Revascularization and adjunctive strategies: beyond the ESC guidelines.

Adrian P. Banning, MD
Oxford University Hospitals NHS Foundation Trust, UK
With all the remarkable advancements in percutaneous coronary intervention (PCI) and adjunctive pharmacotherapy, the mortality following acute myocardial infarction (MI) has declined over the past decades. The management of MI is one of the most impressive successes of evidence-based medicine, effectively decreasing the incidence of cardiovascular mortality from >40% in the early 1950s to <10% today. However, we have reached a plateau in the improvement of clinical outcomes following MI.
Microvascular obstruction (MVO) is a common complication following primary PCI in patients with MI, and it can have significant negative effects on patient outcomes (Figure 1).
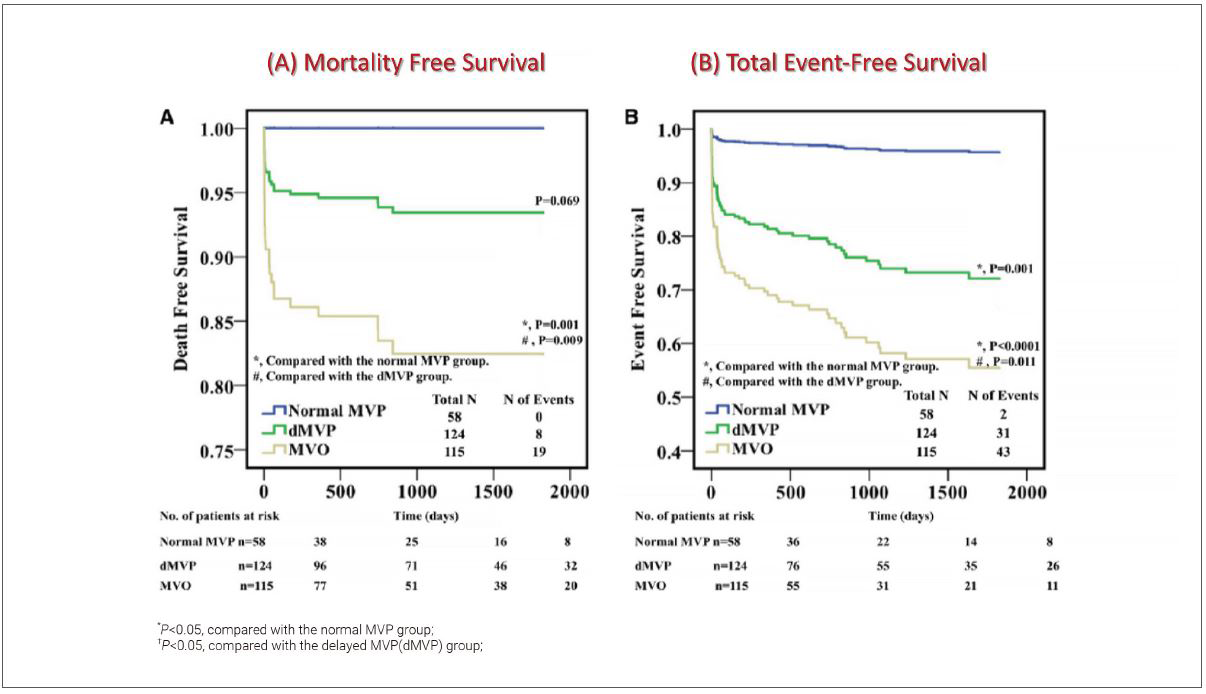
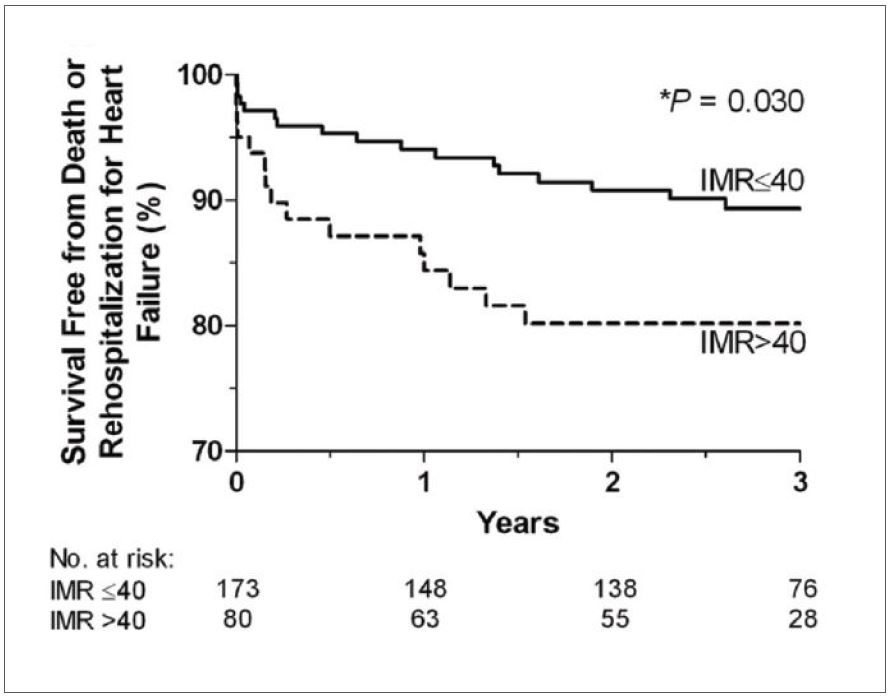
MVO occurs when there is impaired blood flow through the microvessels in the infarct zone, leading to reduced myocardial salvage and increased infarct size, even in patients with successful reperfusion. This is important because the size of the infarct is a predictor of adverse events, such as heart failure and death. An elevated index of microcirculatory resistance (IMR) reflects microvascular function, and when measured after primary PCI it can predict an adverse clinical outcome (Figure 2).
Based on previous report, improved perfusion of the myocardium measured by IMR during primary PCI is not universal. Approximately one-third of patients presenting with ST-elevation myocardial infarction (STEMI) still have limited improvement or have worsened perfusion despite stenting. Therefore, the aim of MI treatment would be not only to achieve successful reperfusion of the occluded artery with primary PCI but also to ensure adequate microvascular perfusion in the infarct zone. In addition to standard therapy for MI, different therapeutic interventions have been investigated for improving microvascular perfusion. These interventions include vasodilators, glycoprotein IIb/IIIa inhibitors, and mechanical thrombectomy devices. Besides these, several therapeutic interventions are considered to minimize ischemia-reperfusion injury. He will introduce several novels and exciting therapies that could improve outcomes in primary PCI. These include relatively novel strategies, such as myocardial cooling, left ventricular unloading, supersaturated oxygen (SSO2), and pressure-controlled intermittent coronary sinus occlusion (PICSO). In this presentation, the PISCO therapy is more focused. The PICSO therapy is designed to reduce reperfusion injury by intermittently occluding the coronary sinus, which drains blood from the heart, and delivering pressure-controlled pulses of saline into the coronary venous system. This creates a retrograde flow that helps to flush out any debris and microthrombi that may have accumulated during the blockage, improving microcirculatory flow and tissue perfusion. Several studies have suggested that PICSO therapy can improve myocardial perfusion and reduce infarct size, which could lead to better clinical outcomes for patients with MI. Trials on these novel strategies are ongoing.
Meet the Experts over Breakfast
Acute Coronary Syndrome
Sunday, May 07, 7:00 AM - 8:00 AM
Art Hall, Level 4
Edited by

Sang Woo Park, MD
Konkuk University Medical Center, Korea (Republic of)

