Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-075
Retrograde Kissing Wire Marker as a Plan B of Antegrade CTO Procedure
By Dafsah Arifa Juzar, Deo Idarto
Presenter
Deo Idarto
Authors
Dafsah Arifa Juzar1, Deo Idarto2
Affiliation
National Cardiovascular Center Harapan Kita, Indonesia1, Soewandhie Academic General Hospital, Indonesia2,
View Study Report
TCTAP C-075
CORONARY - Chronic Total Occlusion
Retrograde Kissing Wire Marker as a Plan B of Antegrade CTO Procedure
Dafsah Arifa Juzar1, Deo Idarto2
National Cardiovascular Center Harapan Kita, Indonesia1, Soewandhie Academic General Hospital, Indonesia2,
Clinical Information
Patient initials or Identifier Number
AP
Relevant Clinical History and Physical Exam
A 57 years old male was planned for elective PCI CTO in RCA with J-CTO score 2 and Werner score CCS 2 . His risk factor is hypertension, had CABG X2 ( LIMA-LAD, SVG-PL) 3 years prior to admission. He presented with stable angina pectoris CCS II and graft failure in SVG-PL. His physical examination is normal, and hemodinamically stable.
Relevant Test Results Prior to Catheterization
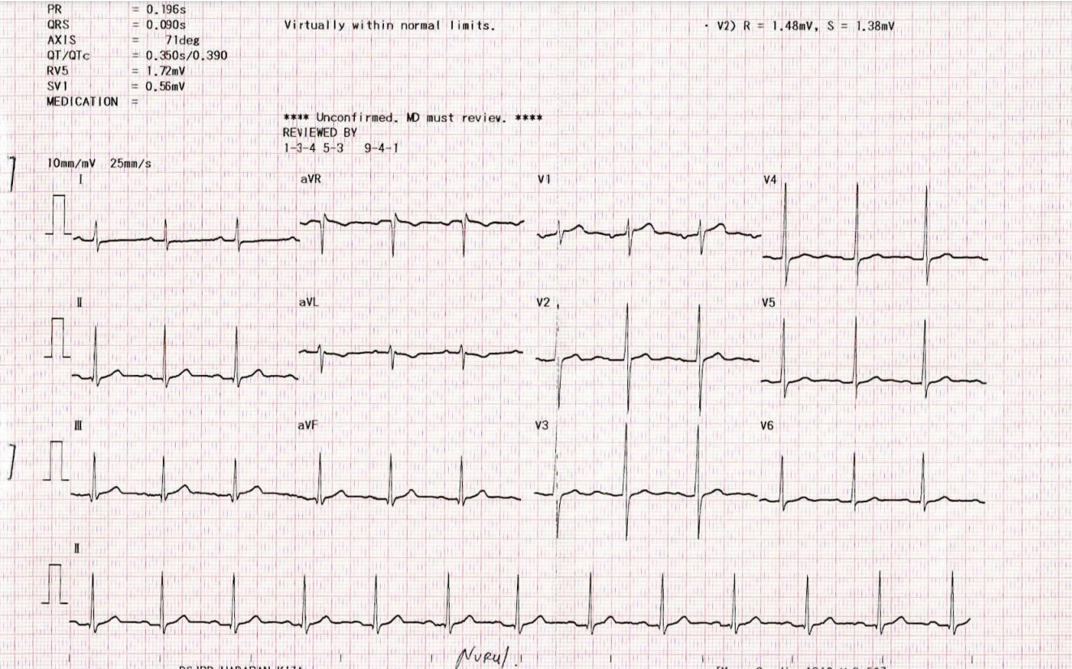
