Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-204
When the Clips Become a Hero Twice
By Krissada Meemook, Donluck Poonkasem
Presenter
Donluck Poonkasem
Authors
Krissada Meemook1, Donluck Poonkasem2
Affiliation
Ramathibodi Hospital Mahidol University, Thailand1, Ramathibodi Hospital, Thailand2,
View Study Report
TCTAP C-204
STRUCTURAL HEART DISEASE - Valvular Intervention: Mitral or Tricuspid
When the Clips Become a Hero Twice
Krissada Meemook1, Donluck Poonkasem2
Ramathibodi Hospital Mahidol University, Thailand1, Ramathibodi Hospital, Thailand2,
Clinical Information
Patient initials or Identifier Number
3802322
Relevant Clinical History and Physical Exam
A 92-year-old woman had underlying diseases of AF with SSS on a dual-chamber pacemaker, HT, and DLP. In the past 3 years, she had progressive dyspnea on exertion and was treated with M-TEER for severe MR. After a successful procedure, her clinical symptoms improved. Recently, she revisited the HF clinic with recurrent dyspnea and peripheral edema. Neck vein engorgement and pan-systolic murmur along left parasternal border were noticed. Severe TR was believed to be the key problem at this time.
Relevant Test Results Prior to Catheterization
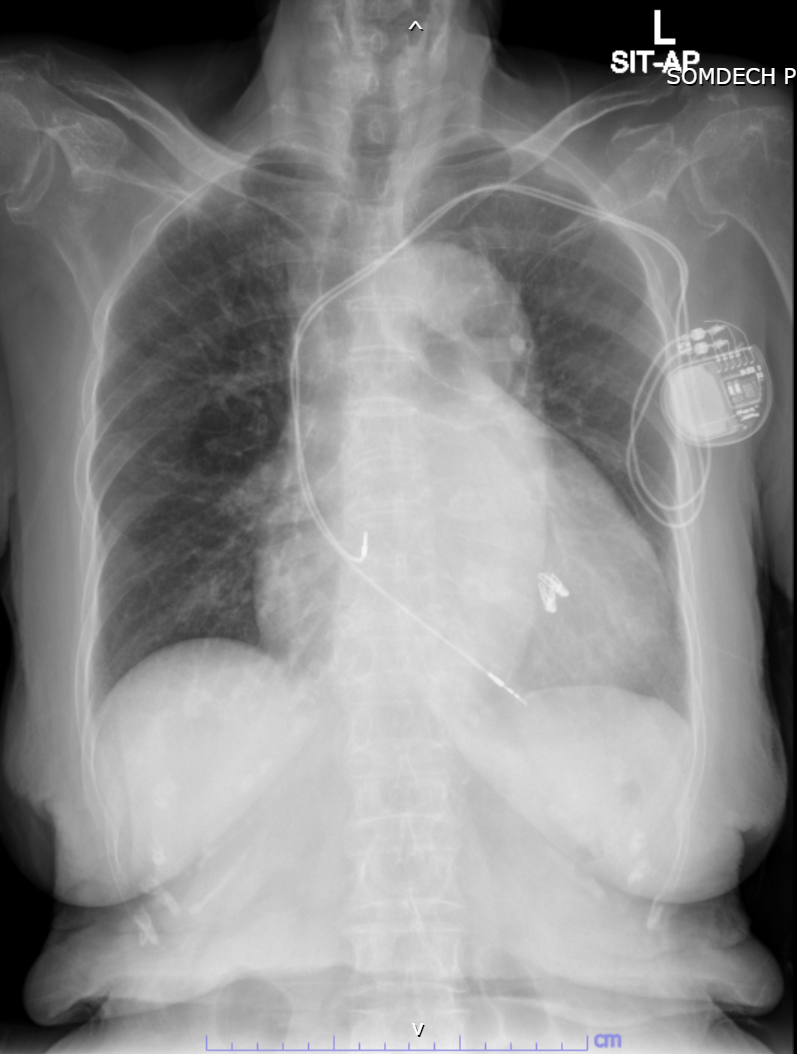
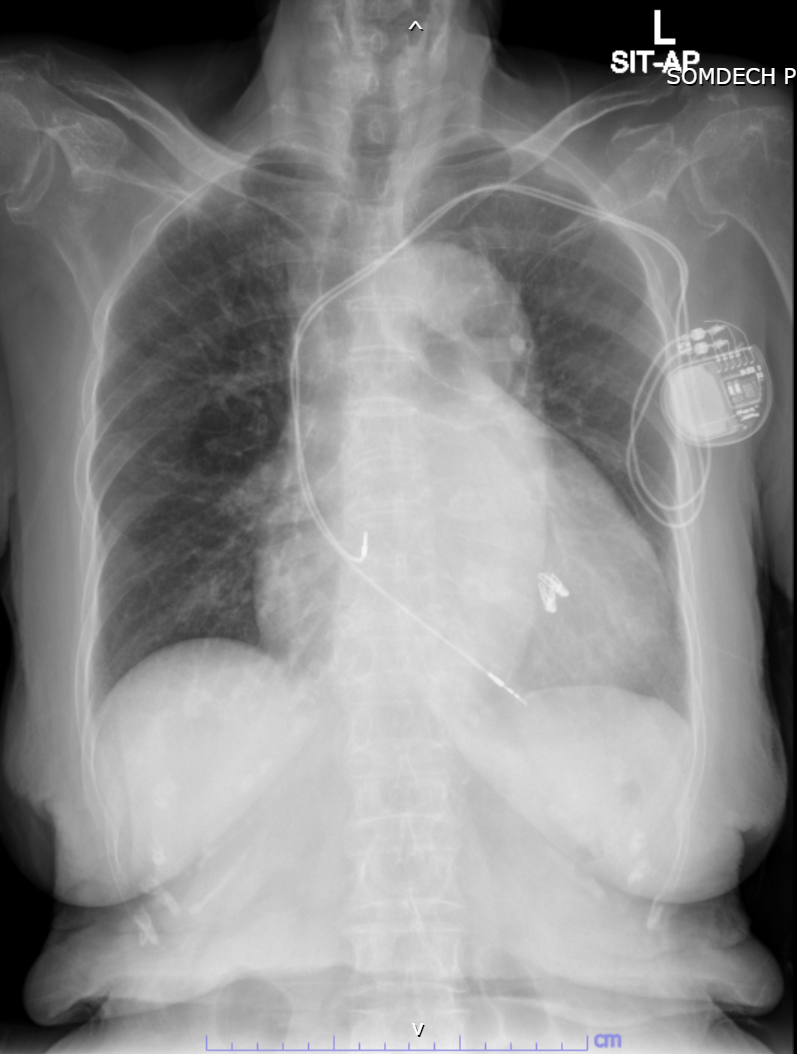
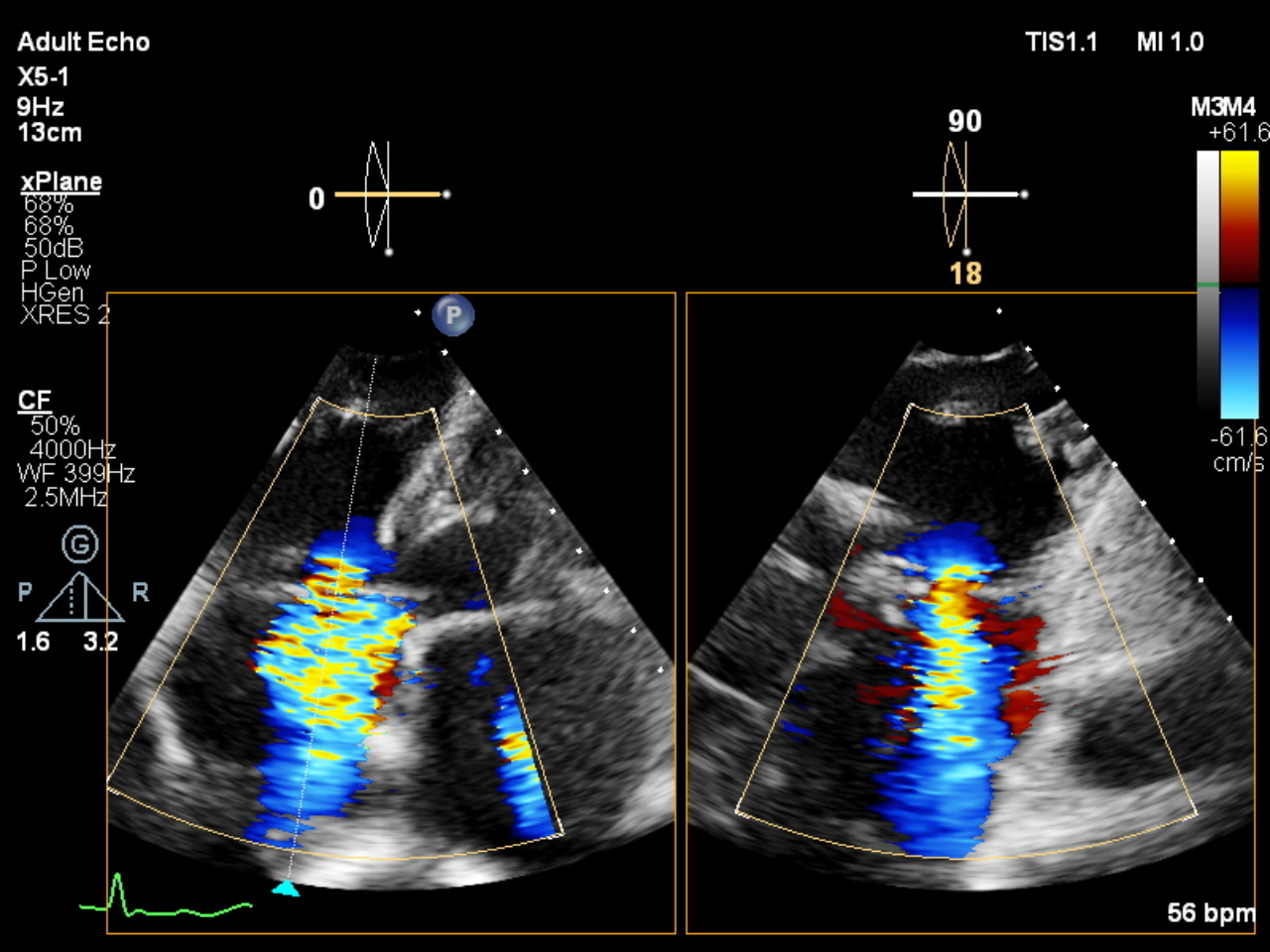
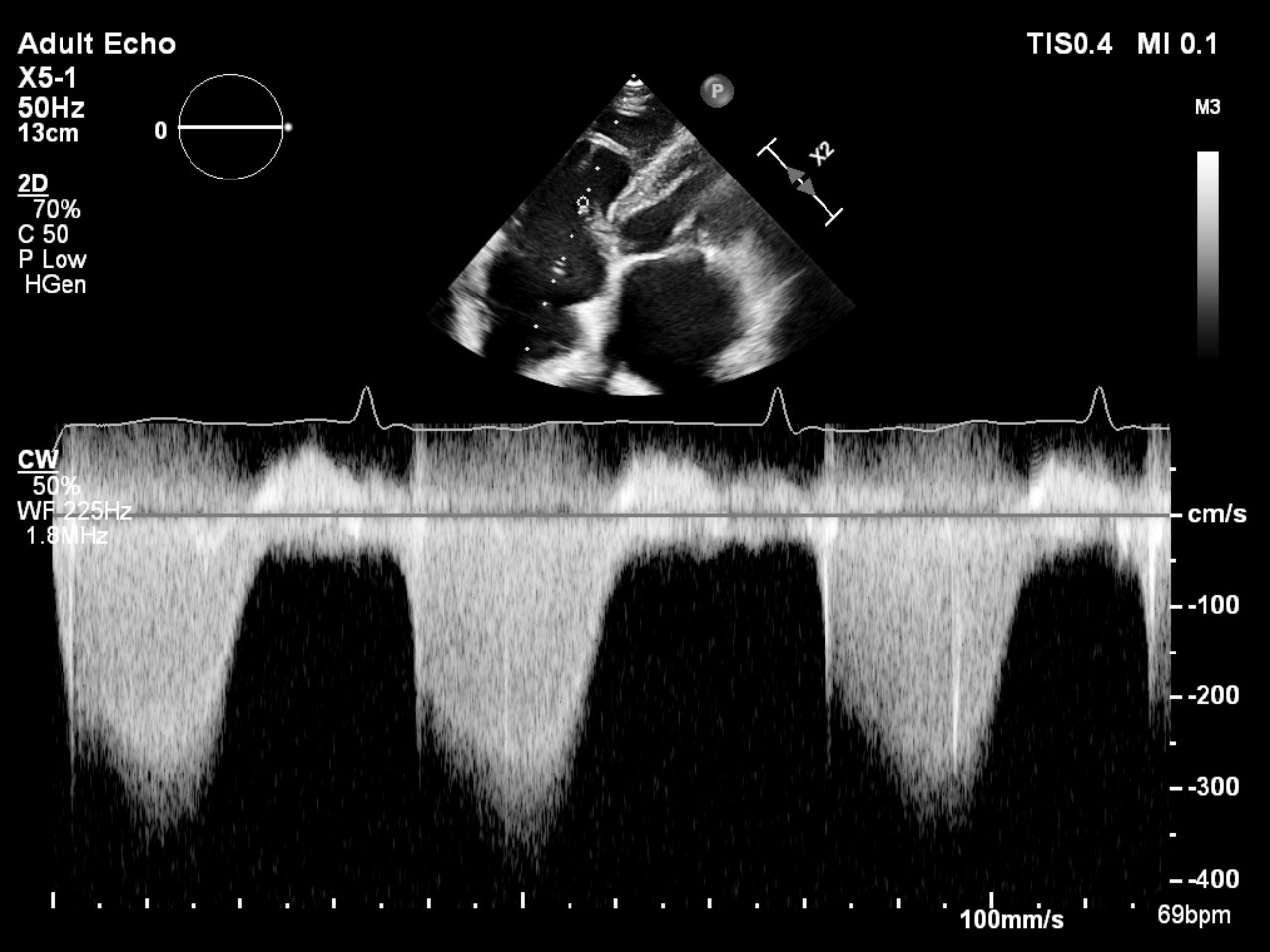
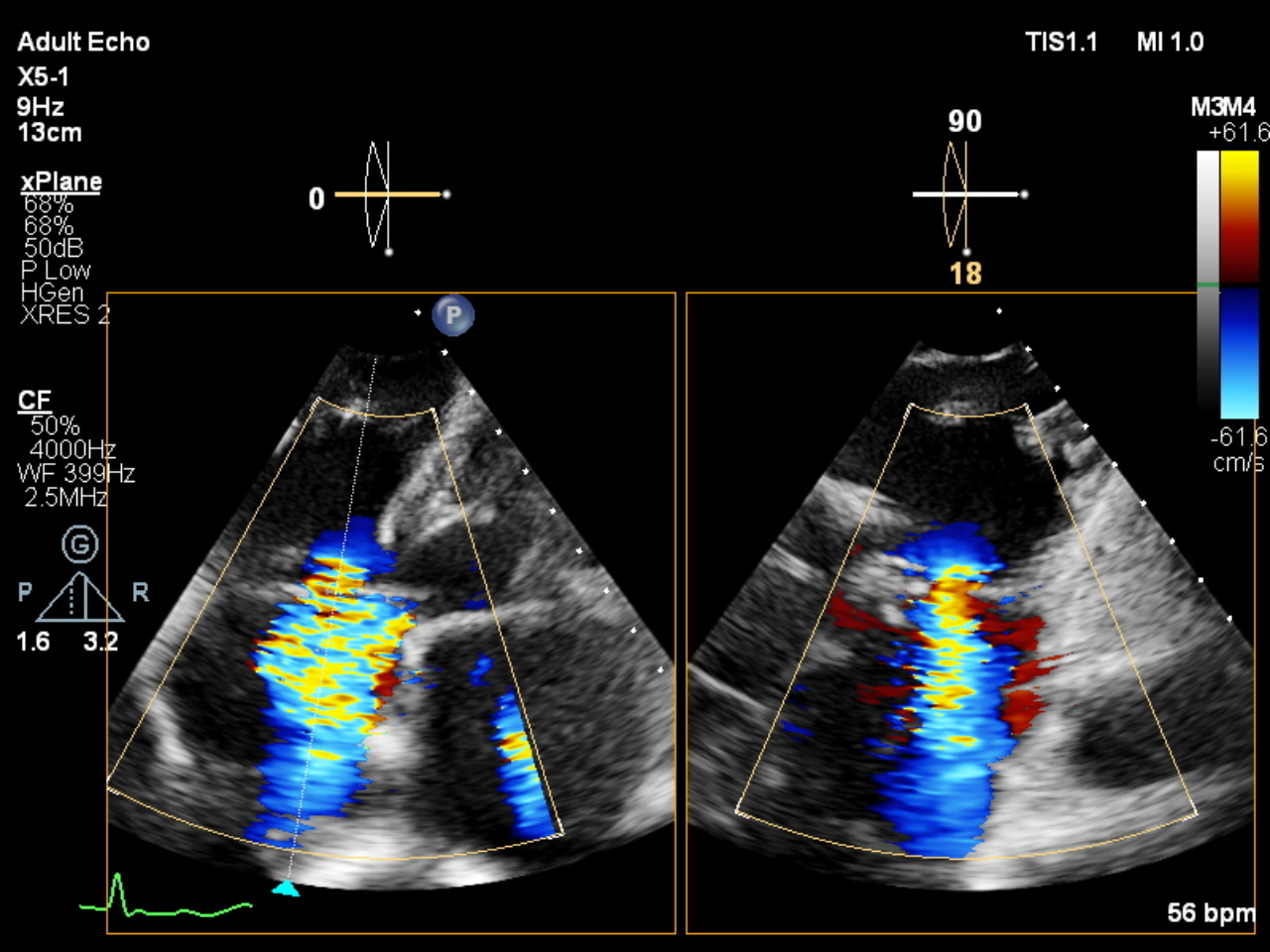
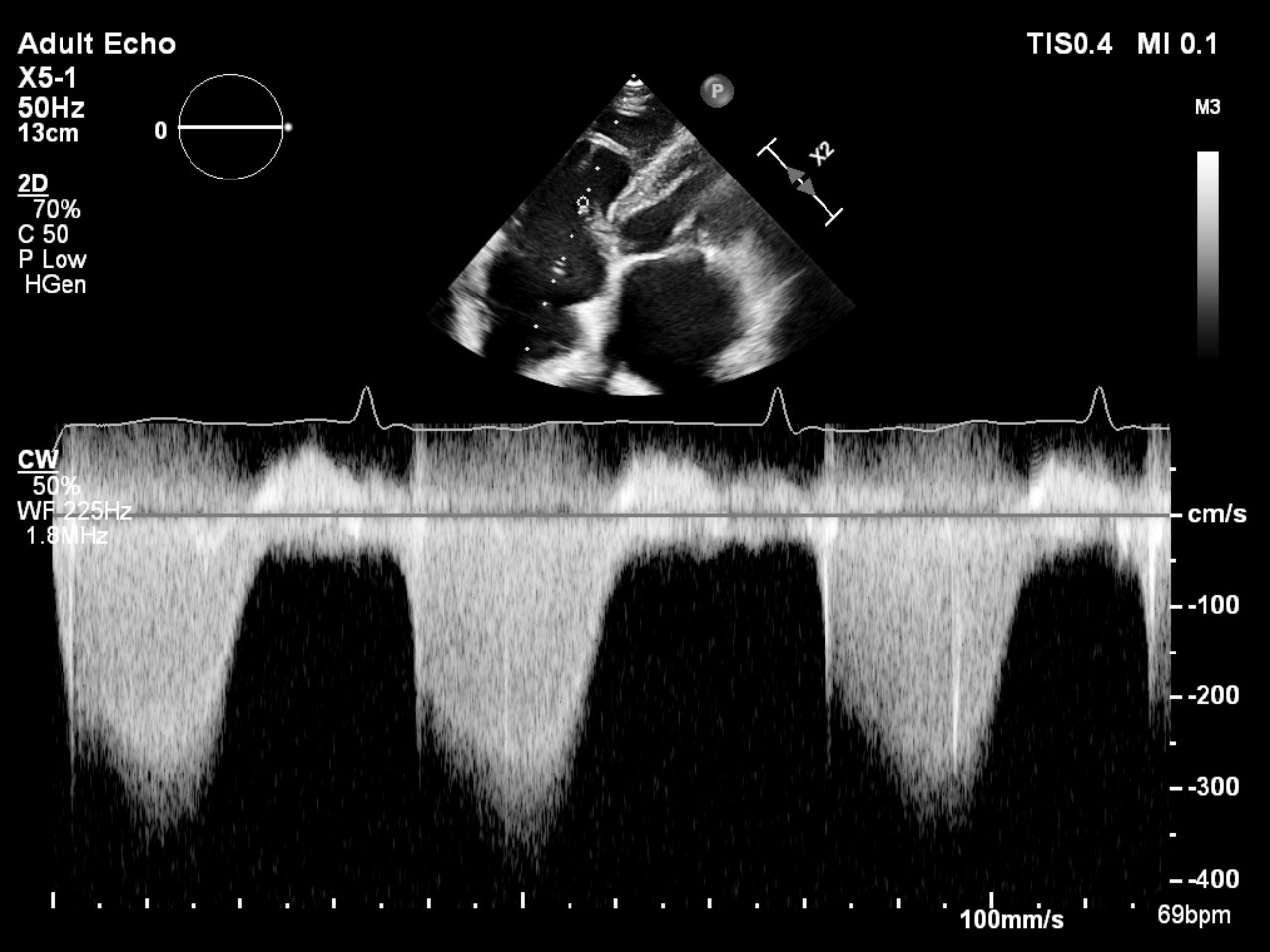
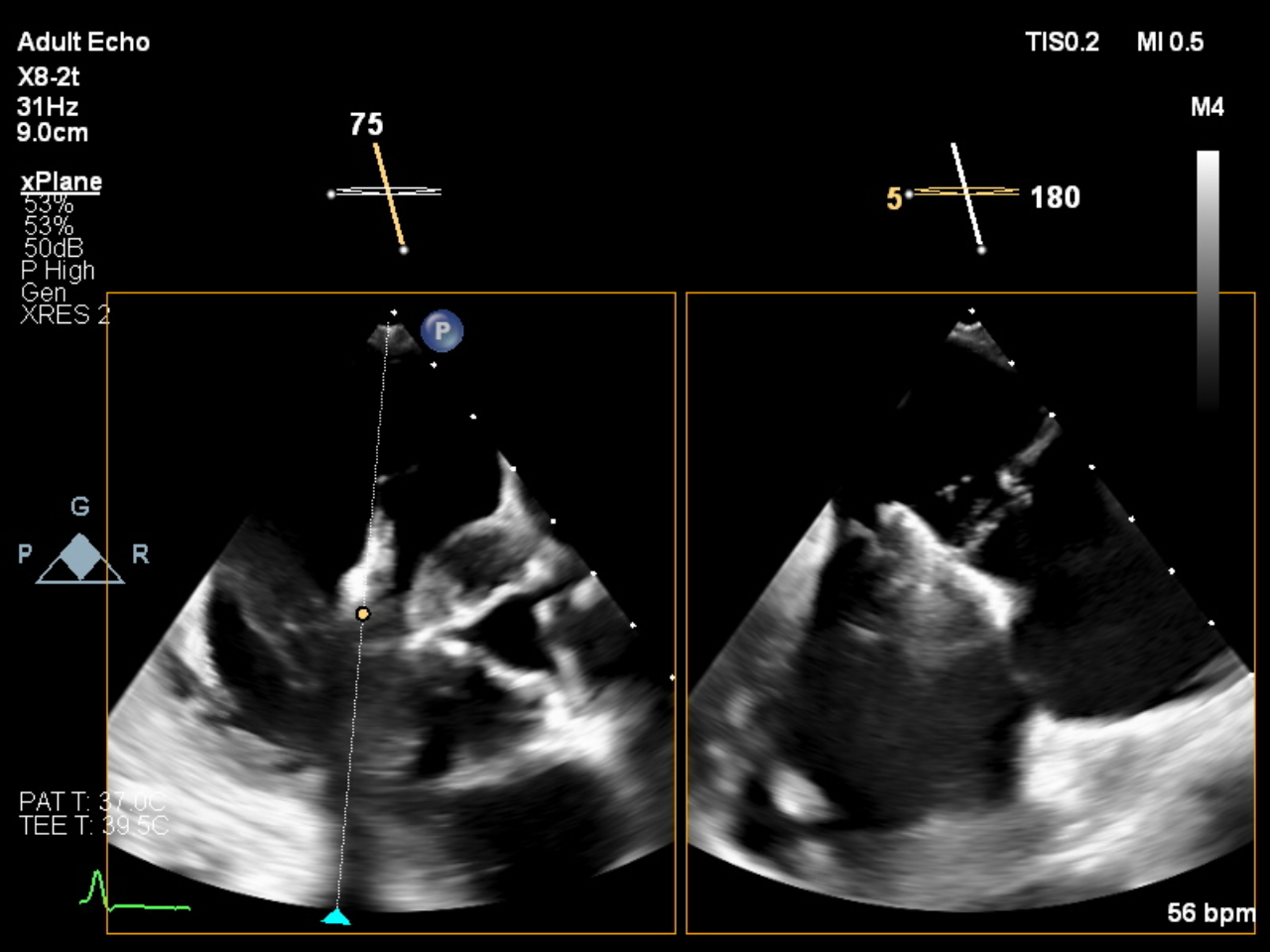
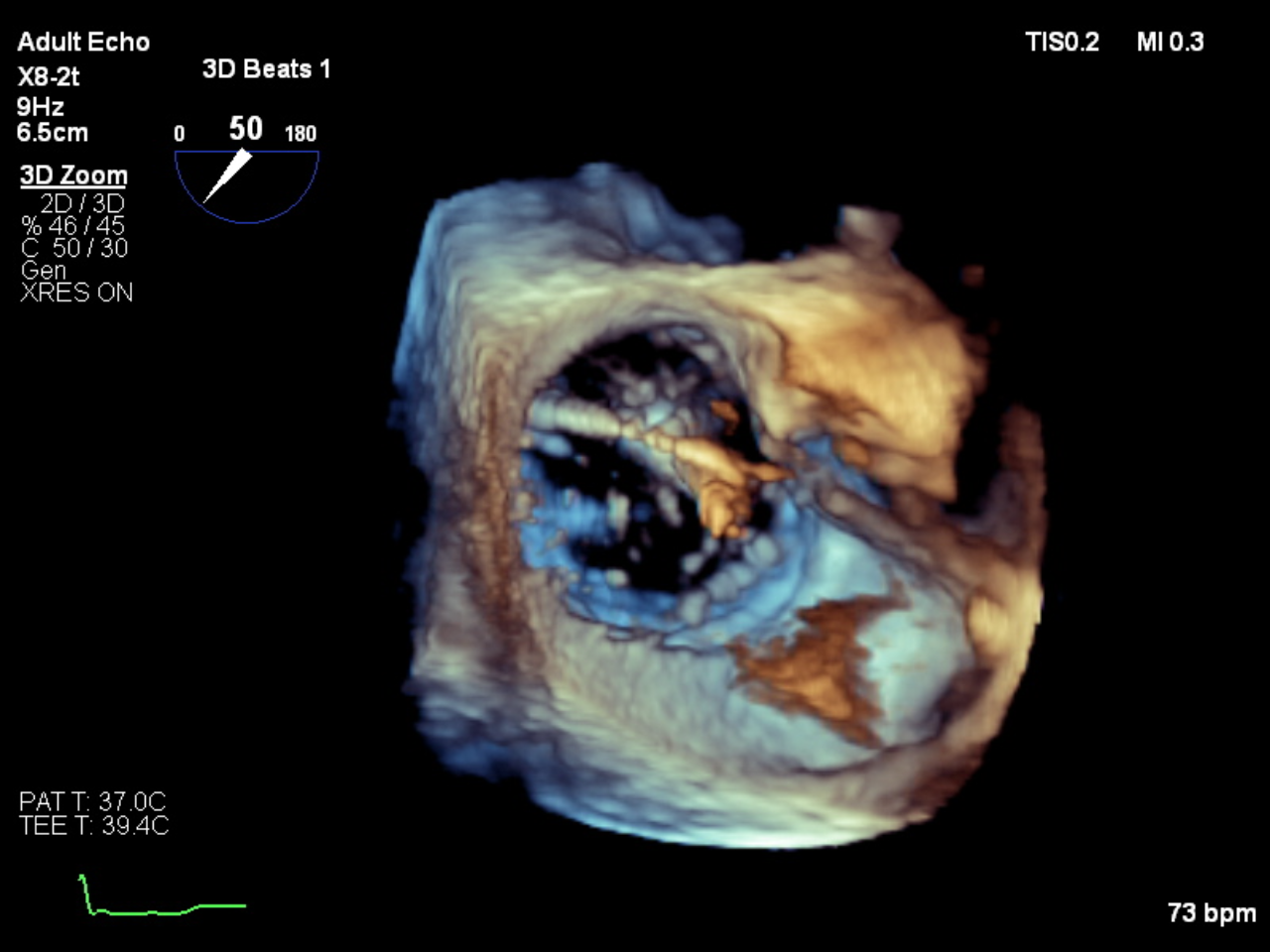
TTE showed severe LA and RA dilation, normal LV systolic function (LVEF 62%) and normal RV systolic function. There is mild residual MR with two well-seated MitraClips (mean PG of 4 mmHg). But there is severe TR (VC 1.1 cm), which is suspected from pacemaker lead impingement and mild PH (RVSP 38 mmHg). TEE showed severe functional TR due to non-coaptation of the septo-anterior tricuspid leaflets, in contrast to the postero-septal commissure where the pacemaker lead is implanted, causing mild TR.
