Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-117
In a Blink of an Eye: A Case of Distal Coronary Wire Perforation
By Menaka Mahendran, Houng Bang Liew
Presenter
Menaka Mahendran
Authors
Menaka Mahendran1, Houng Bang Liew2
Affiliation
Hospital Queen Elizabeth II, hospital Serdang, Malaysia1, Queen Elizabeth II Hospital, Malaysia2,
View Study Report
TCTAP C-117
CORONARY - Complications (Coronary)
In a Blink of an Eye: A Case of Distal Coronary Wire Perforation
Menaka Mahendran1, Houng Bang Liew2
Hospital Queen Elizabeth II, hospital Serdang, Malaysia1, Queen Elizabeth II Hospital, Malaysia2,
Clinical Information
Patient initials or Identifier Number
Mr.A
Relevant Clinical History and Physical Exam
57 years old gentleman with underlying diabetes and hypertension had a history of anterior ST-elevation myocardial infarction 1 year ago, for which he had received successful thrombolytic therapy. A coronary angiogram was done with a proximal LAD stenting. He presented electively for a stage procedure for his right coronary artery. He has otherwise been well for the past 1 year with no reduced effort tolerance or chest pain.
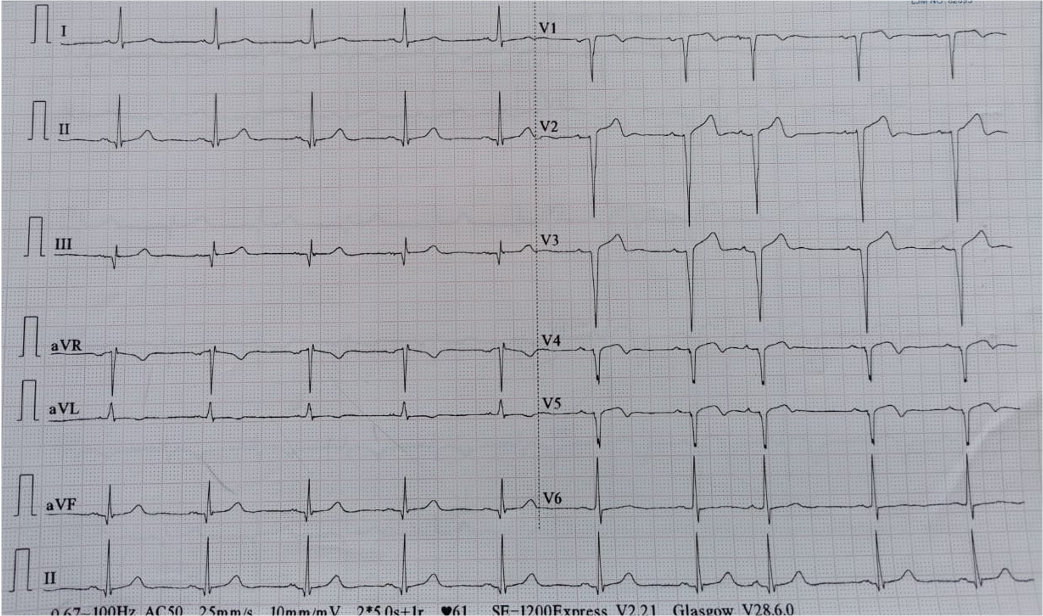
Relevant Test Results Prior to Catheterization
Blood investigations :Hemoglobin : 15.1 g/dL Platelet : 221 x 10^9/L.
