Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-118
Iatrogenic Aorto-Coronary Dissection of the Right Coronary Artery During Diagnostic Angiography Using a Tiger Catheter
By Ronald Santos, Meliton III Aquines Evangelista, Alwyn Susanto, Conrad Estanislao, Paterno Frias Dizon, Joanne Cosare San Pedro
Presenter
Meliton III Aquines Evangelista
Authors
Ronald Santos1, Meliton III Aquines Evangelista1, Alwyn Susanto2, Conrad Estanislao1, Paterno Frias Dizon1, Joanne Cosare San Pedro1
Affiliation
St. Luke's Medical Center, Philippines1, St Lukes Medical Center Quezon City, Philippines2,
View Study Report
TCTAP C-118
CORONARY - Complications (Coronary)
Iatrogenic Aorto-Coronary Dissection of the Right Coronary Artery During Diagnostic Angiography Using a Tiger Catheter
Ronald Santos1, Meliton III Aquines Evangelista1, Alwyn Susanto2, Conrad Estanislao1, Paterno Frias Dizon1, Joanne Cosare San Pedro1
St. Luke's Medical Center, Philippines1, St Lukes Medical Center Quezon City, Philippines2,
Clinical Information
Patient initials or Identifier Number
RC
Relevant Clinical History and Physical Exam
A 64-year-old female, hypertensive, diabetic, with degenerative disc disease was admitted for nerve root decompression. During hospitalization, the patient complained of chest heaviness and shortness of breath and was managed as a case of ACS-NSTEMI. Physical exam was unremarkable and vital signs were stable. She was referred for coronary angiogram prior to the spine surgery.
Relevant Test Results Prior to Catheterization
HS-Trop I: 1735 ng/L
Relevant Catheterization Findings
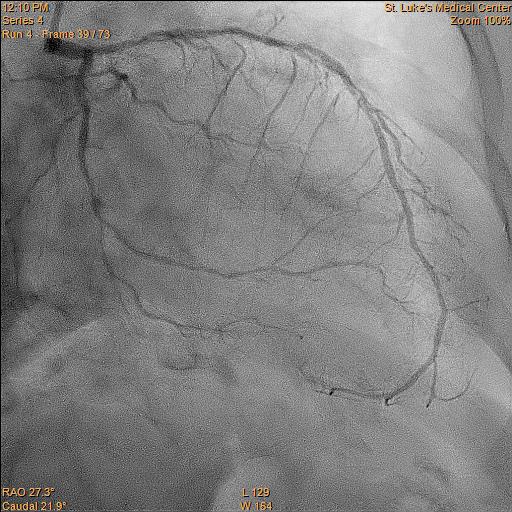
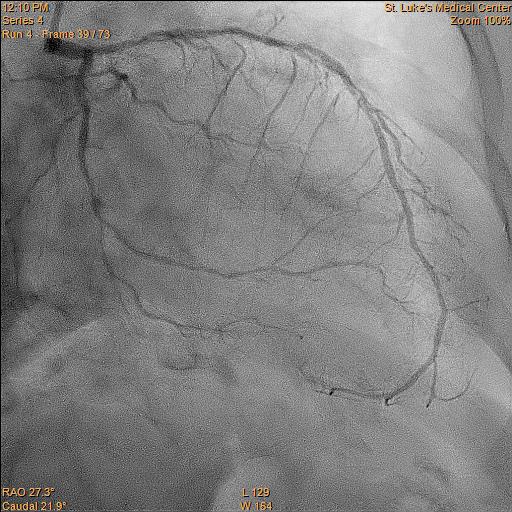
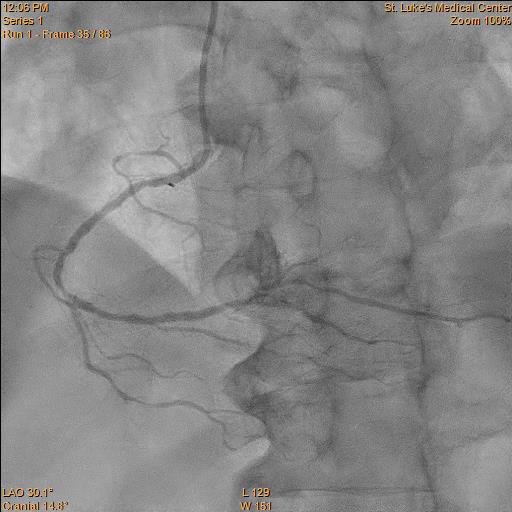
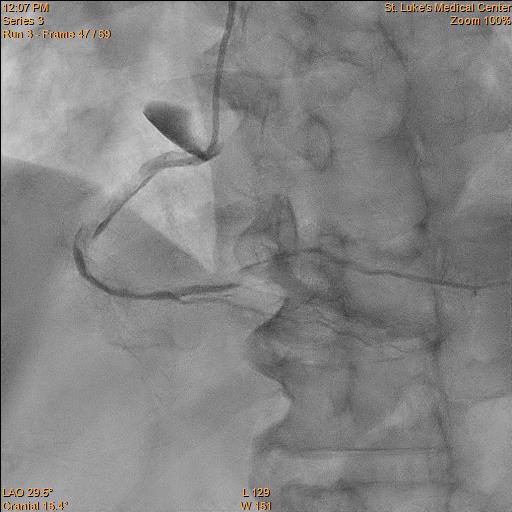
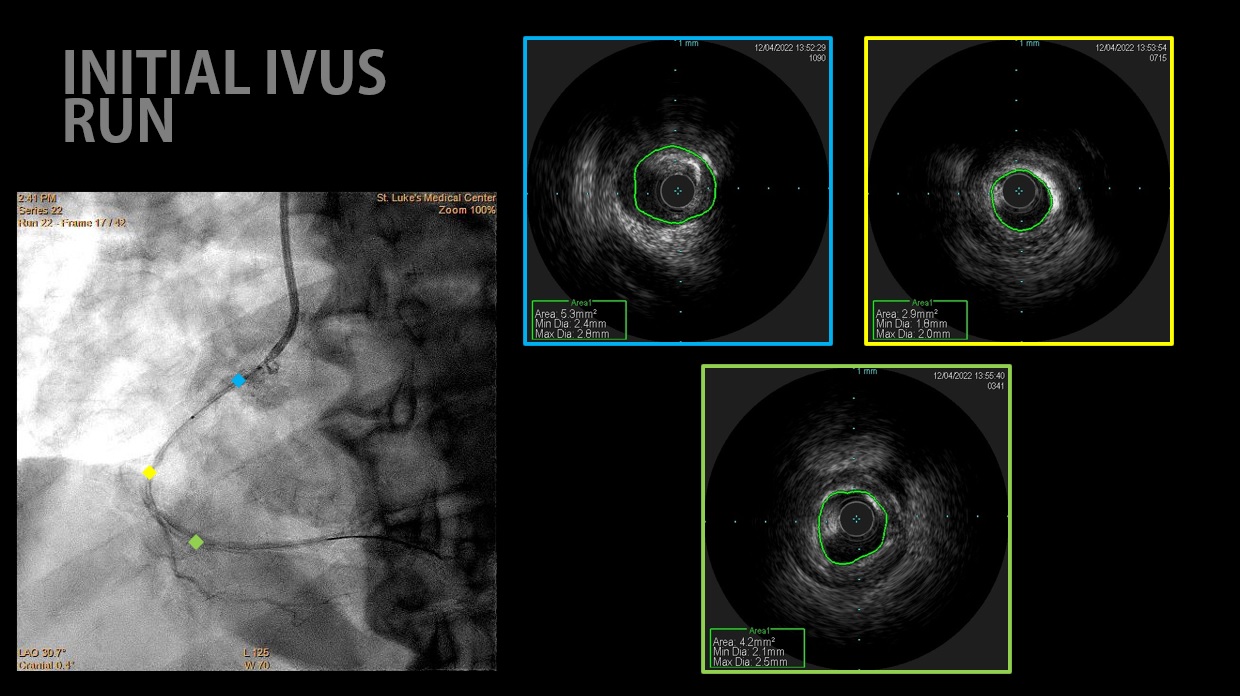
The LMCA appears disease-free.