Relevant Catheterization Findings
Right heart catheterization showed giant V wave with RAP 14 mmHg, mean PAP 27 mmHg, PCWP 21 mmHg, PVR 1.8 WU, and CO 4.5 L/min.
Interventional Management
Procedural Step
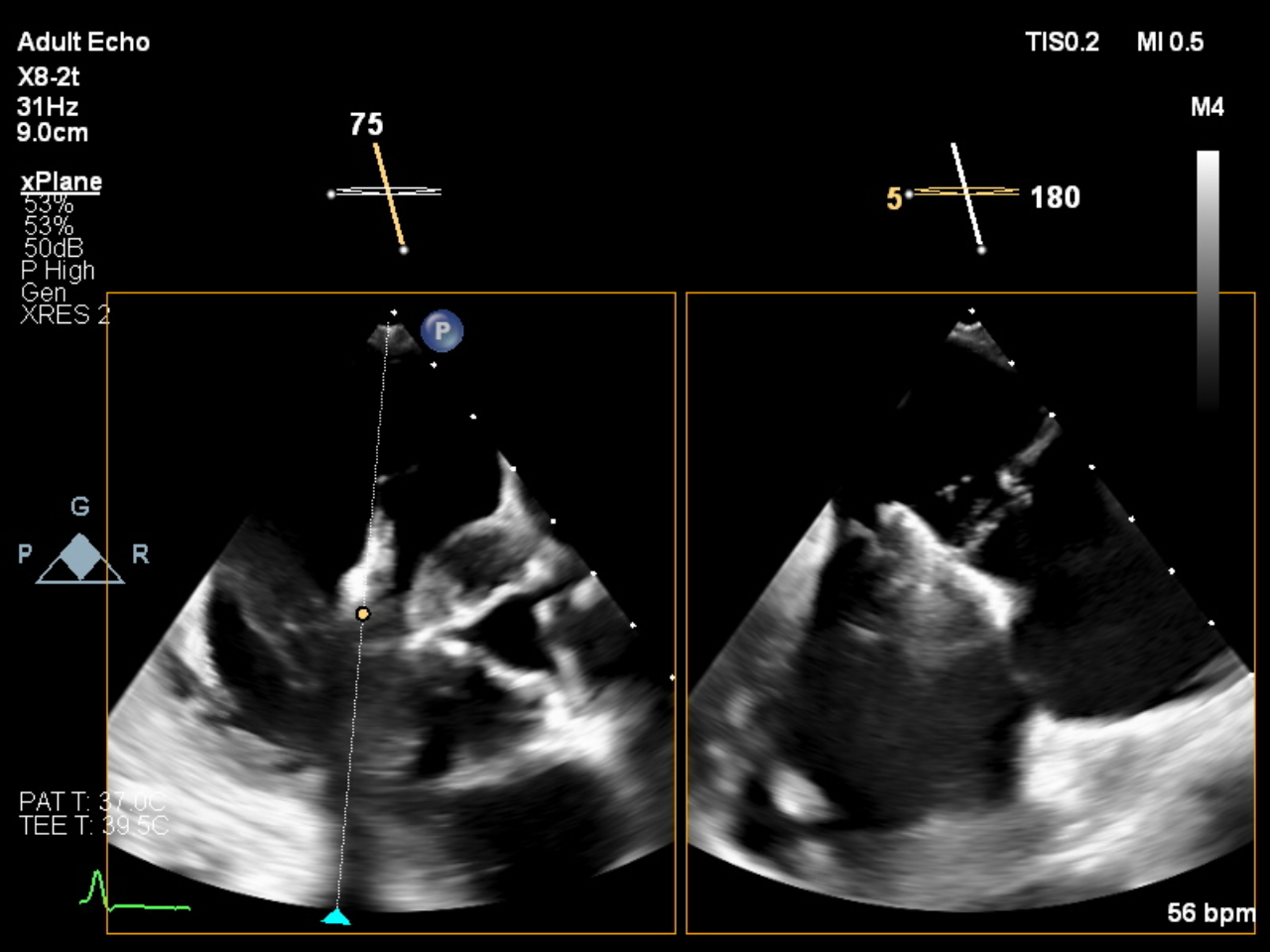
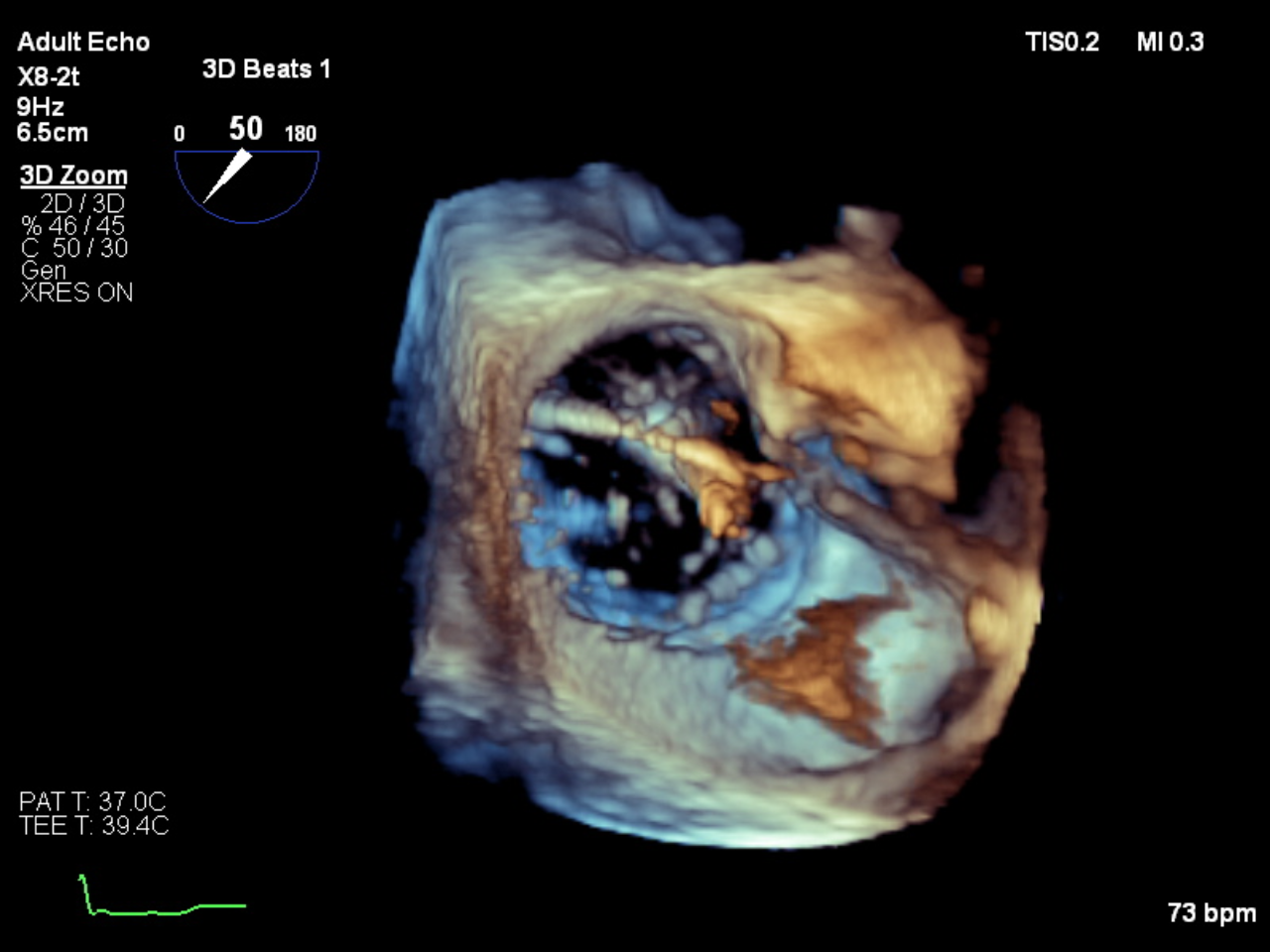
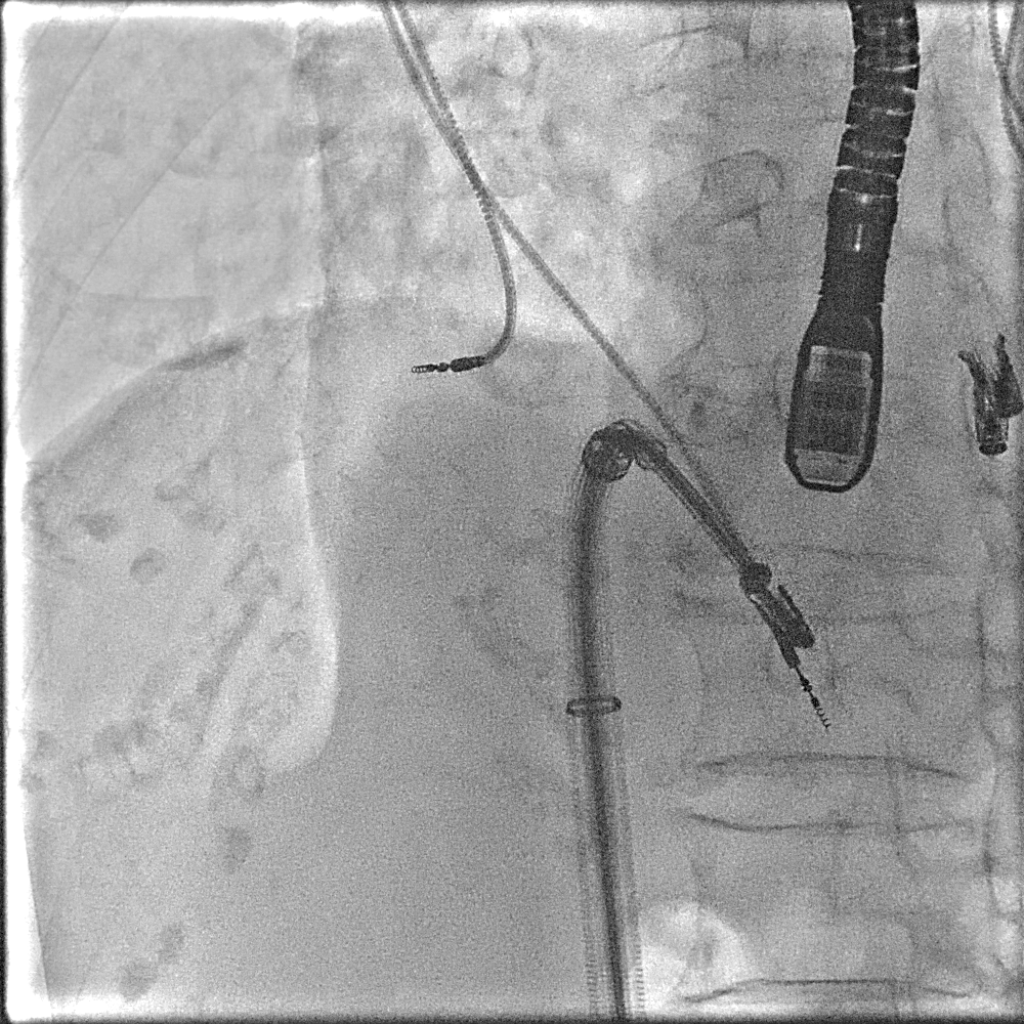
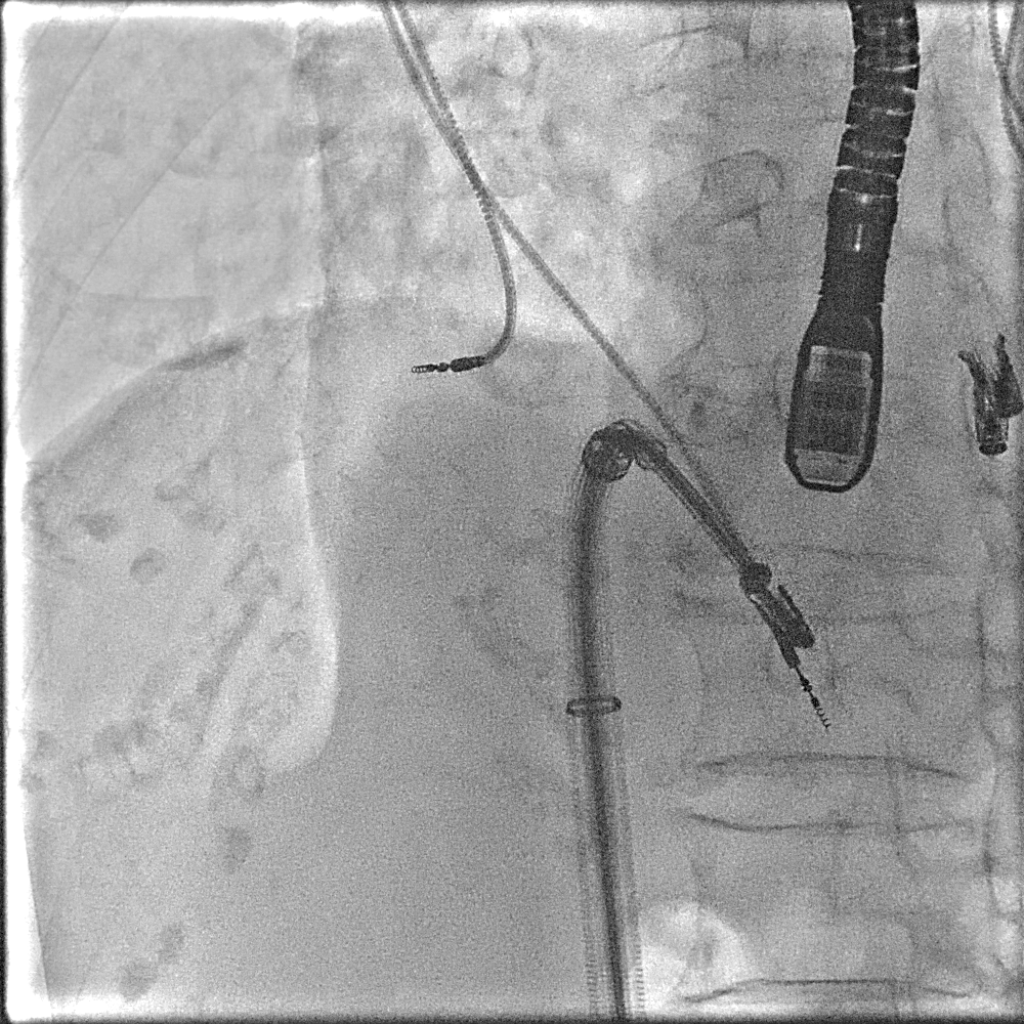
- General anesthesia was performed by the anesthesiologist.- The patient was given 1 gram of Cefazolin IV for prophylaxis.- A 7F Swan-Ganz catheter was inserted through the right internal jugular vein to measure hemodynamics. TEE probe was inserted at mid esophageal level.- Under local anesthesia, the Proglide device was used to gain venous access at the right femoral vein using a pre-close suture technique, followed by the insertion of an 8F sheath.