Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-132
Optical Coherence Tomography Guided Circumflex Artery Stenting Complicated by Left Main Occlusion Treated by Intravascular Ultrasound Guided Left Main and Left Descending Artery Stenting
By Farhat Fouladvand, Mauro Musmeci, Guido Belli
Presenter
Farhat Fouladvand
Authors
Farhat Fouladvand1, Mauro Musmeci1, Guido Belli1
Affiliation
Clinica San Carlo, Italy1,
View Study Report
TCTAP C-132
CORONARY - Complications (Coronary)
Optical Coherence Tomography Guided Circumflex Artery Stenting Complicated by Left Main Occlusion Treated by Intravascular Ultrasound Guided Left Main and Left Descending Artery Stenting
Farhat Fouladvand1, Mauro Musmeci1, Guido Belli1
Clinica San Carlo, Italy1,
Clinical Information
Patient initials or Identifier Number
BG 473-2022
Relevant Clinical History and Physical Exam
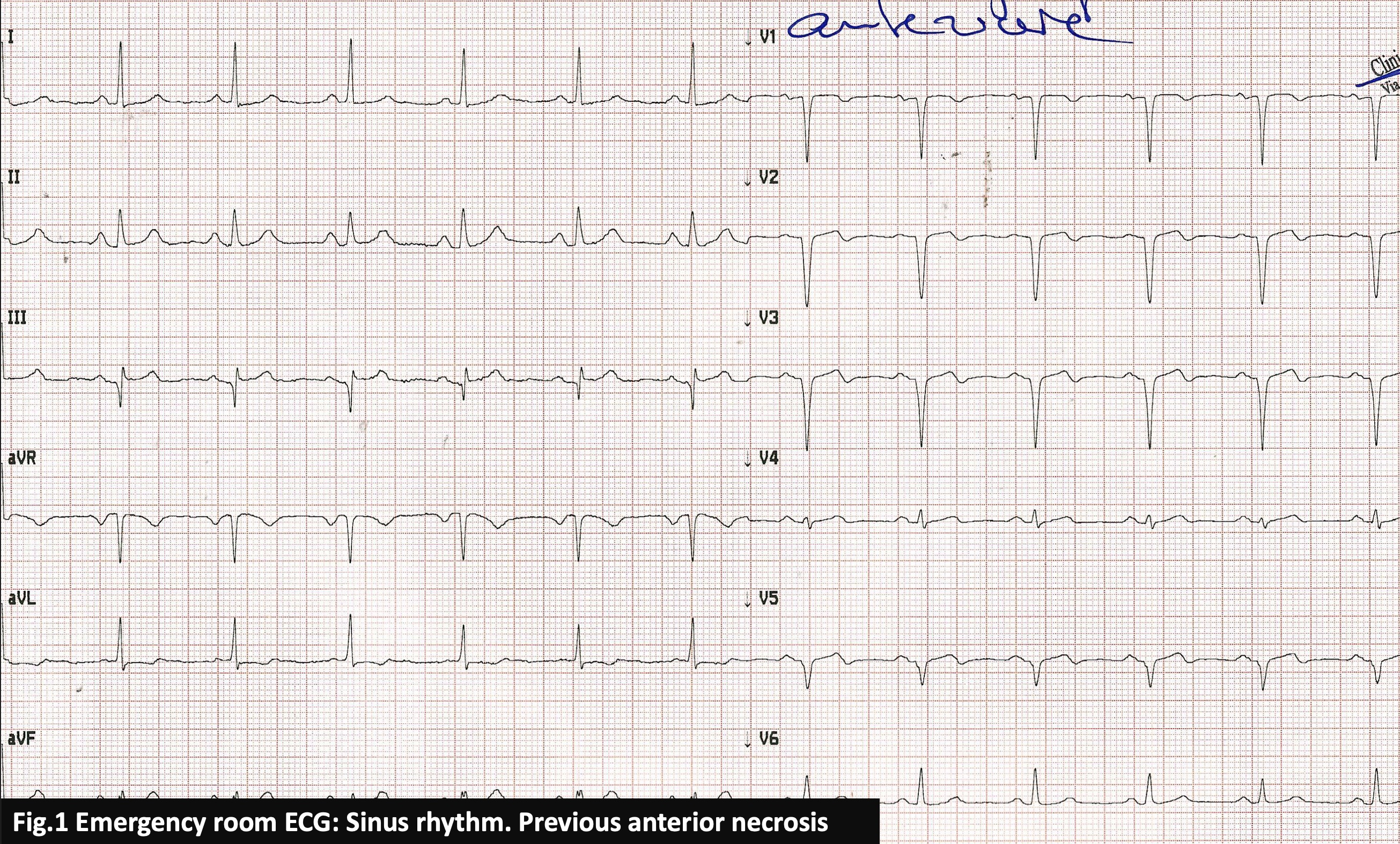
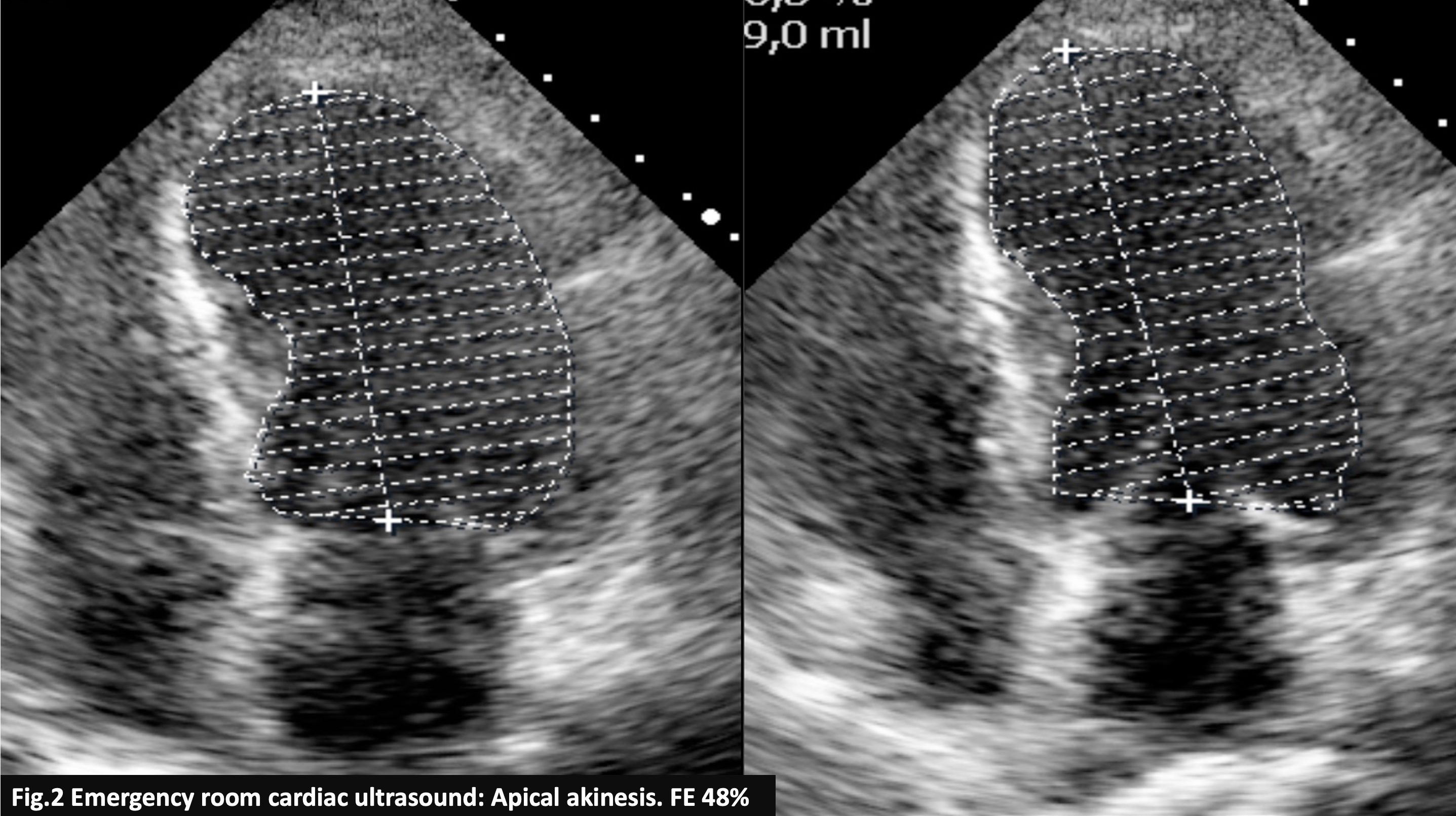
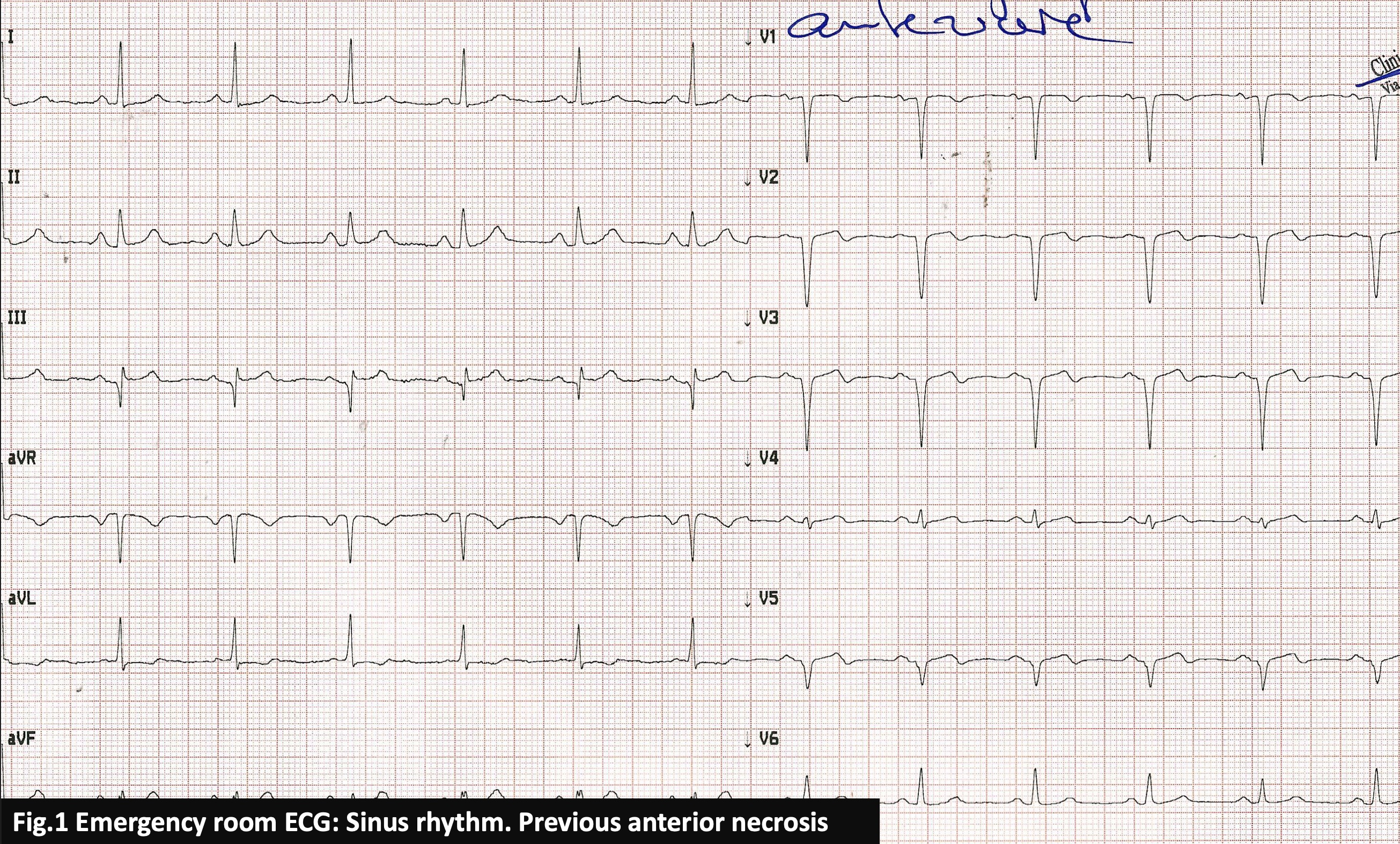
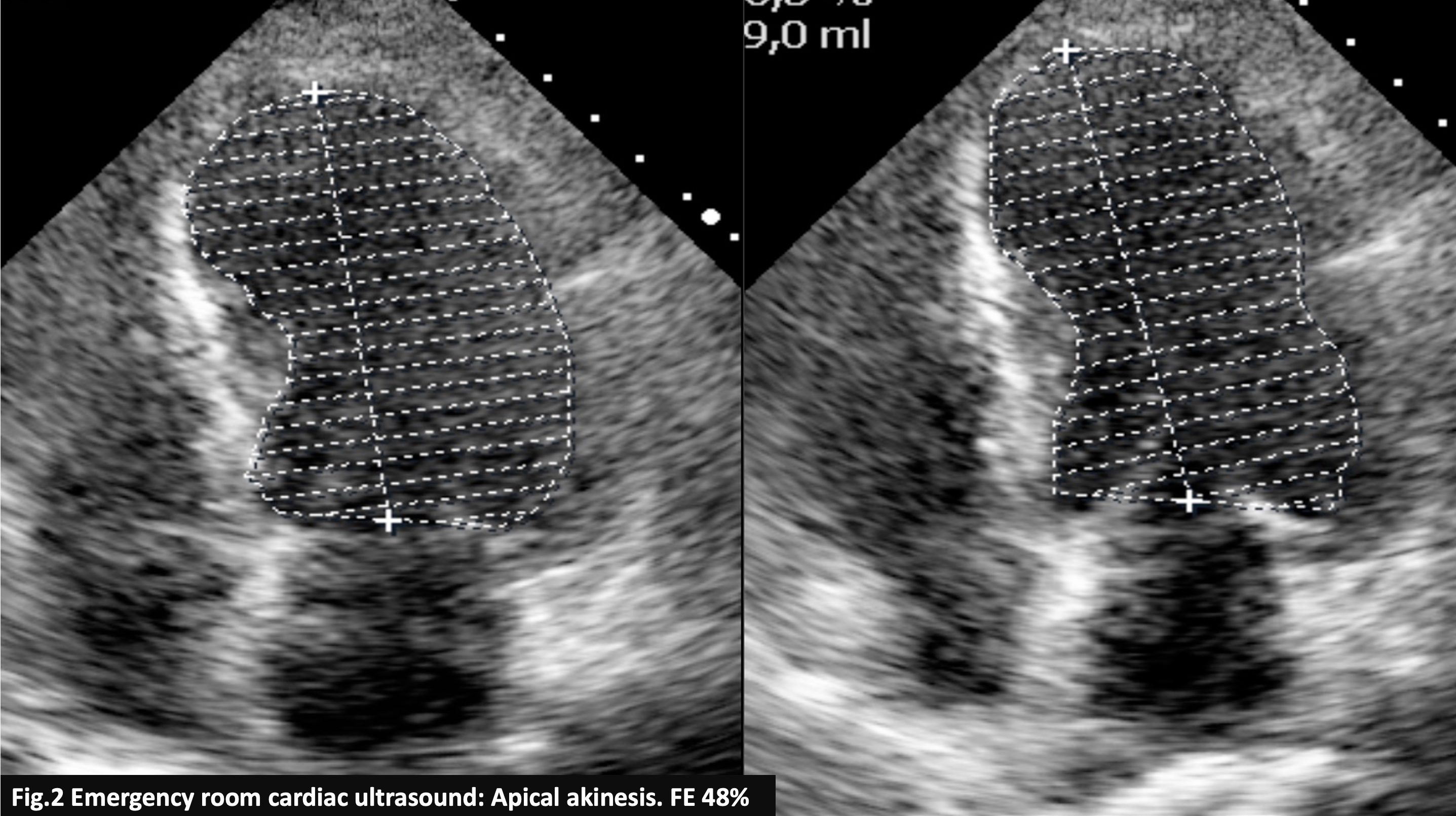
A 69-year-old woman with hypertension and dyslipidemia with no history of heart disease is described. Her cardiac history started in 2010 with anterior STEMI treated with angioplasty and stent placement on mid LAD. In 2011 she was recovered for unstable angina that was treated with two stents. Her basal ECG demonstrate transmural anterior necrosis and her cardiac echo shows apical akinesia with EF 48%.Because of the onset of intensive chest pain at rest she came to our emergency department.
