Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-124
Touch-Me-Not: Proximal Propagation of Intramural Hematoma in Spontaneous Coronary Artery Dissection After Stenting
By Arvin Romero Yumul, Regidor Ricohermoso Encabo, Ariel Miranda
Presenter
Arvin Romero Yumul
Authors
Arvin Romero Yumul1, Regidor Ricohermoso Encabo1, Ariel Miranda1
Affiliation
Cardinal Santos Medical Center, Philippines1,
View Study Report
TCTAP C-124
CORONARY - Complications (Coronary)
Touch-Me-Not: Proximal Propagation of Intramural Hematoma in Spontaneous Coronary Artery Dissection After Stenting
Arvin Romero Yumul1, Regidor Ricohermoso Encabo1, Ariel Miranda1
Cardinal Santos Medical Center, Philippines1,
Clinical Information
Patient initials or Identifier Number
R.C.M.
Relevant Clinical History and Physical Exam
We present a case of a 45-year-old woman, non-smoker, non-pregnant, without any co-morbidities, and denies hormonal therapy, who presented a month ago with sudden onset right-sided chest pain, accompanied by diaphoresis and shortness of breath noted after an episode of severe emotional stress. She was initially brought to another hospital and 12-lead ECG showed ST-segment elevation in leads V1 to V4 and was managed conservatively as a case of acute coronary syndrome.