- The 6MP catheter, which was inserted with 0.035" Amplatz super stiff guidewire, was cannulated into the right atrium, and then the 6MP catheter was removed.- The TriClip XTw steerable guiding catheter was inserted over the Amplatz wire and placed in the right atrium.- The TriClip XTw was prepared as usual and carefully advanced through the device deployment sheaths into the right atrium under fluoroscopy and TEE guidance.- After optimizing the position of the device, the Triclip XTw was deployed under TEE and fluoroscopy guidance.- TEE showed a well-seated clip that attached the anterior and septal leaflets. The clip was successfully released in the usual fashion.- TEE examination revealed a reduction in the degree of TR from severe to mild, with a mean TV gradient of 1 mmHg.- The Triclip steerable guide catheter was withdrawn from the body and venous hemostasis was achieved by proceeding with preclosure suture. - RAP slightly increased from 8 to 11 mmHg.
Case Summary
A 92-year-old woman who had previously experienced exertional dyspnea due to severe MR and had it corrected with MitraClips presented with recurrent progressive dyspnea. The cause of dyspnea this time was severe atrial functional TR. Due to the high risk of cardiac surgery, we decided to perform TriClip under TEE and fluoroscopy for reduction of TR severity and clinical symptoms. The Tricuspid Clip was successful in implantation; after that, her symptoms improved, and finally, she never came to the emergency department with recurrent dyspnea again.


