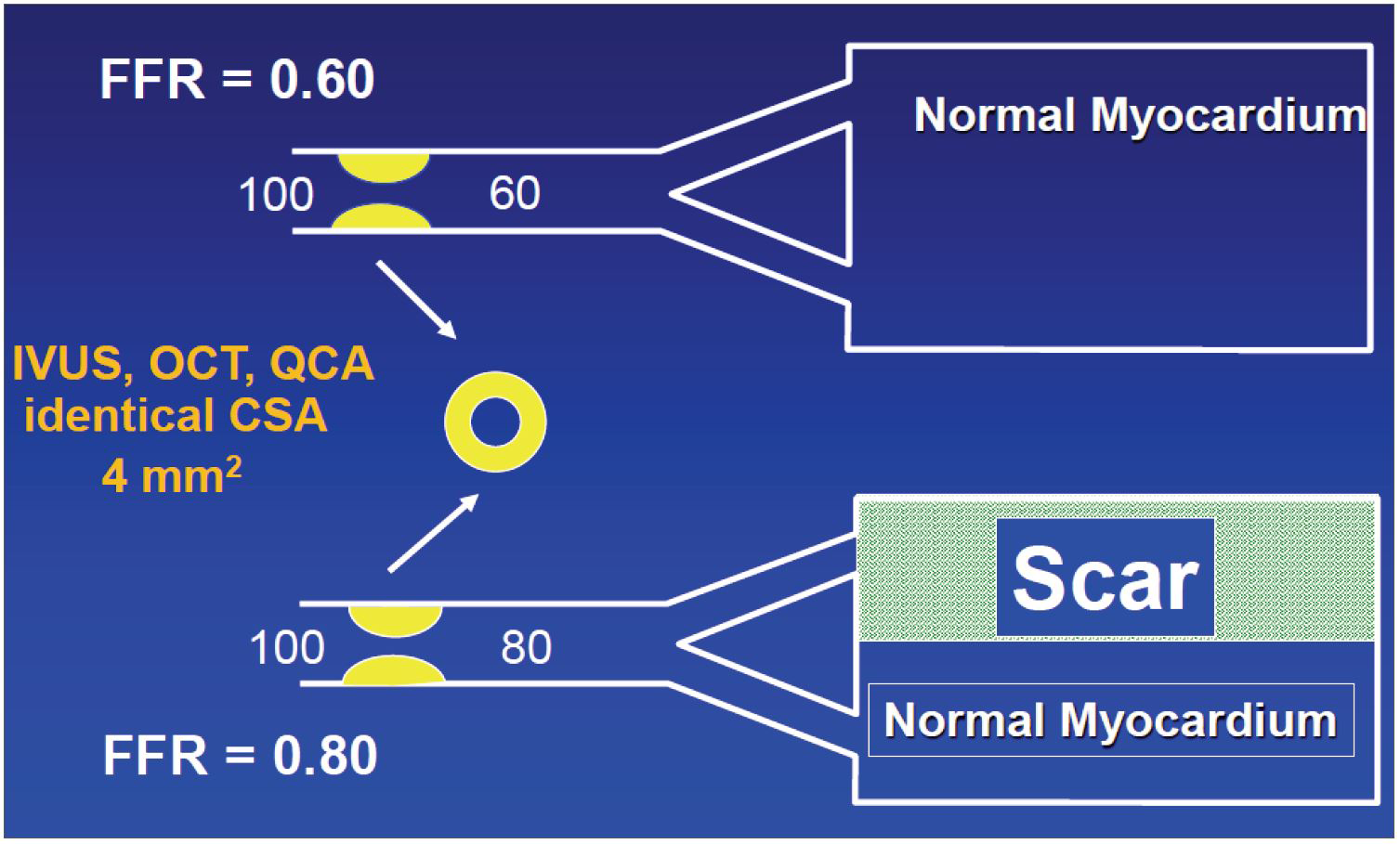
FFR has a sound scientific basis and experimental validation, is accurate and reproducible with an unequivocal normal value and a clear-cut-off with a narrow gray zone, and is easy to perform. FFR is the link amid stenosis severity, maximal blood flow, perfusion territory, and myocardial ischemia. FFR can assess the severity of many complex lesions and functional improvement after percutaneous coronary intervention (PCI) (Figure 1).
Numerous clinical trials have investigated the role of FFR-guided PCI in comparison with angiography alone, medical treatment, or coronary artery bypass grafting (CABG). For instance, the FAME trial showed lower stent use and lower major adverse cardiac events (MACE) in the FFR-guided PCI group compared to the angio-guided PCI group. The FAME-2 trial showed better clinical outcomes in the FFR-guided PCI group than in the medical therapy group. The FAME-3 trial demonstrated that FFR-guided PCI using current-generation drug-eluting stents (DES) did not meet the criteria for noninferiority compared with CABG among patients with angiographic three-vessel disease.
In conclusion, anatomy alone is insufficient to understand the physiologic significance of coronary artery disease. FFR provides superior insight into coronary pathophysiology and greatly improves the correct diagnosis of coronary artery disease. There is incontrovertible evidence for improved outcomes of coronary disease and revascularization by the systematic use of FFR.
Opening of TCTAP 2023 & Key Note Lectures
Sunday, May 07, 9:30 AM - 10:16 AM
Main Arena, Walker Hall, Level 1
Edited by
Yong-Hoon Yoon, MD
Ulsan City Hospital, Korea (Republic of)