Relevant Test Results Prior to Catheterization
She was then referred to our institution 1 month post discharge for further evaluation. On work-up, treadmill stress test showed a preserved ejection fraction (EF) of 54% but with worsening of previously noted wall motion abnormality in the left anterior descending (LAD) artery territory and progression of symptoms at a low workload of only 5.4 METS.
Relevant Catheterization Findings
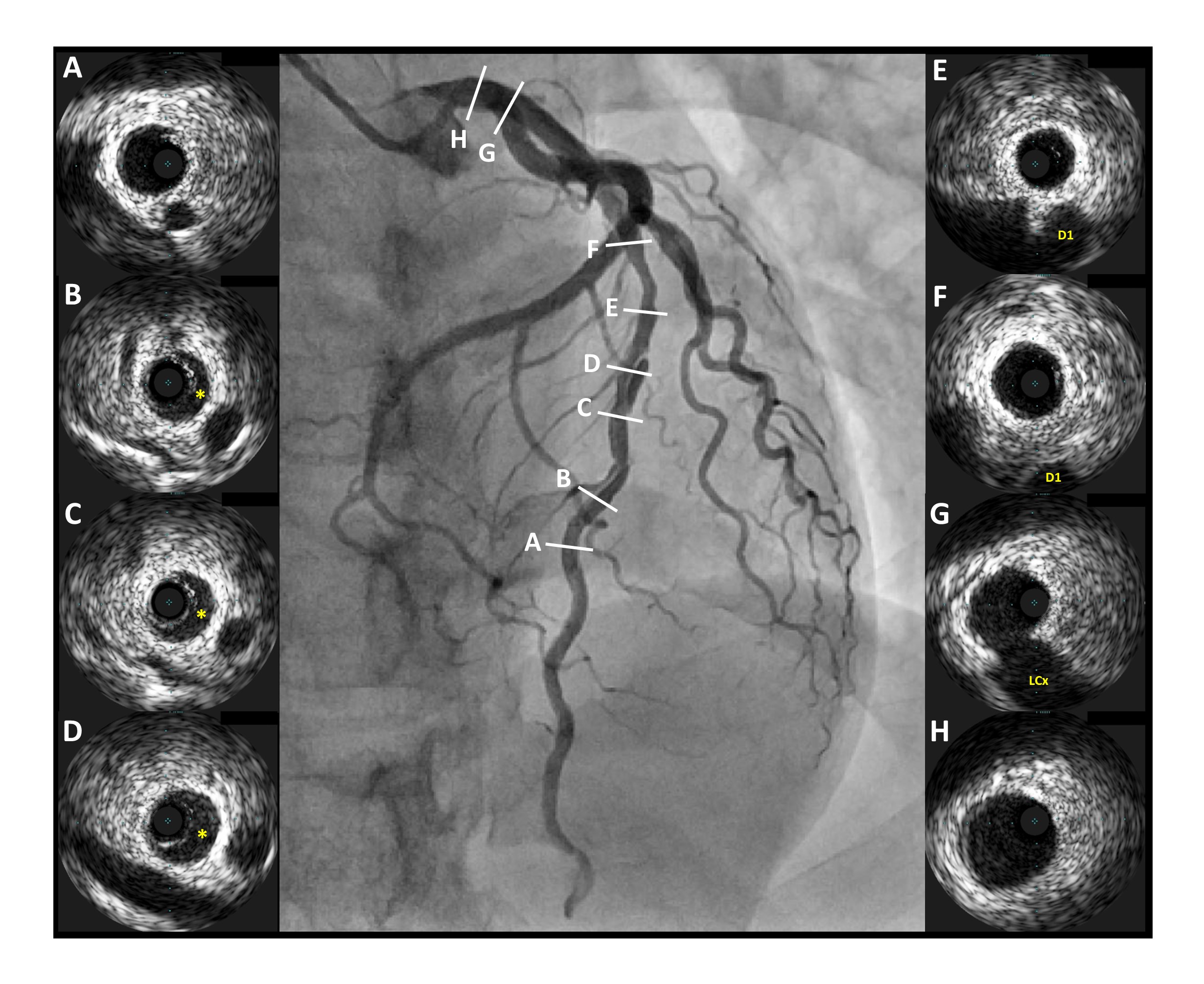
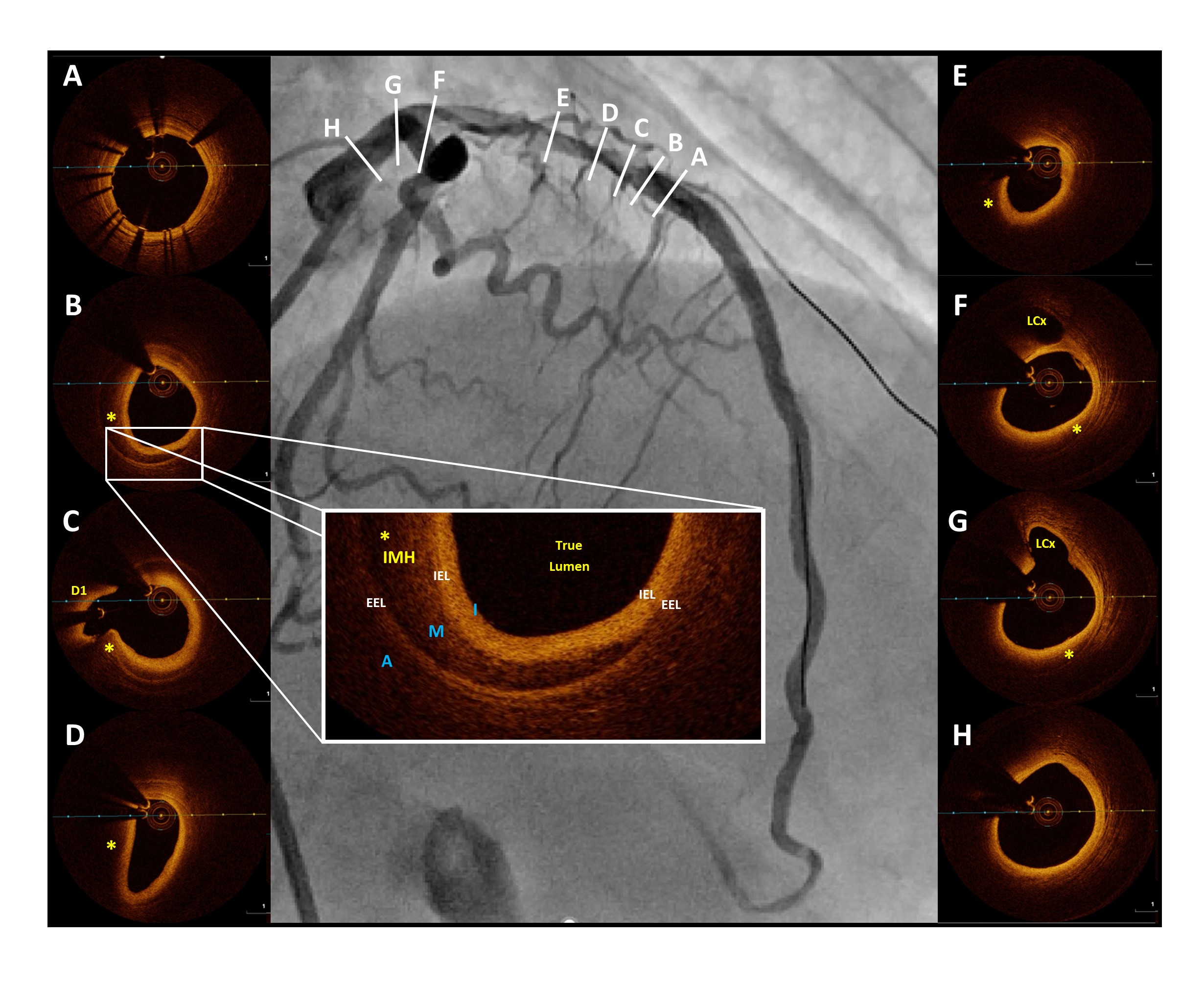
Coronary angiogram with intravascular ultrasound (IVUS) was then done and showed a 20 mm type-1 spontaneous coronary artery dissection (SCAD) at the mid to distal LAD shown by the yellow arrows (Fig1) and yellow asterisk (Fig2), while the rest of the coronaries were normal. Since the patient remained symptomatic with poor functional capacity despite 1 month of conservative management, we decided to proceed with percutaneous coronary intervention (PCI).


