
Andrejs Erglis, MD
Pauls Stradins Clinical University Hospital, Latvia
The popularity of percutaneous coronary intervention (PCI) for the treatment of unprotected left main (ULM) lesions has increased in the past few years due to the advances in stent technologies and adjunctive pharmacotherapies. However, PCI of complex bifurcation lesions is still challenging in the drug-eluting stent (DES) era, and the results are worse compared with the simple coronary lesions.
Although the provisional stent (PS) strategy is generally considered as the default strategy for bifurcation lesions, there are scenarios in which the two-stent strategy is initially necessary to improve the patency of both the main branch and the side branch. Unfortunately, the high occurrence of in-stent restenosis (ISR) of the left circumflex artery (LCx) ostium is a major limitation of the 2-stent strategy for ULM lesion, with a recent study reporting that an ISR rate of 25.4% with this strategy (majority in the LCx ostium) versus a rate of 6.3% with a PS strategy.
Bioresorbable vascular scaffolds (BVS) has the unique ability to restore vascular physiology and anatomical integrity, such as native tortuosity and angulation, with only a temporary scaffold necessary to maintain the patency of the vessel after the intervention. Studies have shown a complete resorption of scaffold struts at five-years. Therefore, it may provide a novel way to treat ULM distal bifurcation lesions, that would benefit from a two-stent strategy at the time of intervention but leave nothing behind to preclude later surgical revascularization or noninvasive imaging.
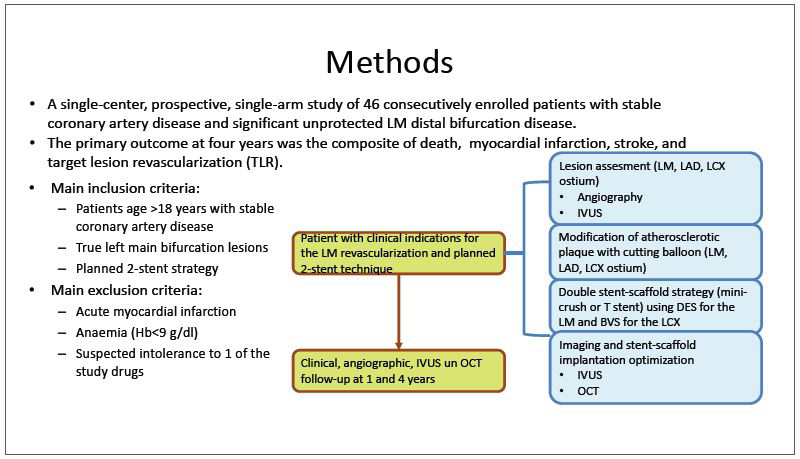
The study aimed to investigate the long-term outcomes of a two-stent strategy in patients with LM bifurcation lesions involving the ostium of the LCx artery, utilizing a DES in the LM extending into the left anterior descending artery (LAD) and a BVS in the LCx ostium (Figure 1). The primary outcome at four-years was the composite of deaths, myocardial infarction, stroke, and target lesion revascularization (TLR).
