Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-199
Left Main Coronary Artery Thrombosis During Transcatheter Aortic Valve Implantation
By Mary Jane Penelope Diaz Gatpatan, Alwyn Susanto, Terence Cuezon, Douglas Bailon, Ferdinand Alzate, Fabio Enrique Posas
Presenter
Mary Jane Penelope Diaz Gatpatan
Authors
Mary Jane Penelope Diaz Gatpatan1, Alwyn Susanto2, Terence Cuezon1, Douglas Bailon1, Ferdinand Alzate1, Fabio Enrique Posas1
Affiliation
St. Luke's Medical Center, Philippines1, St Lukes Medical Center Quezon City, Philippines2,
View Study Report
TCTAP C-199
STRUCTURAL HEART DISEASE - Valvular Intervention: Aortic
Left Main Coronary Artery Thrombosis During Transcatheter Aortic Valve Implantation
Mary Jane Penelope Diaz Gatpatan1, Alwyn Susanto2, Terence Cuezon1, Douglas Bailon1, Ferdinand Alzate1, Fabio Enrique Posas1
St. Luke's Medical Center, Philippines1, St Lukes Medical Center Quezon City, Philippines2,
Clinical Information
Patient initials or Identifier Number
FA
Relevant Clinical History and Physical Exam
Patient is an 82-year-old female, hypertensive, diabetic, diagnosed breast cancer St II, post modified radical mastectomy, left and radiation therapy, admitted due to progressive dyspnea. Cardiac exam revealed distinct s1, soft s2, with grade 3/6 holosystolic murmur at the 2nd intercostal space right parasternal border.
Relevant Test Results Prior to Catheterization
2D echo
Relevant Catheterization Findings
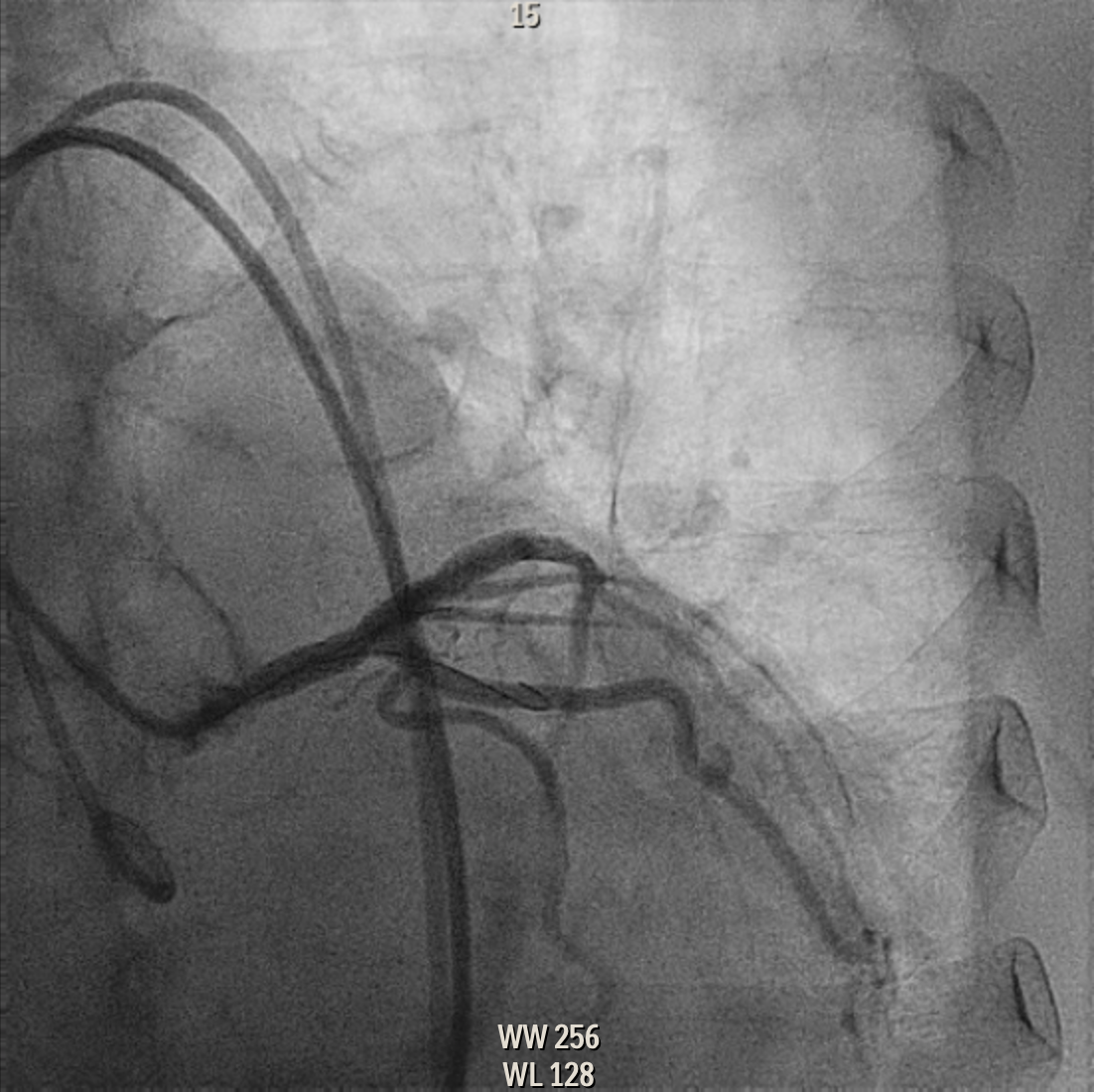
The left main coronary artery is a normal-sized vessel with non-significant stenosis at the ostium.The left anterior descending and circumflex arteries are normal-sized vessel that appears to be free of disease. The right coronary artery is a normal- sized dominant vessel with moderate (50-70%) stenosis of the mid right posterolateralbranch.