Interventional Management
Procedural Step
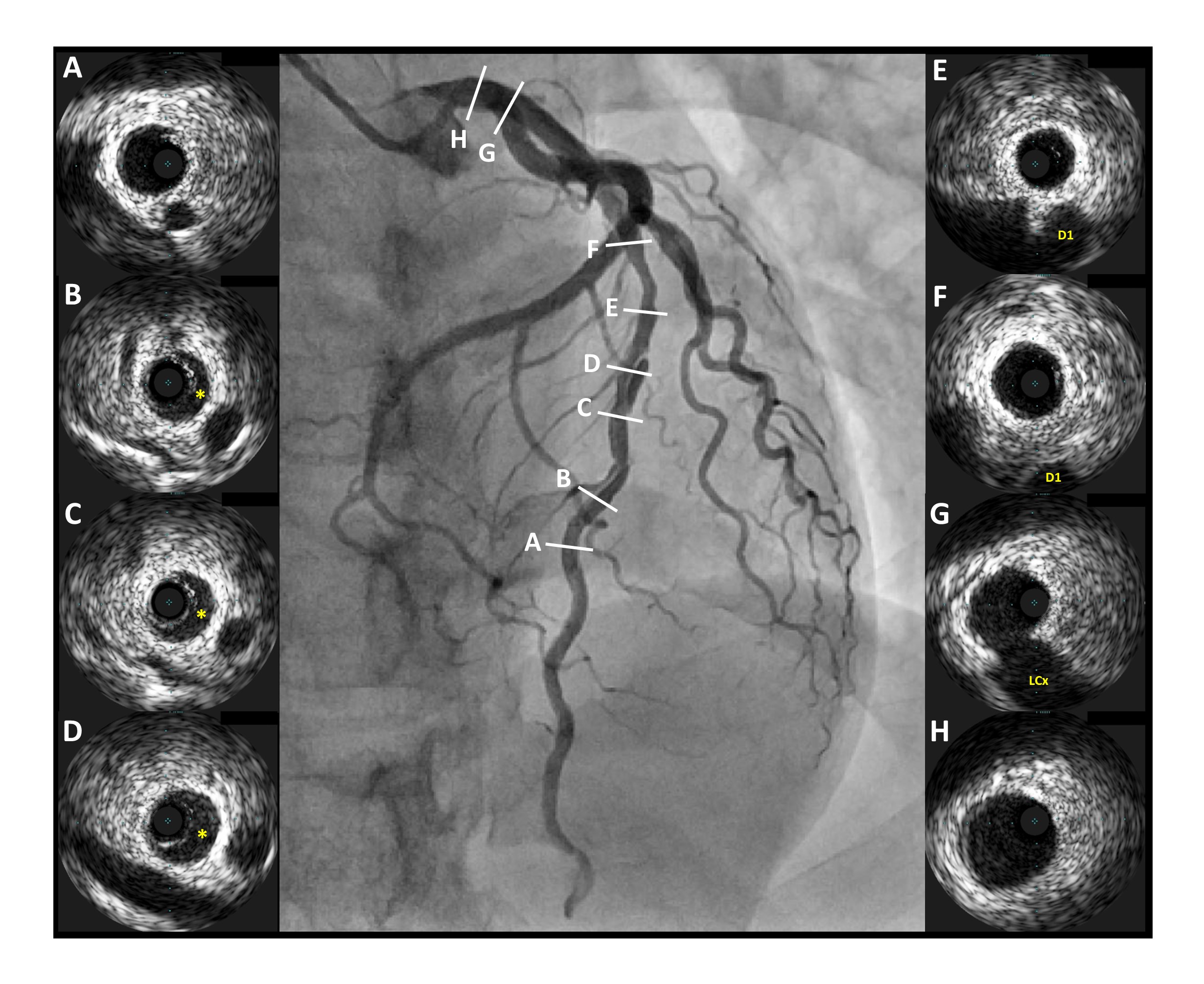
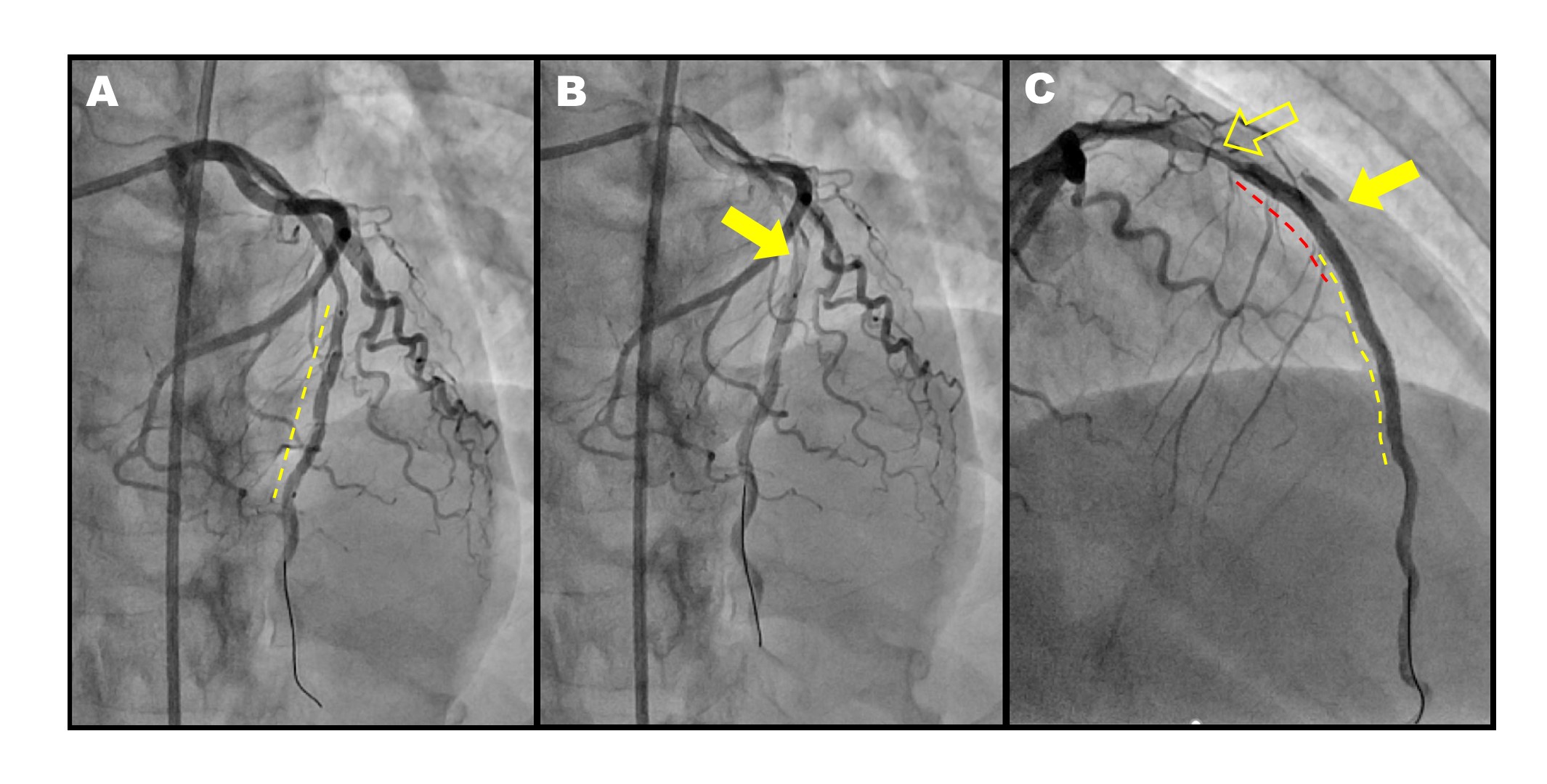
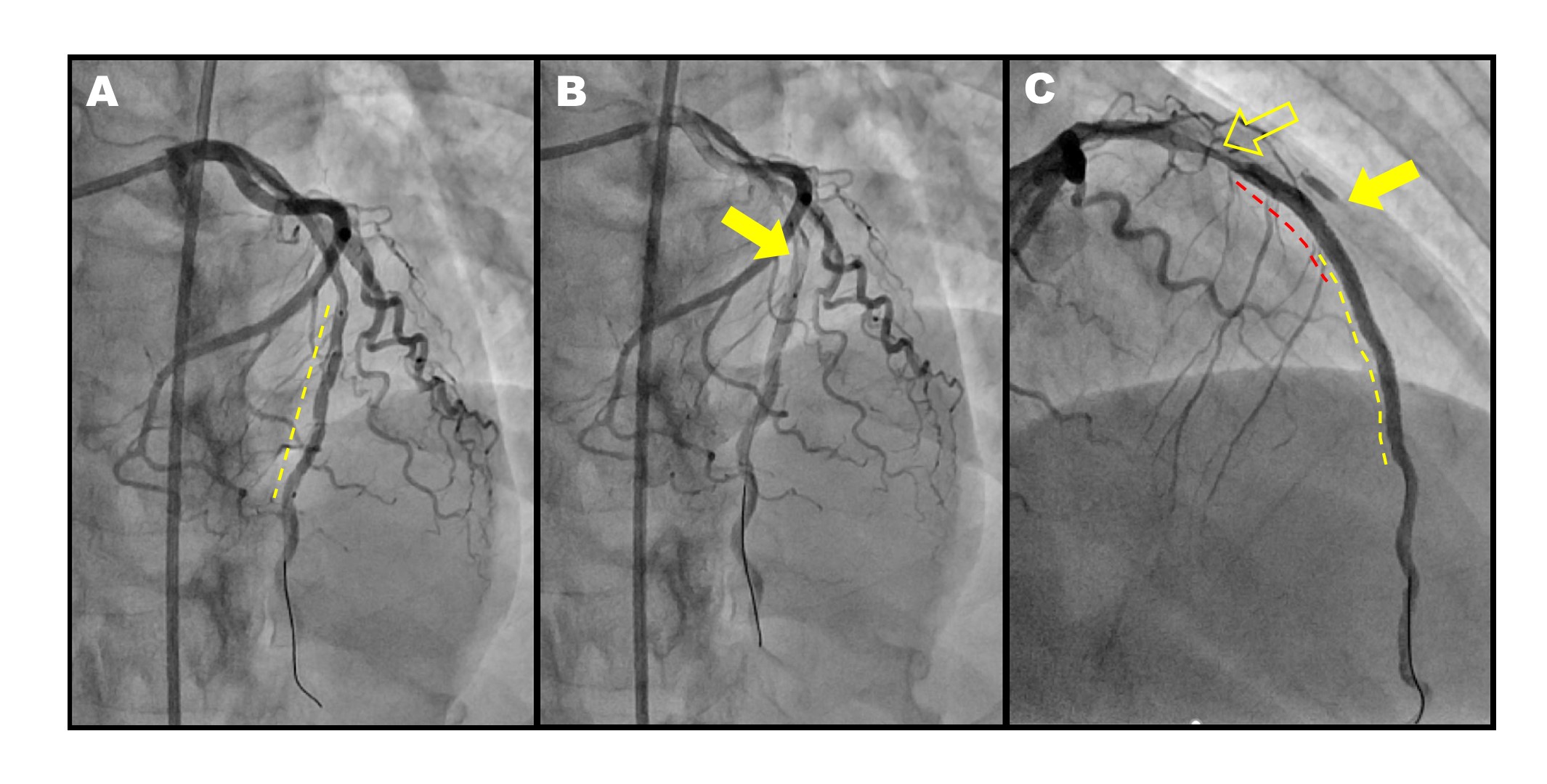
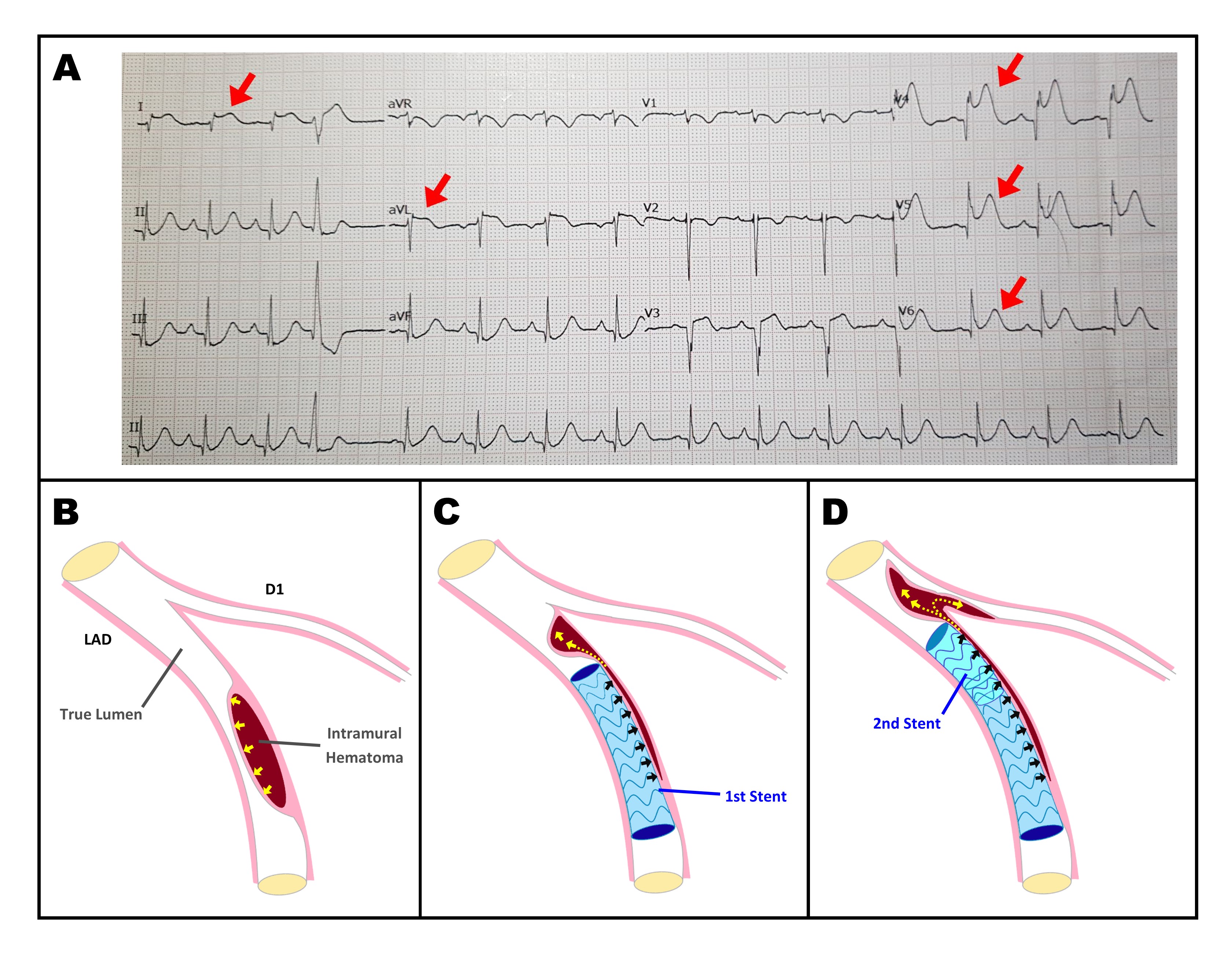
Pre-dilation of the mid LAD was done using a 2.0x15 mm balloon and a 2.75x30 mm Zotarolimus-eluting stent (ZES) was deployed in the mid to distal LAD extending 5 mm from both edges of the IMH (normal-to-normal) (Fig3A). There was note of TIMI 2 flow immediately after deployment with note of staining in the proximal edge suggestive of proximal IMH extension (Fig3B), hence another ZES, 3.0x18 mm was deployed at the mid LAD after the diagonal branch (D1) ostium and overlapping the previous stent distally. Angiogram showed acute stenosis proximal to the stent accompanied by contrast staining at the ostio-proximal D1 with TIMI 1 flow suggestive of further extension of the IMH proximally (Fig3C). The patient noted sudden chest pain with new onset ST-segment elevation in leads V4 to V6, I and aVL consistent with a compromised blood flow in the lateral wall (Fig4A) caused by the “squeezing-induced” IMH propagation during stent deployment (Fig4B, 4C, 4D). An optical coherence tomography (OCT) run in the LAD was done to further characterize and strategize the approach which clearly showed well apposed and expanded stents but with proximal extension of the IMH compromising the D1 flow and involving the ostial LAD and sparing of the left main (Fig5). After a few minutes of observation, there was resolution of the chest pain with stable vital signs and final angiogram showed TIMI 3 flow into the LAD but still with TIMI 1 flow in the D1.