ECG: Normal Sinus Rhythm with slight T inversion in lead AVL
Echocardiography: LVEF (teich) : 57% with Regional Wall Motion Abnormality seen at basal-mid inferior and slightly decrease RV function ( TAPSE 1.6 cm)
Blood Investigation: Hb: 14.7 g/dL Platelet: 281.000 Ureum: 30.5 mg/dL Creatinine: 1.08 mg/dL
Echocardiography: LVEF (teich) : 57% with Regional Wall Motion Abnormality seen at basal-mid inferior and slightly decrease RV function ( TAPSE 1.6 cm)
Blood Investigation: Hb: 14.7 g/dL Platelet: 281.000 Ureum: 30.5 mg/dL Creatinine: 1.08 mg/dL
Relevant Catheterization Findings
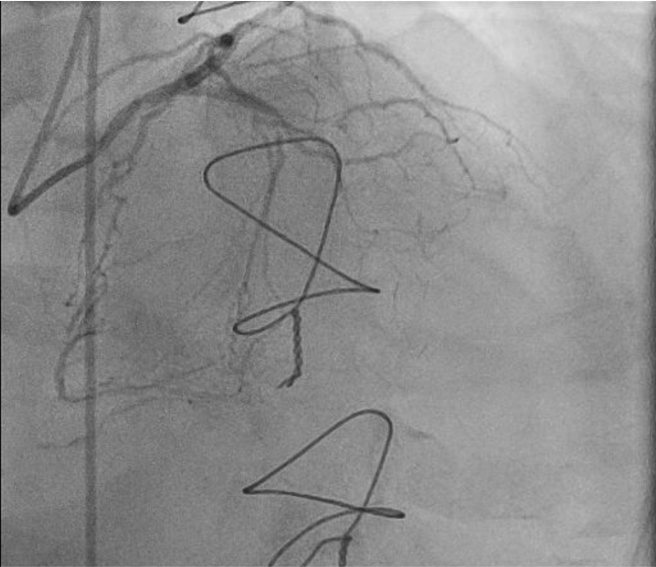
Coronary Angiography findings: Native Vessel:Left Main: normalLAD: CTO at proximal with bridging collateral LCx: Tubular stenosis 80-90% at distalRCA: CTO at mid with collateral bridging, distal filling from ipsilateral and contralateral ( Rentrop II )
Graft Vessel:LIMA-LAD : Graft patent SVG-PLB: Total occlusion at osteal
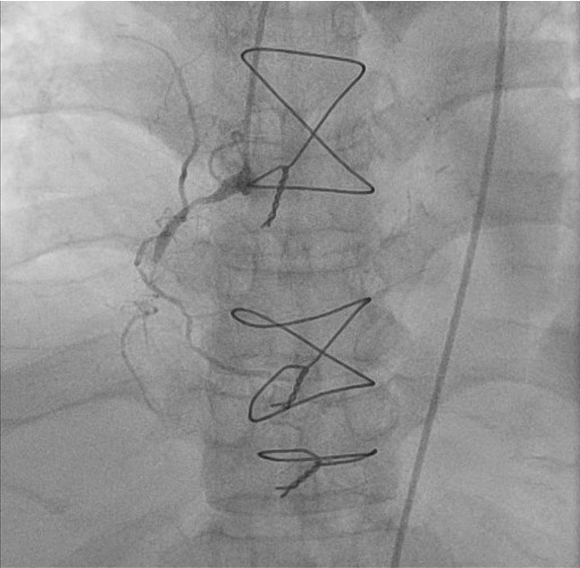
Graft Vessel:LIMA-LAD : Graft patent SVG-PLB: Total occlusion at osteal
Interventional Management
Procedural Step
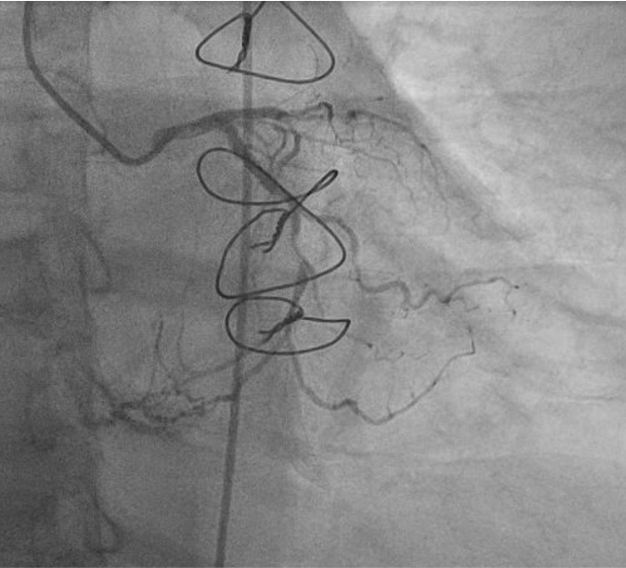
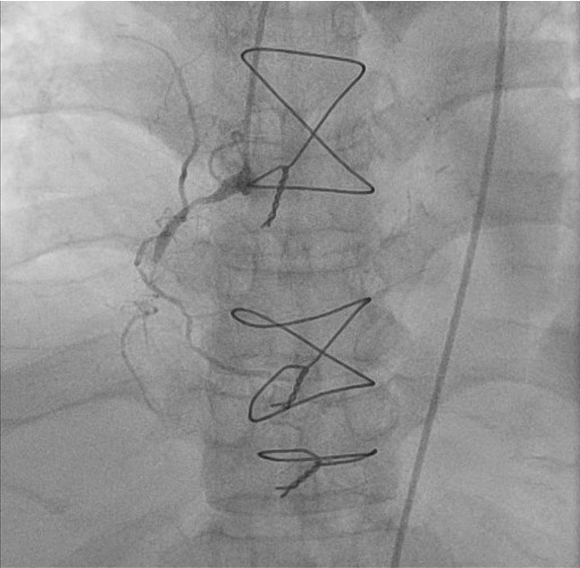
