
David Joel Cohen, MD
Cardiovascular Research Foundation, USA
For decades, coronary artery bypass grafting (CABG) has been the standard choice of revascularization for significant left main coronary artery (LMCA) disease. However, with remarkable advancements in device technology and adjunctive pharmacology, percutaneous coronary intervention (PCI) offers a more expeditious approach with rapid recovery and is a safe and effective alternative in appropriately selected patients with LMCA disease. Several landmark randomized clinical trials (RCTs) have shown that PCI with drug-eluting stents for LMCA disease is a safe option with similar long-term survival rates to CABG surgery, especially in those with low and intermediate anatomic risk.
Should CABG be preferred for most patients?
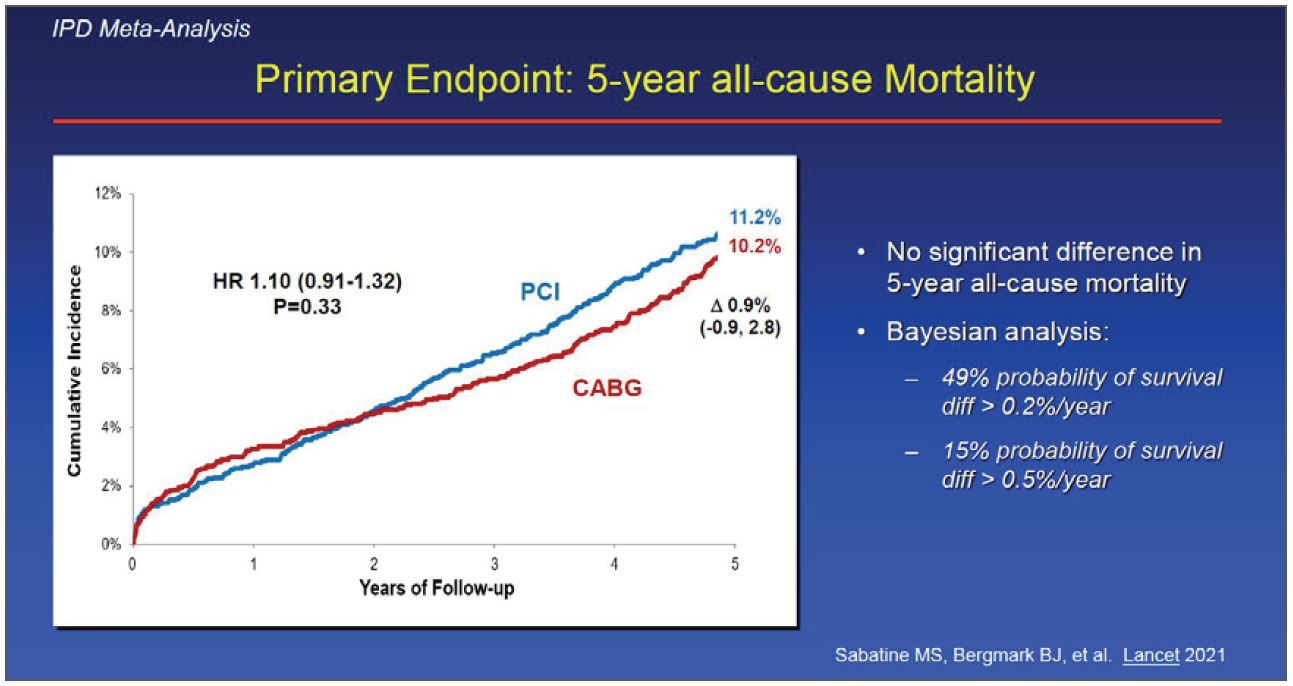
The most recent individual patient-level meta-analysis incorporating long-term follow-up results from key RCTs (SYNTAX, PRECOMBAT, NOBLE, and EXCEL trials) showed no statistical difference in 5-year all-cause death between PCI and CABG, although a Bayesian approach suggested a difference probably exists favoring CABG (Figure 1). Spontaneous myocardial infarction and repeat revascularization were more common with PCI than with CABG. Overall, there was no difference in the risk of stroke between PCI and CABG, but the risk was lower with PCI in the first year after randomization. A Heart Team approach to communicate expected outcome differences might be useful to assist patients in reaching a treatment decision.
Role of mechanical circulatory support
If the Heart Team decides to proceed with PCI as a revascularization method, several technical aspects of the PCI strategy should be considered to optimize PCI outcomes. Left main PCI should be performed as much as possible by experienced operators in catheterization laboratories with intracoronary imaging, invasive coronary physiology, and mechanical circulatory support (MCS). MCS use remained low but increased from 0.2% to 0.6% of high-risk elective PCIs between 2007 and 2017, and unprotected left main PCI was the main high-risk feature associated with prophylactic MCS use. Patients with normal left ventricular function rarely require planned MCS. When the left main anatomy is complex (distal bifurcation lesion, severe calcification requiring atheroablation) and cardiac reserve is limited (ejection fraction <30%, pulmonary capillary wedge pressure >30 mmHg), MCS should be considered for unprotected left main PCI.
1-stent vs. 2-stent strategies
An up-front 2-stent strategy for bifurcation lesions has been deemed inferior to provisional stenting; nevertheless, the optimal stent strategy for LMCA bifurcation lesions remains unknown. The DKCRUSH-V trial demonstrated that PCI for true distal LMCA bifurcation lesions using a planned double-kissing crush 2-stent strategy resulted in a lower rate of target lesion failure at 1 year than the provisional stenting strategy. In contrast, the EBC-MAIN trial demonstrated that the stepwise layered provisional approach was associated with numerically fewer major adverse cardiac events than planned dual stenting. Currently, the initial single-stent crossover and provisional side branch approach is recommended for LMCA bifurcation lesions. However, the choice of strategy should be based on angiographic features (vessel size, side branch involvement, lesion length), as well as operator expertise. A more detailed evaluation of the anatomic severity can be obtained by intracoronary imaging, which is essential for pre-interventional lesion assessment and post-interventional stent optimization.
TCTAP Workshops
LM & Multi-Vessel Diseases and Bifurcation & CTO After ISCHEMIA Study
Saturday, May 6, 10:30 AM ~ 12:30 PM
Valve & Endovascular Theater, Vista 1, B2
Edited by

Ju Hyeon Kim, MD
Asan Medical Center, Korea (Republic of)