Relevant Test Results Prior to Catheterization
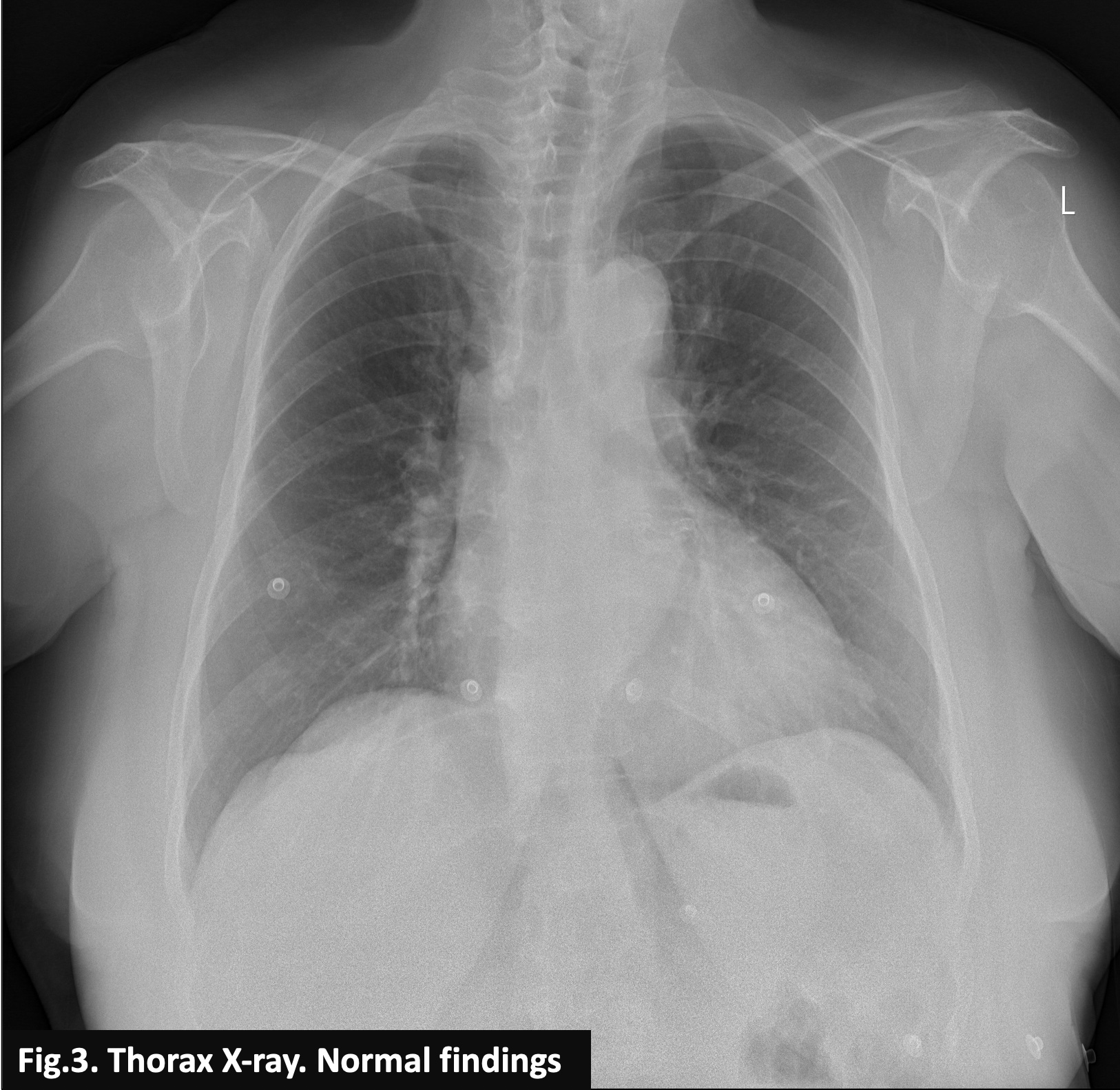
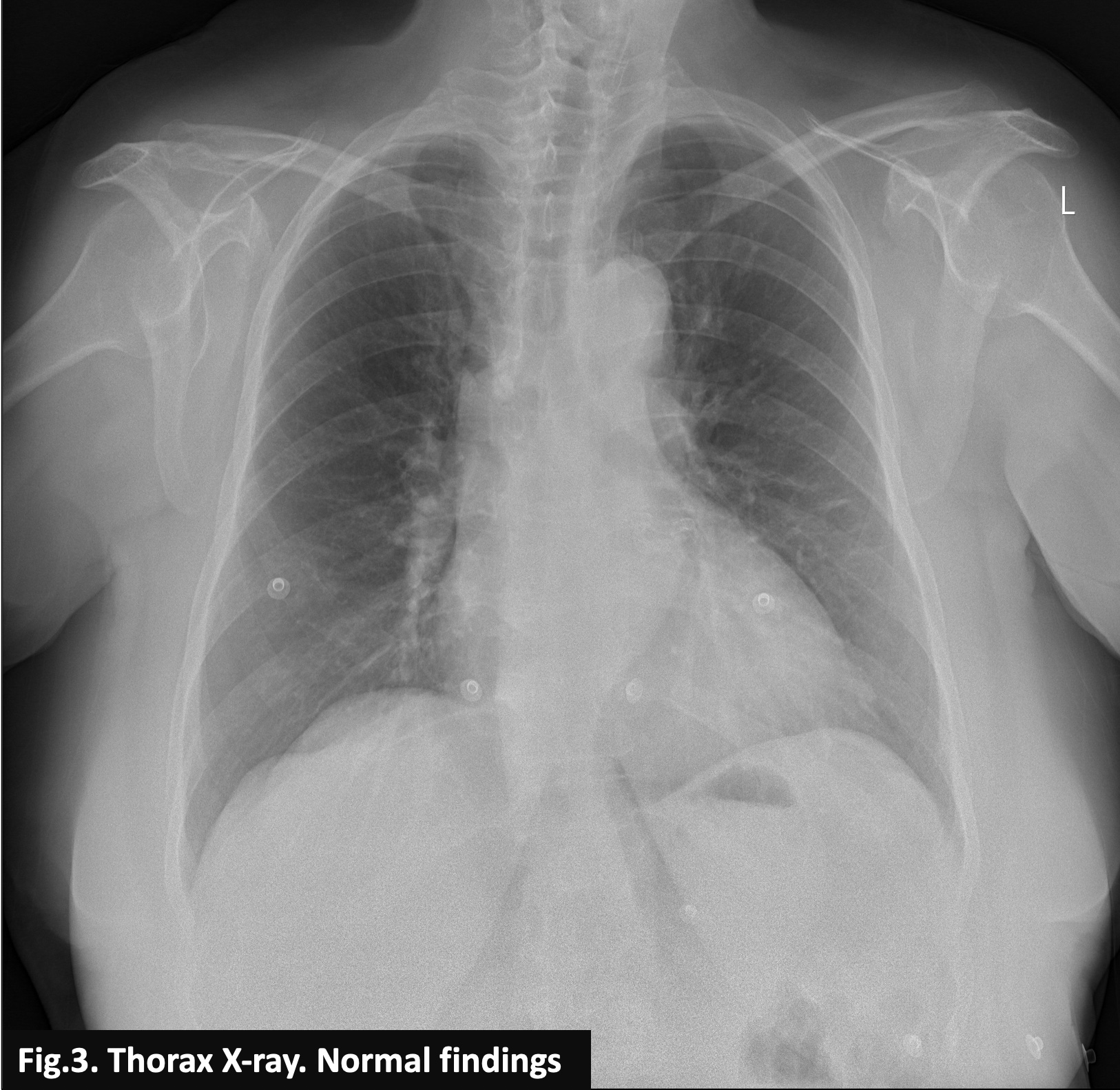
At admission in ER her ECG and eco