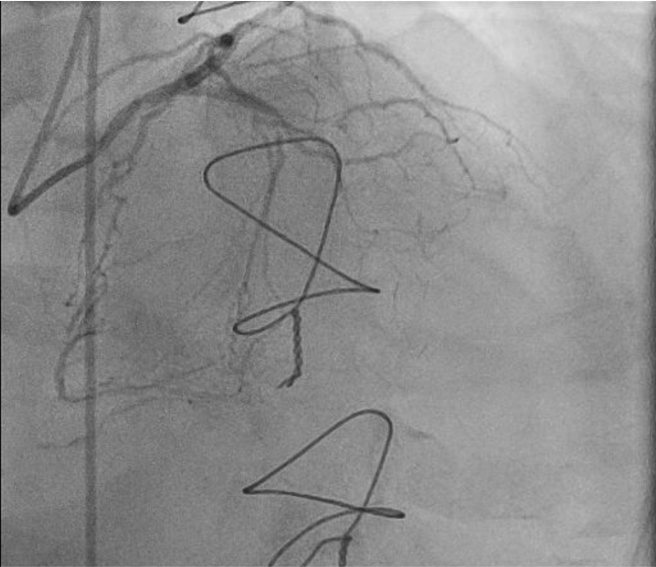
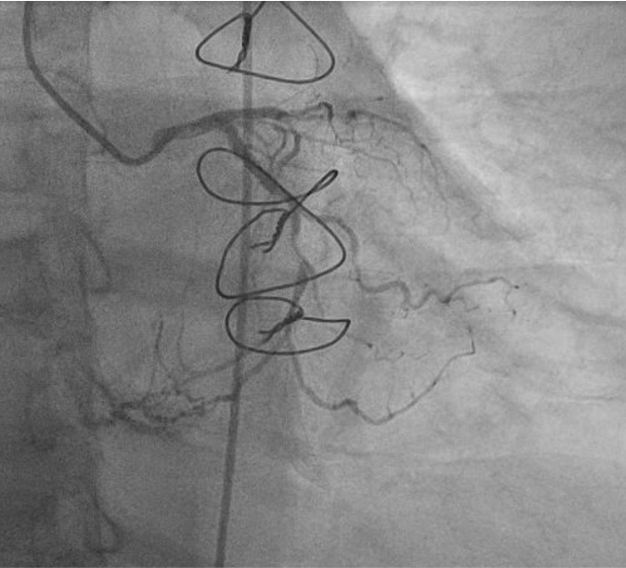
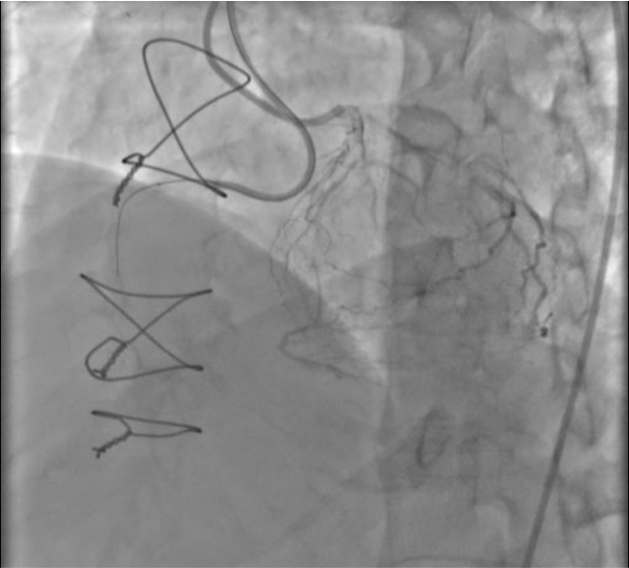
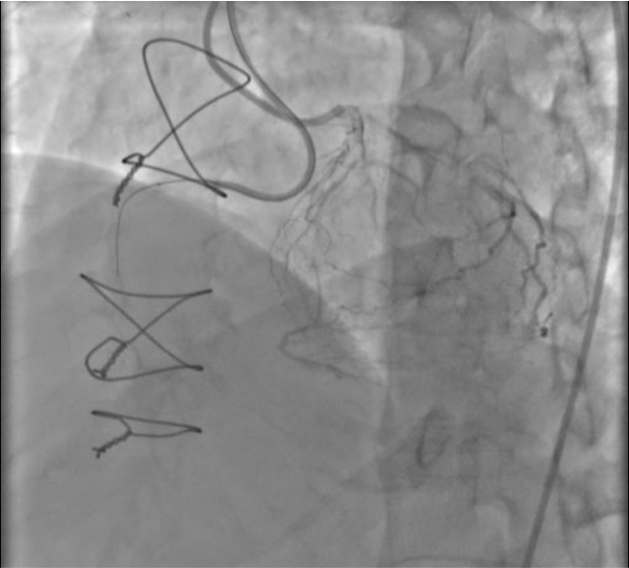
Dual injection was performed ( transradial with guiding JL 3.5/6F cannulated in LCA , and transfemoral with guiding AL 1/6F cannulated in RCA). Gaia II and Gaia III failed to cross the lesion antegradely in proximal RCA with microcatheter Finecross 1.8F/130 cm due to imprecise distal. Wiring with workhorse wire through the left system, crossing the septal LAD and placed as a marker wire in PL branch retrogradely with microcatheter Finecross 1.8F/150 cm. Unfortunately the microcatheter failed to cross the PL branch. Continue the antegrade technique with escalating wire Conquest Pro 12 and successfully crossed the lesion and placed in PDA. Anchor balloon SC 2.0/15 mm was inflated in proximal RV branch to facilitate microcatheter to distal RCAExchange wire to workhorse wire in distal RCA. Retrograde marker wire was withdrawn and guiding JL in left system was disengaged. Predilate with balloon 3.0/15 mm from proximal to distal with 10 atm. Everolimus stent 2.5/38 mm was implanted from mid to distal before PL-PDA bifurcation with 11 atm Everolimus stent 3.0/38 mm was implanted from proximal to mid ,overlap from previous stent with 10 atm Everolimus stent 3.5/24 mm was implanted from osteal to proximal, overlap from previous stent with 10 atm (full metal jacket)Postdilatation and flair with balloon ex-stent (3.5/24 mm) was inflated with maximum pressure of 16 atm intrastent. Total flurotime was 90 minutes, last evaluation: TIMI 3 flow, no perforation, no dissection, no residual stenosis.




Case Summary
This case showed the necessity to have a backup plan when things did not go our way. J-CTO score of 2 showed only 34.8% success rate in crossing the lesion less than 30 minutes. Another lesson learnt from this case would be not to force the retrograde microcatheter to pass the stuck passage near the PL branch owing to the fact it would cause perforation which could lead to pericardial effusion. The retrograde marker wire allowed us to guide the antegrade wire finding the true lumen along the vessel. The uncrossable antegrade microcatheter was solved with no harm by doing anchor balloon at proximal RV branch. Understanding the steps allowed us to accomplish the procedure well.