Relevant Catheterization Findings
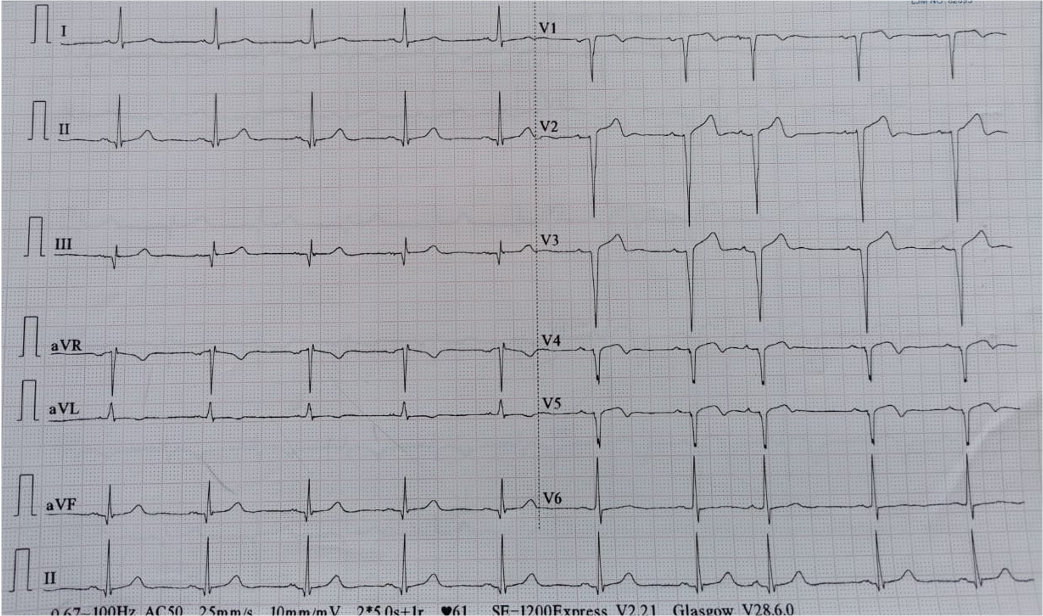
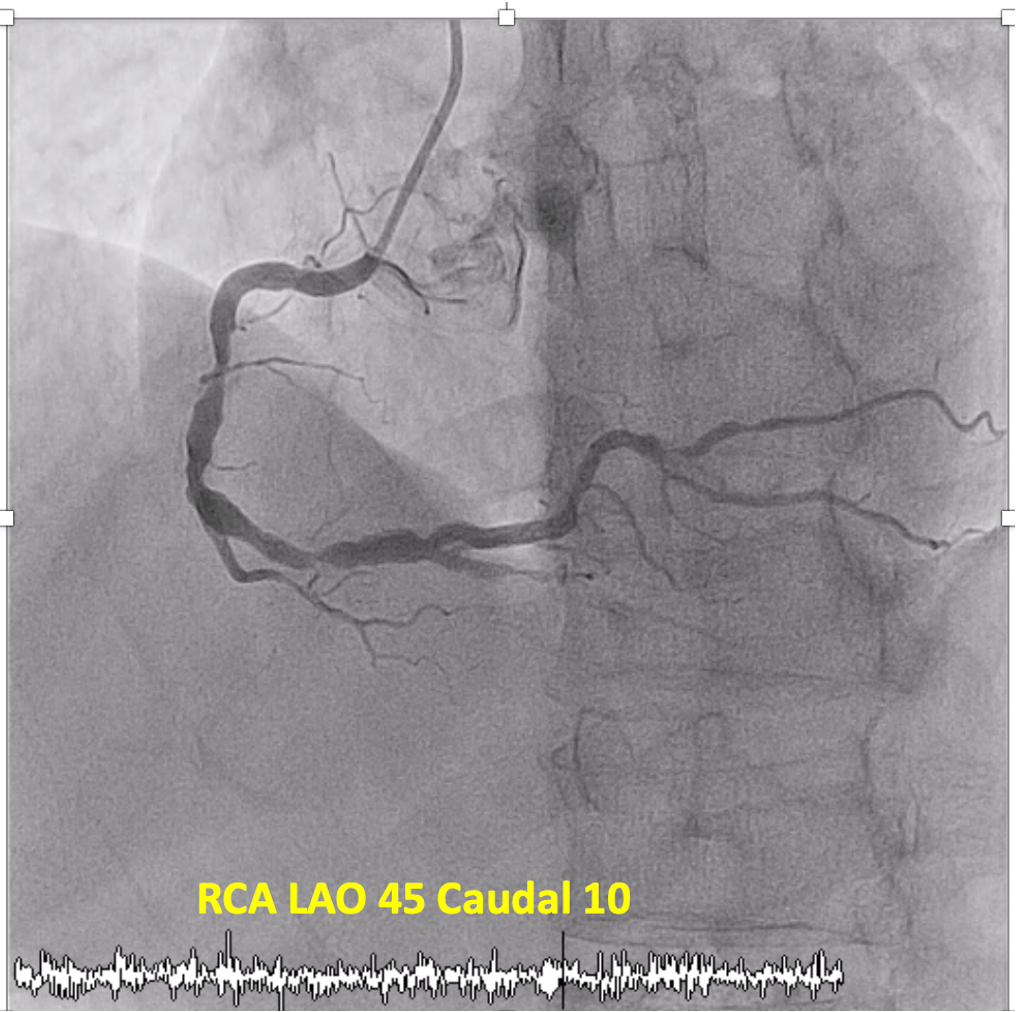
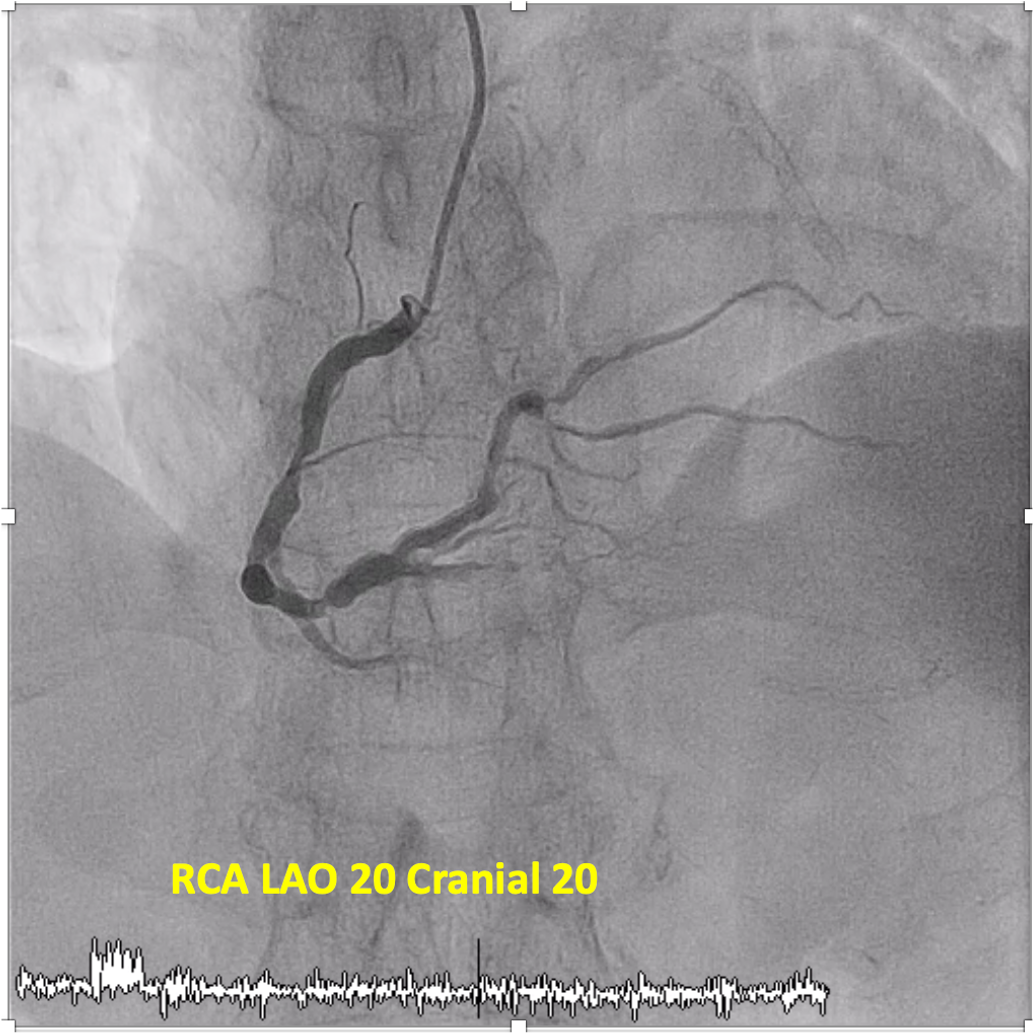
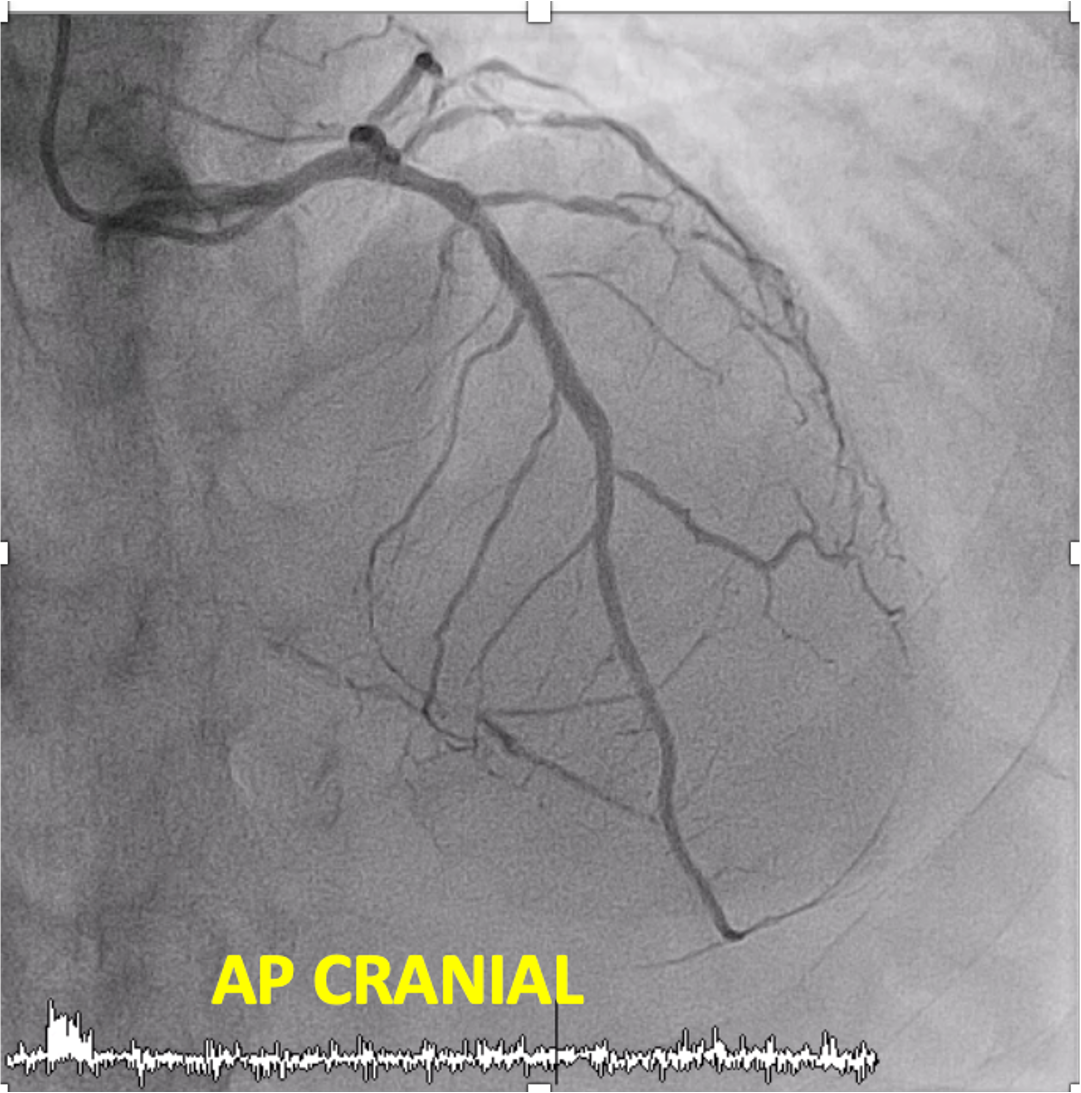
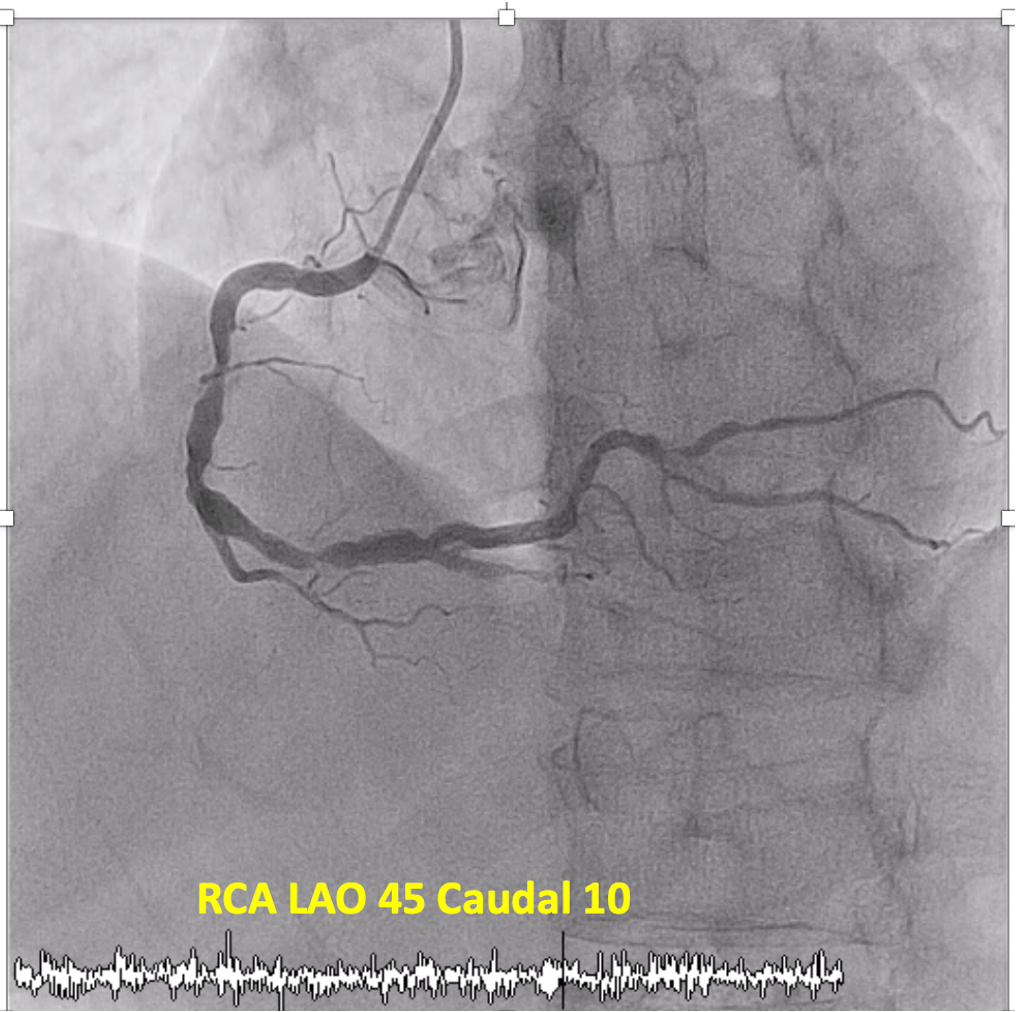
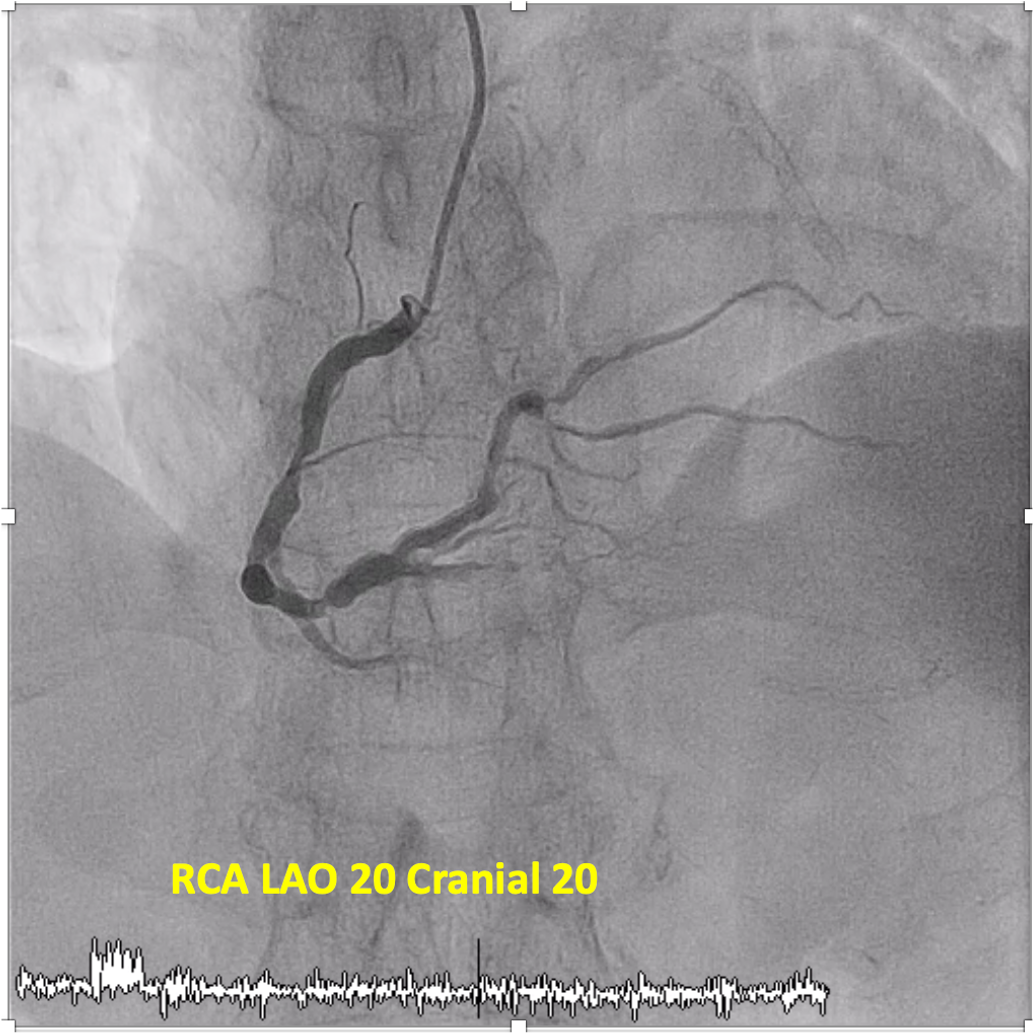
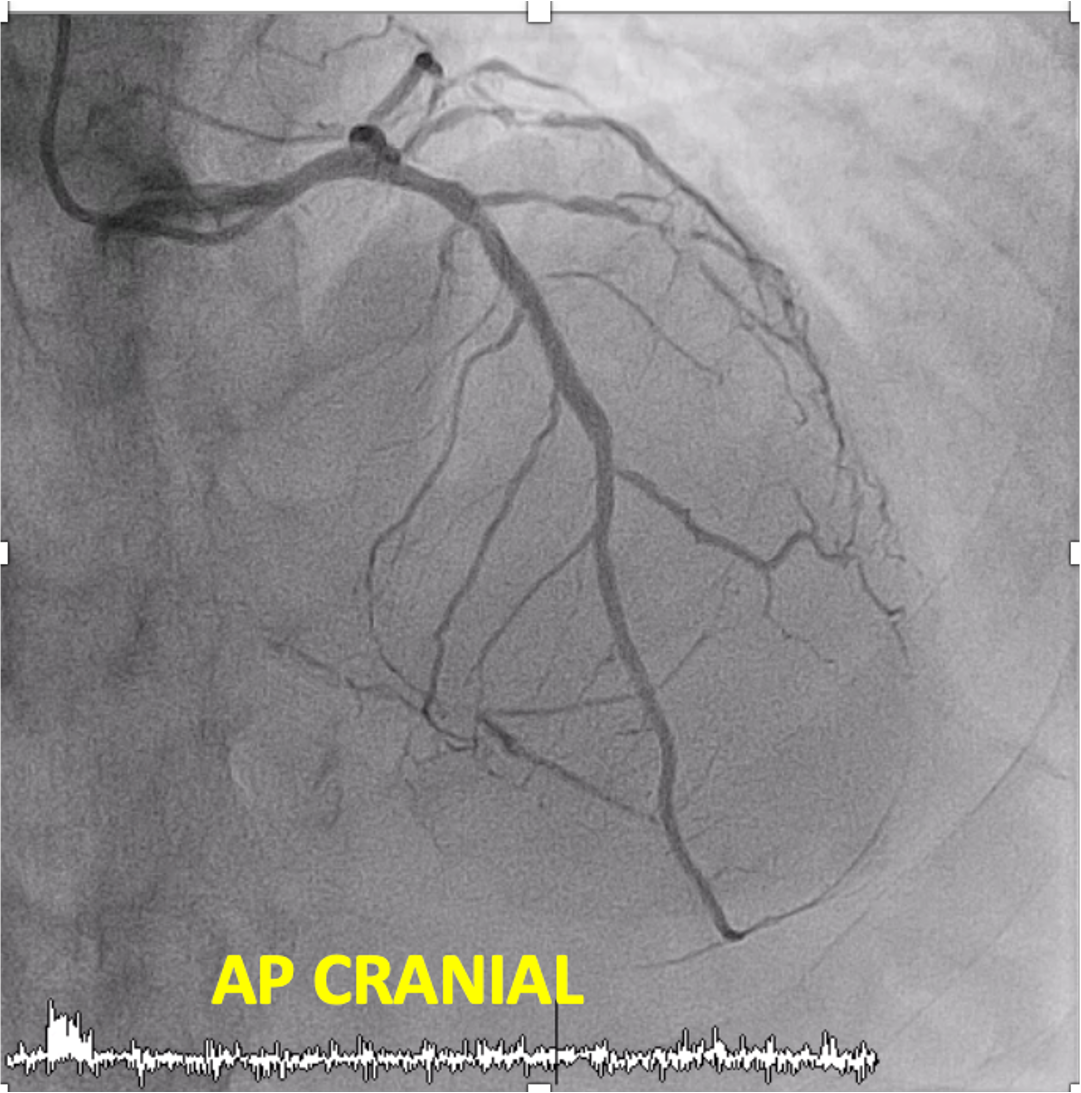
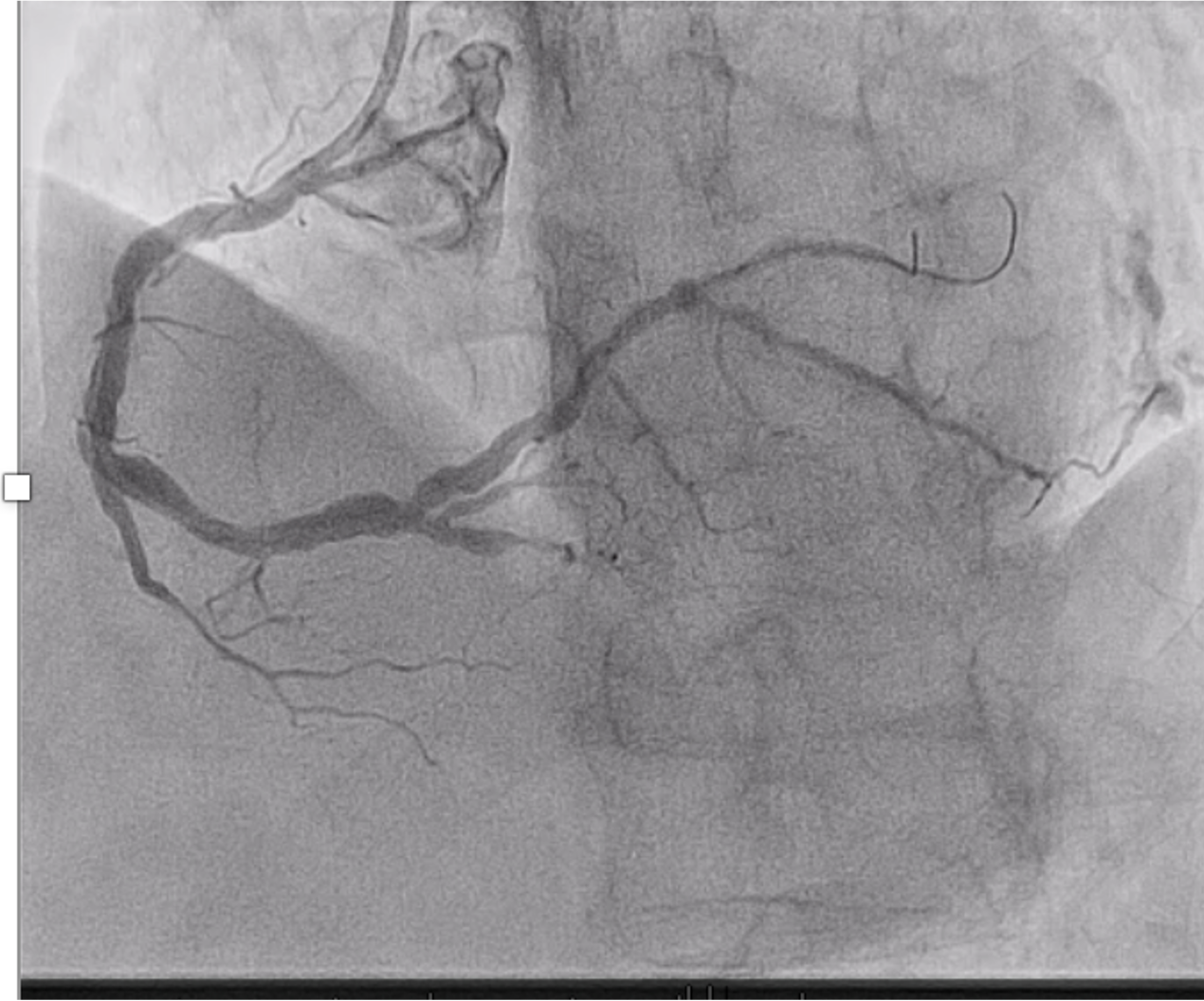
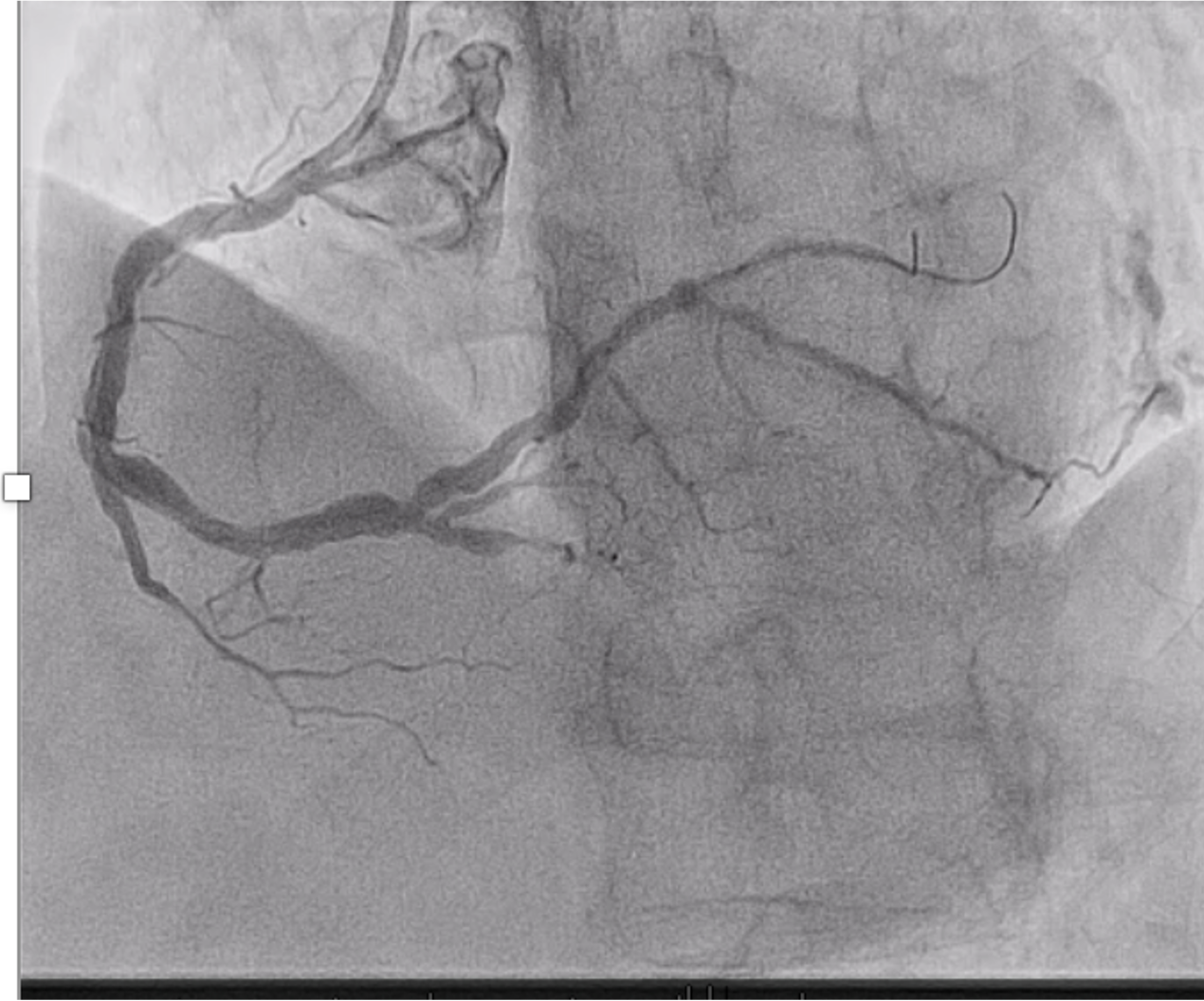