were unchanged compared to the previous exams and her thoracic X-ray (Fig.3) was normal. She had increasing cardiac markers, particularly her TnI-HS, which reached 788 pg/mL at her second test. She was admitted in cardiology department and coronary angiography was scheduled for the next morning. During the night she was completely asymptomatic without further increase in cardiac markers and new ECG changes.
Relevant Catheterization Findings
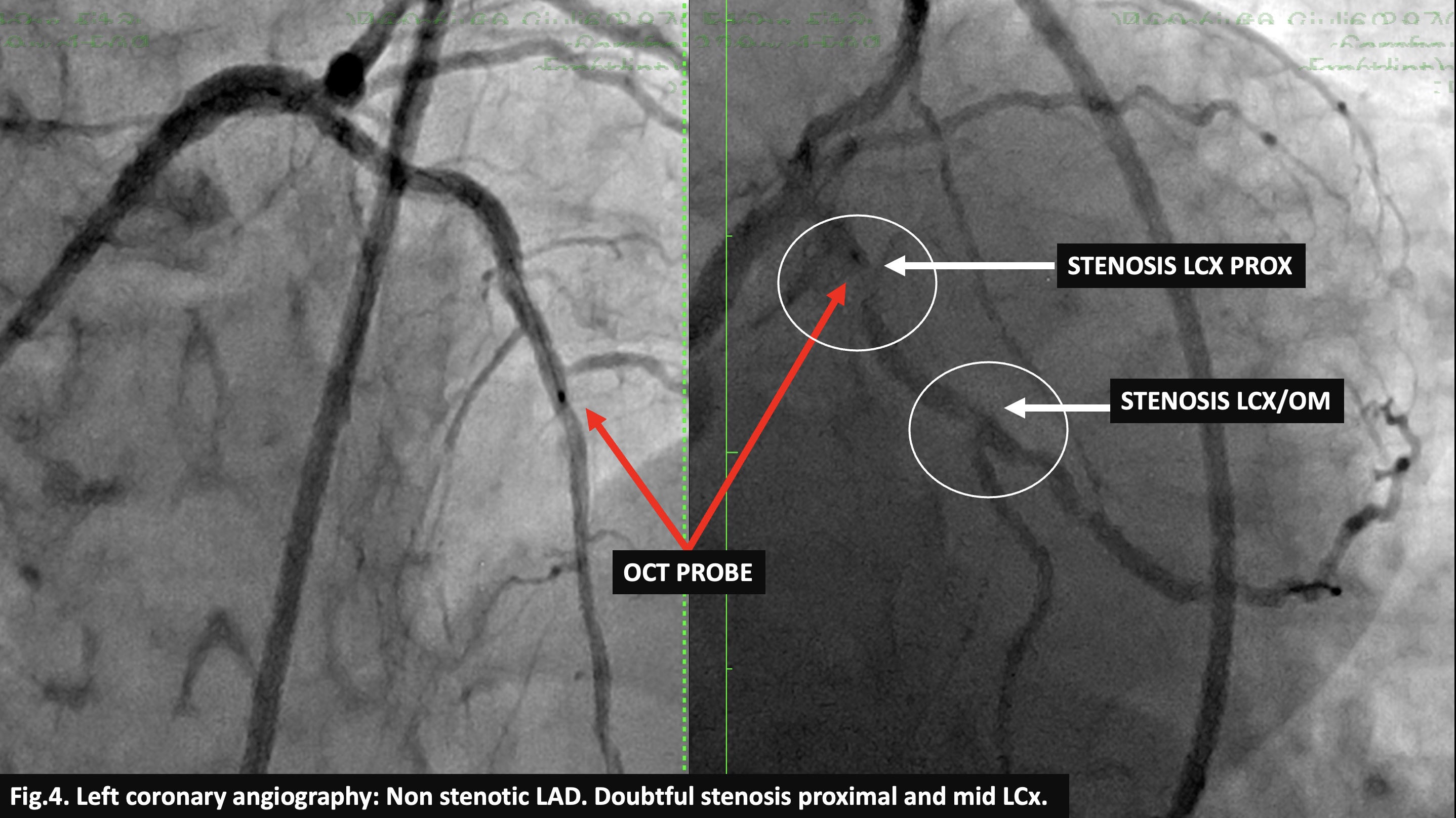