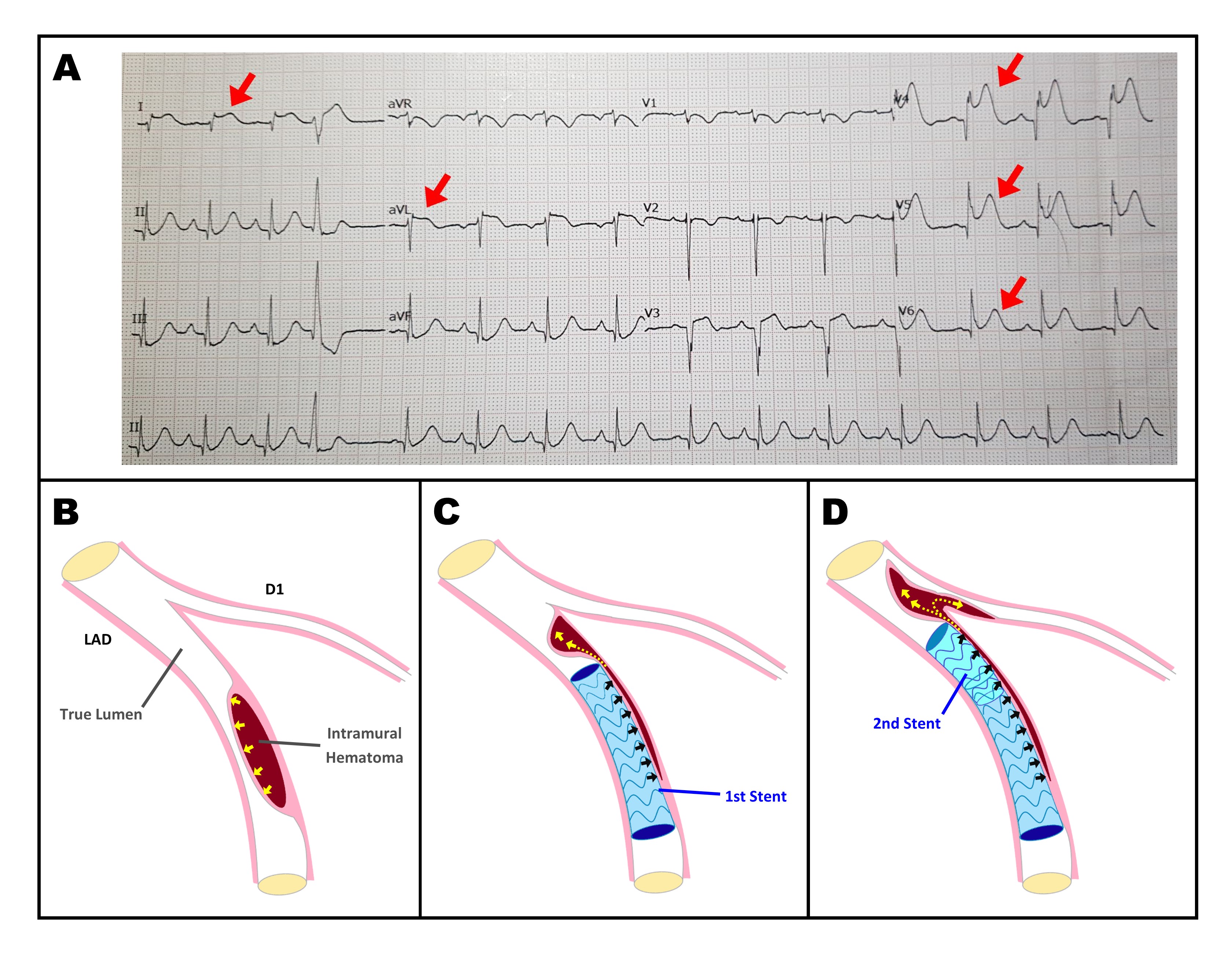
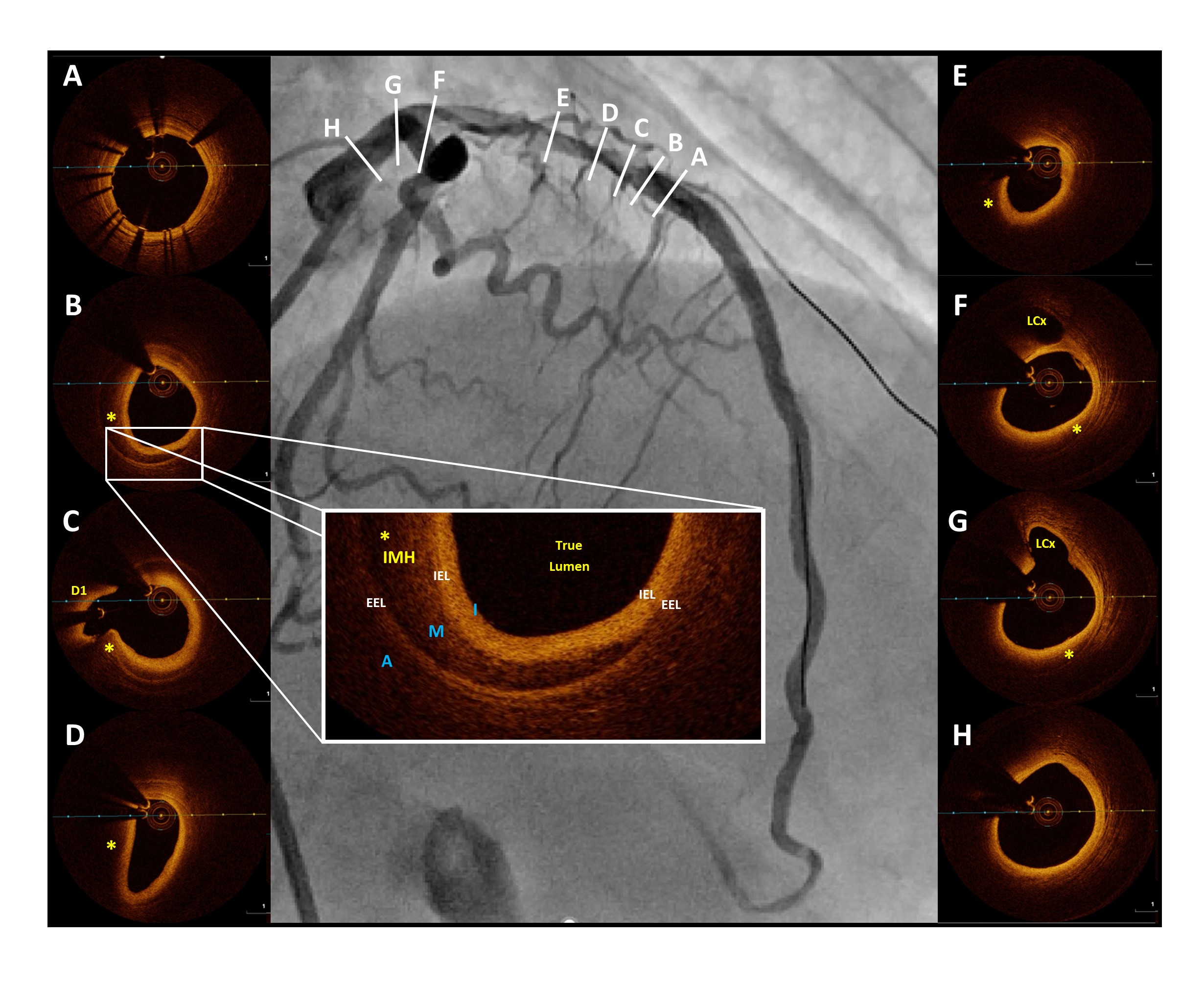
Case Summary
Diagnosis of SCAD requires a high index of suspicion particularly in young women with predisposing factors. Management of SCAD remains challenging despite advances in PCI techniques with dissection extension as one of the primary pitfalls of stenting. Both IVUS and OCT are extremely helpful in defining the extent of SCAD which influences intraprocedural decision making. In our case, after confirming that there was no involvement of the left main, we decided to conclude the procedure without performing post-dilation in order to avoid the risk of further extending the IMH into the left main and possibly even into the aorta which may lead to a catastrophic complication.