Interventional Management
Procedural Step
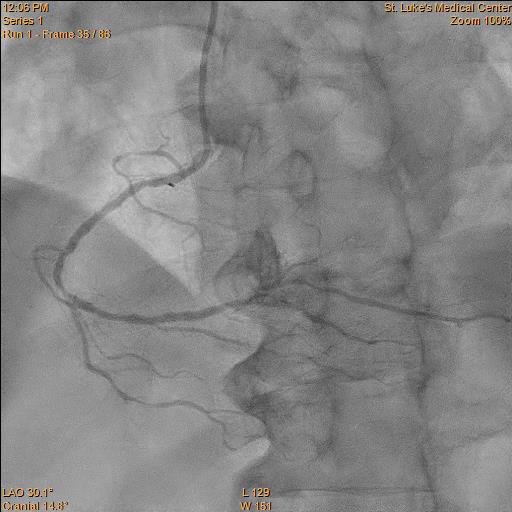
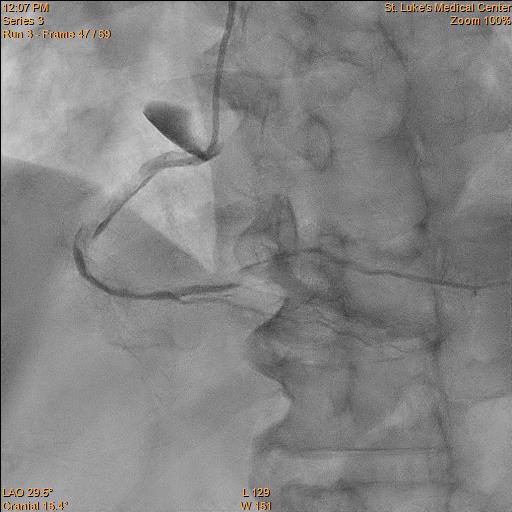
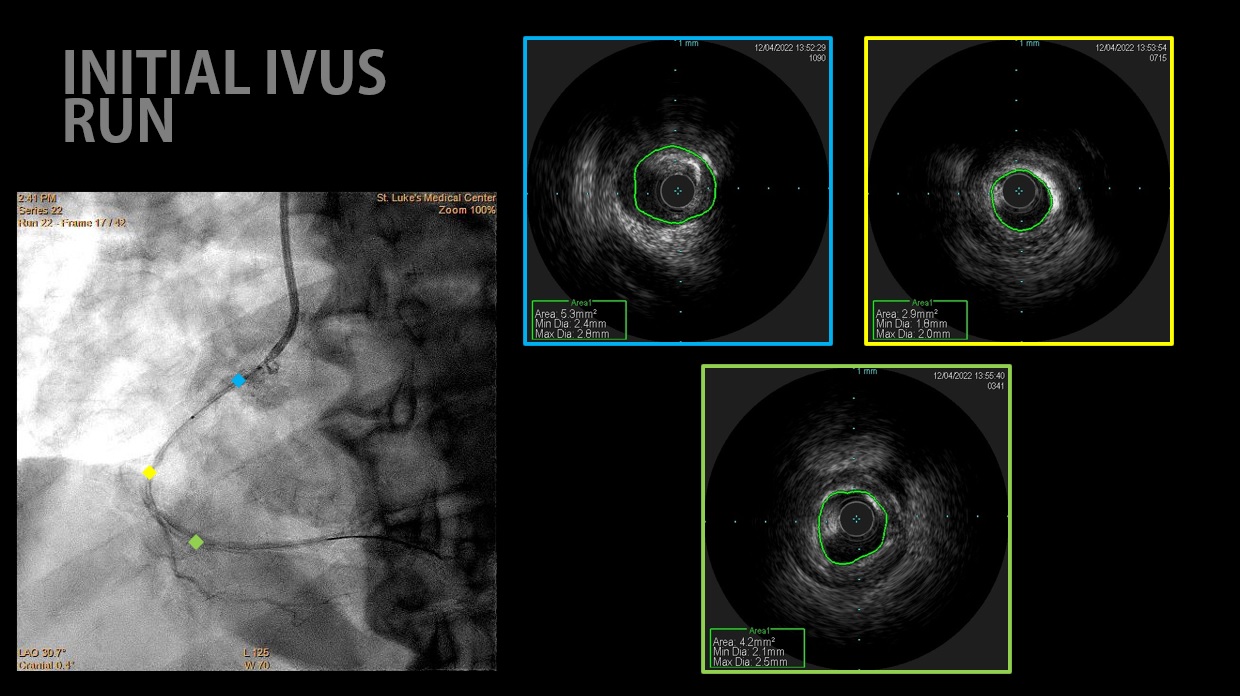
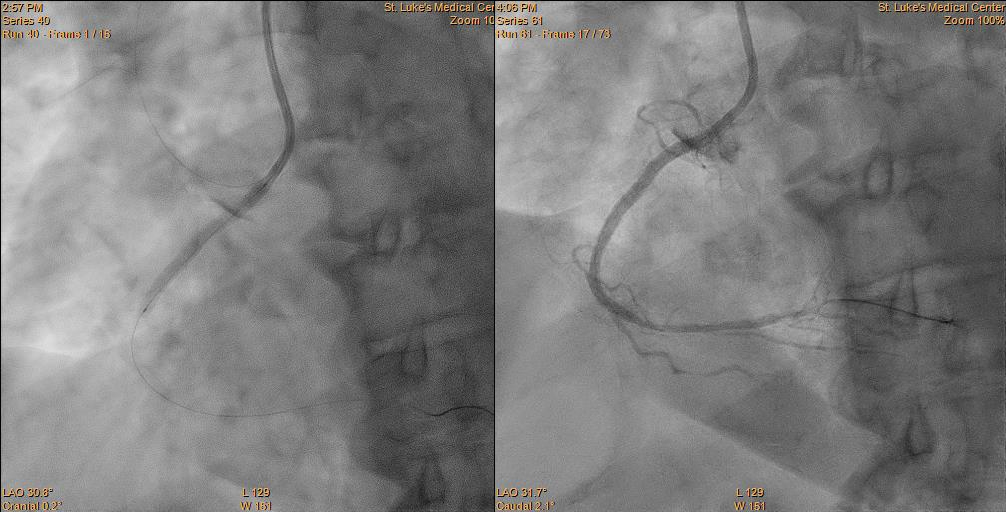
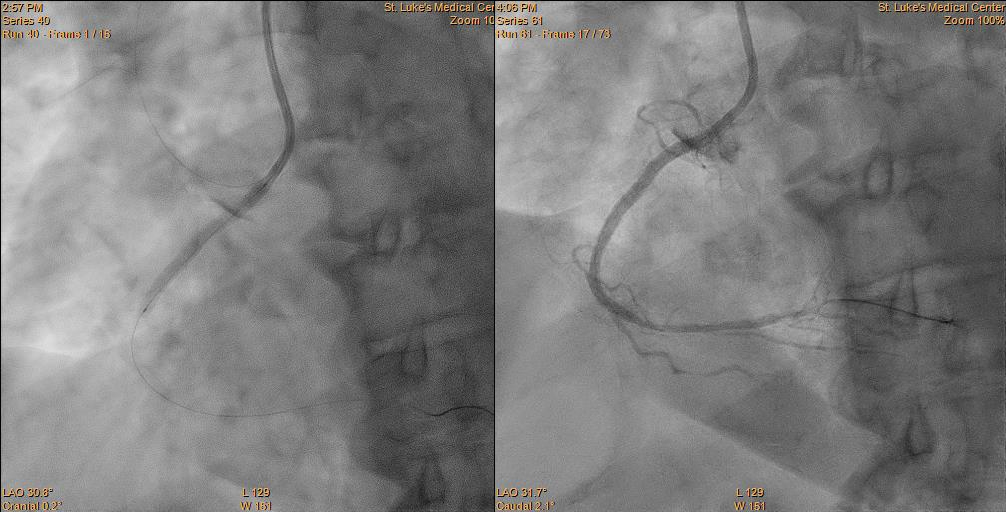
A Heartrail II (Terumo, Japan) JR4 6F guiding catheter was used to engage the right coronary ostium.


Case Summary
Iatrogenic catheter-induced coronary artery dissection is a significant but uncommon side effect of coronary angiography. During regular coronary angiography, the incidence of coronary artery dissection has been found to be around 0.1%, with the right coronary artery dissection being more often than the left. The most common cause of this is mechanical damage to the artery wall brought on by the manipulation of either a wire or a catheter.