The repeated angiogram showed previous proximal LAD stent was patent. Right coronary artery is dominant and large. There is diffuse irregularities with midsegment 90%stenosis and distal ectasia with 80% stenosis. PLV sub-branch 90% stenosis and the PDA is occluded proximally.
Interventional Management
Procedural Step
The right radial artery was punctured, using a 6FR JL4 guiding catheter the RCA was engaged. Two Pilot 50 guidewires were passed into PLV and sub-branch. The PLV and sub-branch was predilated using Sprinter Legend 2.0mm x 15mm balloon followed by predilatation of the proximal to distal RCA with non compliant balloon Scoreflex 3.5 mmx 15 mm, noted difficulty passing the balloon to distal RCA. Therefore the proximal to mid RCA was predilated first. Subsequently balloon was able to pass to predilate the distal RCA. At this point,noted distal wire perforation in the PLV sub-branch with minimal contrast extravasation into myocardium. Patient was asymptomatic and hemodynamically stable. Therefore decision to treat proximal RCA to PLV lesions first with 3 overlapping drug coated balloon Sequent Please Neo 2.5mmx 20 mm and 3.5mm x 25mm inflated at 6 atm, 60 seconds.Subsequently, patient developed chest pain with ECG ST elevation in lead III. A repeat angiogram showed worsening contrast extravasation with echocardiography showing minimal pericardial effusion. The Sprinter Legend 2.5 mm x 15mm balloon was inflated in distal PLVfor 10 minutes. Post balloon deflation, showed the perforation was not sealed off, therefore the distal PLV was stented using covered stent PK Papyrus 2.5mmx15mm deployed at 8atm. Perforation had sealed off. Patient observed for 20minutes on table and repeat angiogram showed no more bleeding. The patient was sent to CCU for observation and discharged 2 days later.




Case Summary
In this case we depict two strategies to overcome distal wire perforation which was balloon inflation and deployment of covered stent. Coronary artery perforation is a rare complication of percutaneous coronary intervention, but it is associated with high morbidity and mortality. Given that the most common cause of distal vessel perforation is due to guidewire migration in a distal small calibre branch, therefore constant attention to the guidewire is of paramount importance.There are many modalities available to treat distal vessel perforation which are coiling, microsphres, thrombin injection, autologous blood clots, fat embolisation, using sutures to plug the perforation and covered stent.