Interventional Management
Procedural Step
Transcutaneous Aortic Valve Implantation and Percutaneous Coronary Intervention of the Ostial Left Main
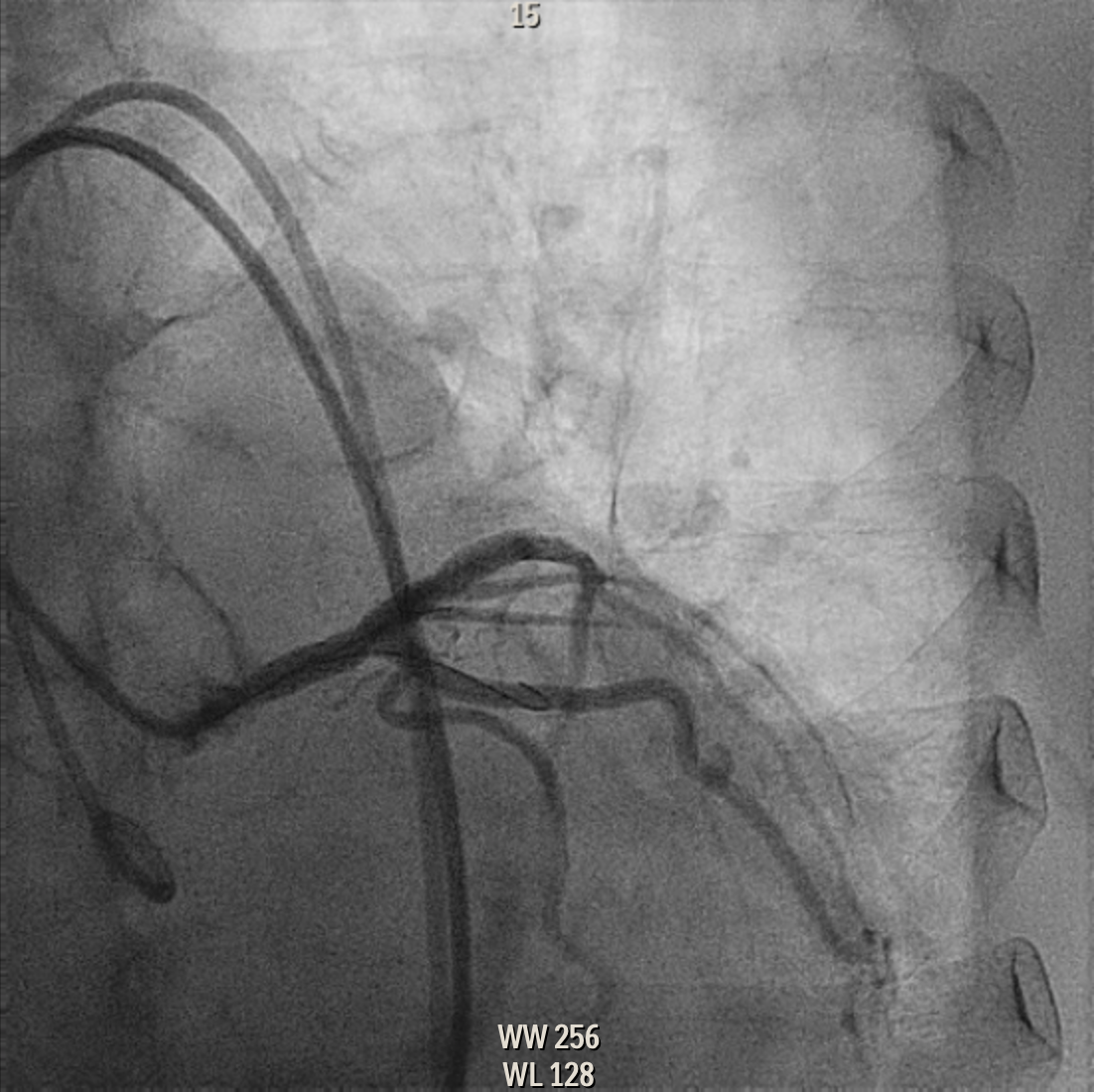
 1 LM preTAVI.png
1 LM preTAVI.png
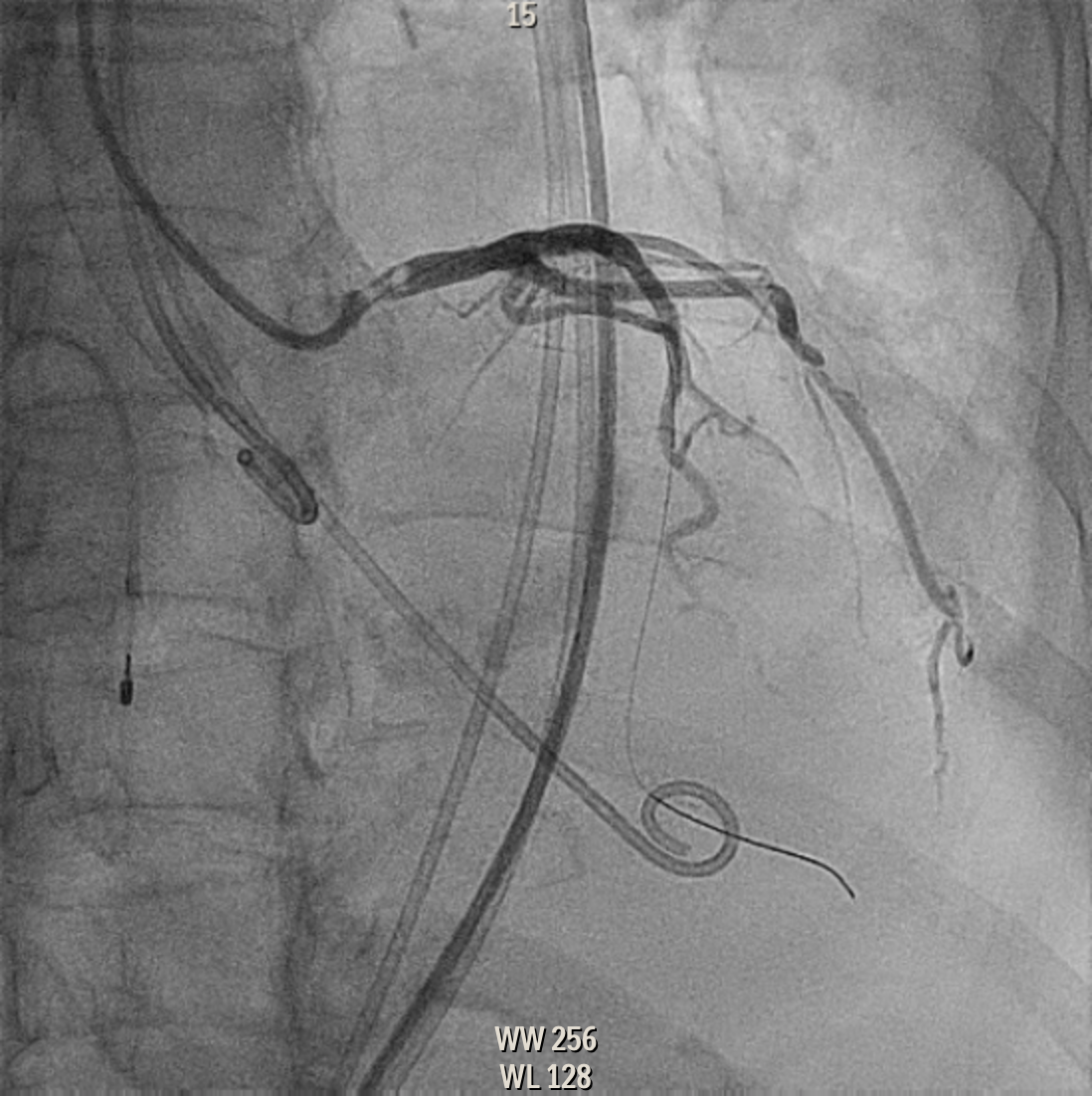

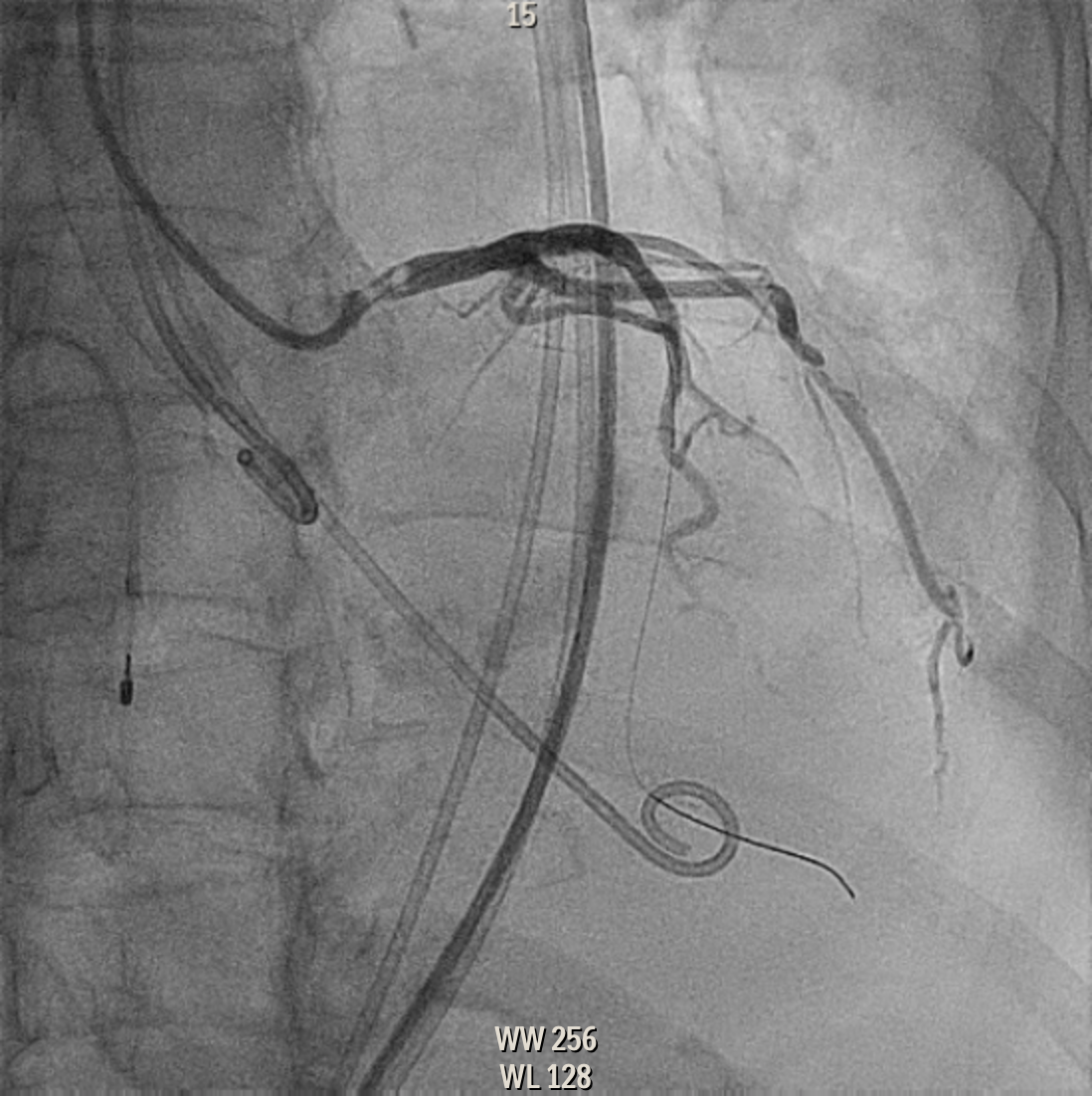

Case Summary
TAVI is the favored intervention for patients with severe aortic stenosis who have prohibitive surgical risk. Despite being less invasive than SAVR, TAVI still carries critical risks. One of dreaded intraprocedural complication is acute coronary obstruction. Coronary protection with preemptive wiring of the at-risk coronary ostia and eventual stent implantation is a strategy to prevent coronary obstruction. However, this strategy may carry a potential risk of thrombosis. Coronary artery thrombosis during TAVI is a rare occurrence, hence poorly studied. Endothelial injury or erosion from the wiring of the coronary artery can be a possible cause of thrombosis.