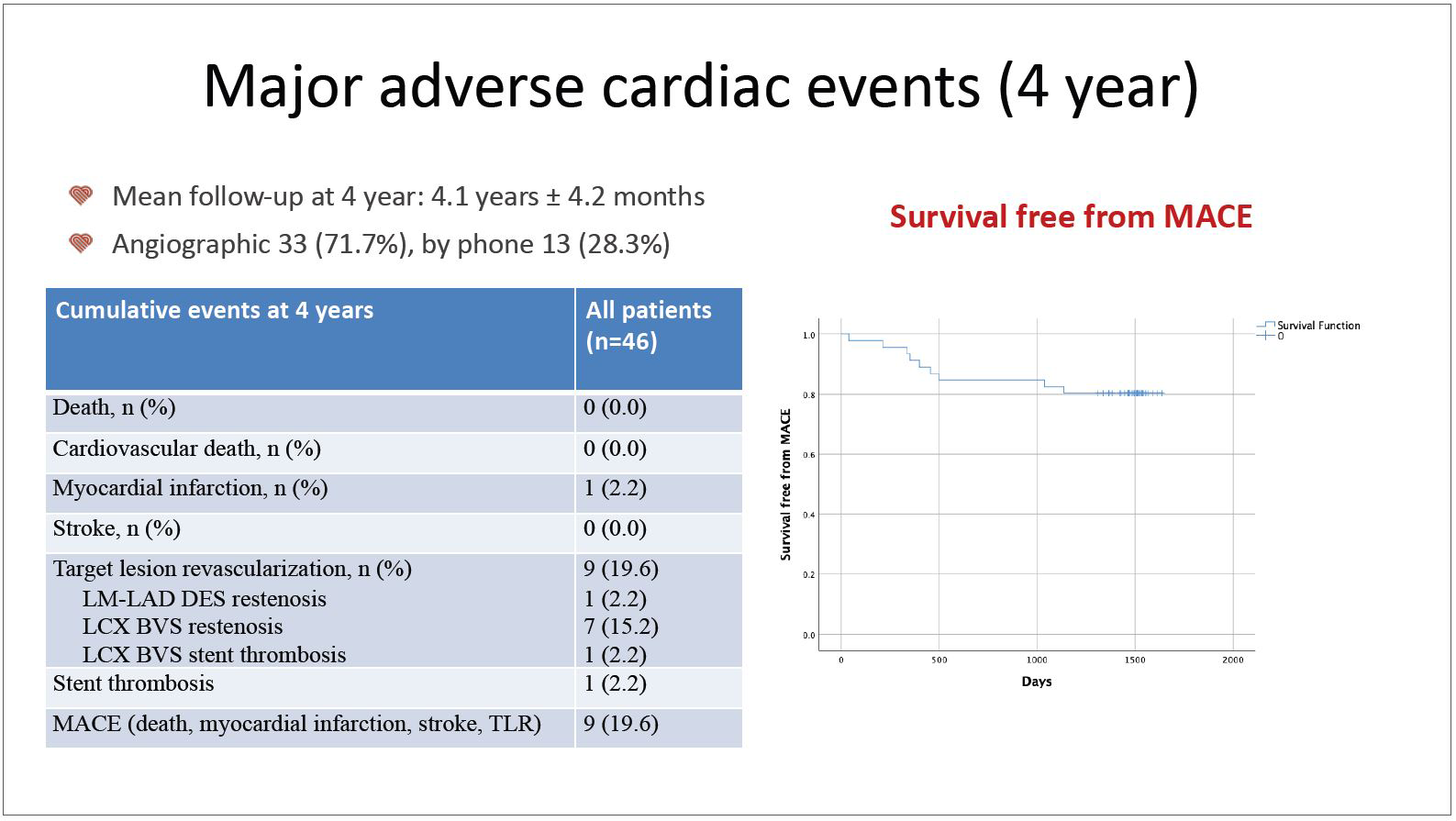
At four-years, the primary outcome was identified in nine patients (19.6%) (Figure 2). All events were TLRs except one myocardial infarction due to BVS thrombosis. Seven of the eight TLRs were a result of side branch BVS restenosis. Univariate predictors of the four-year outcome were higher LDL cholesterol and BVS size ≤2.5 mm. On multivariate analysis, LCx lesion preparation with a cutting balloon and post-procedure use of intravascular ultrasound for optimization was found to be independent protective factors of major adverse cardiovascular events (MACE).
In selected patients with LM distal bifurcation disease, an imaging-guided two-stent strategy with DES in the LM and BVS in the LCx ostium was technically successful in all patients and was reasonably safe and effective for four years.
Meet the Experts over Breakfast
All Bifurcation PCI
Monday, May 08, 7:00 AM - 08:00 AM
Presentation Theater 1, Vista 3, B2
Edited by

Cheol Hyun Lee, MD
Keimyung University Dongsan Medical Center, Korea (Republic of)