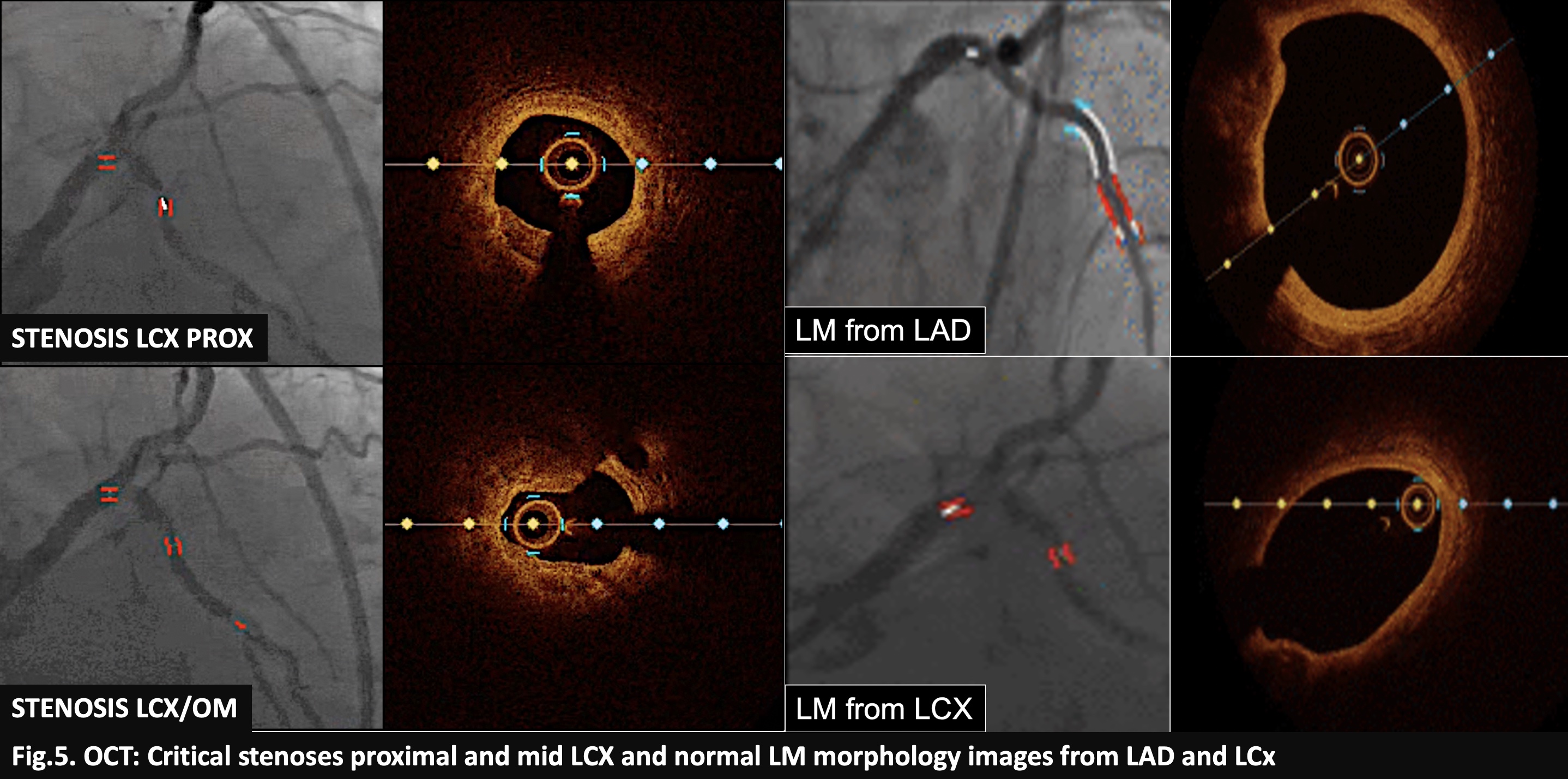
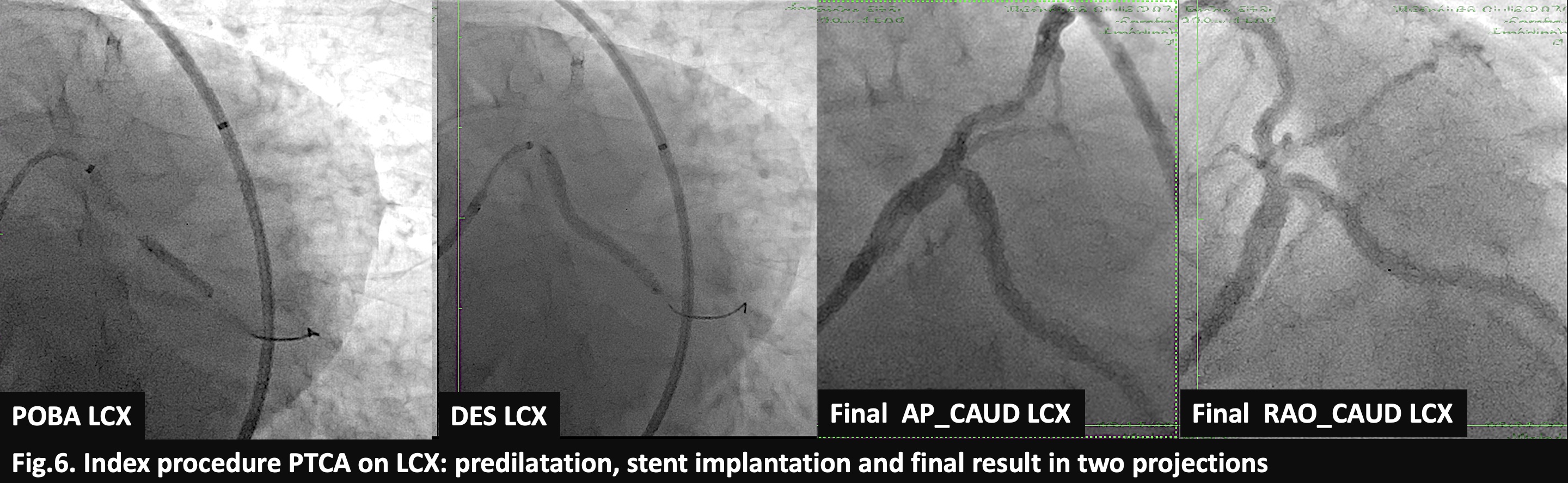
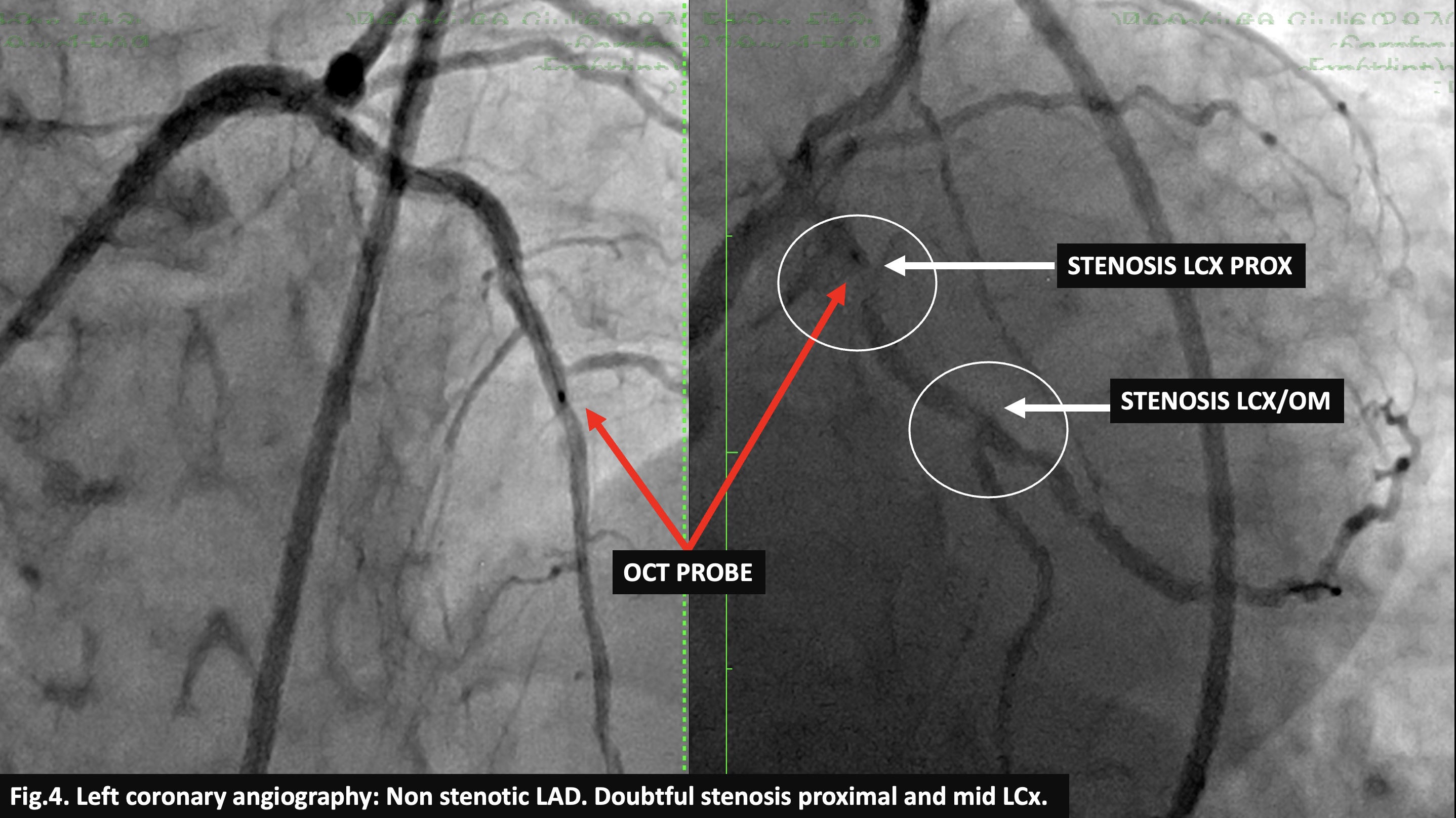
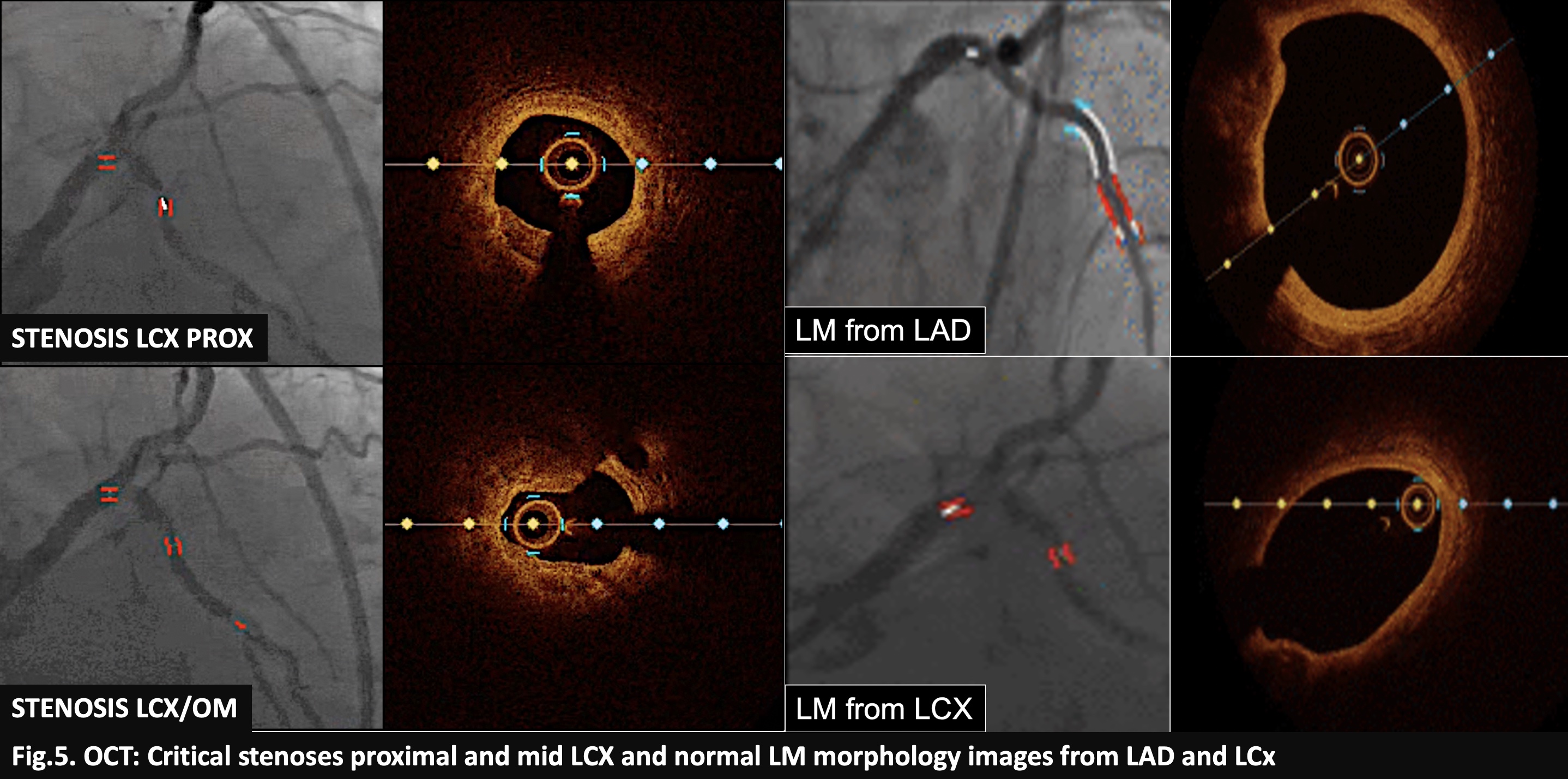
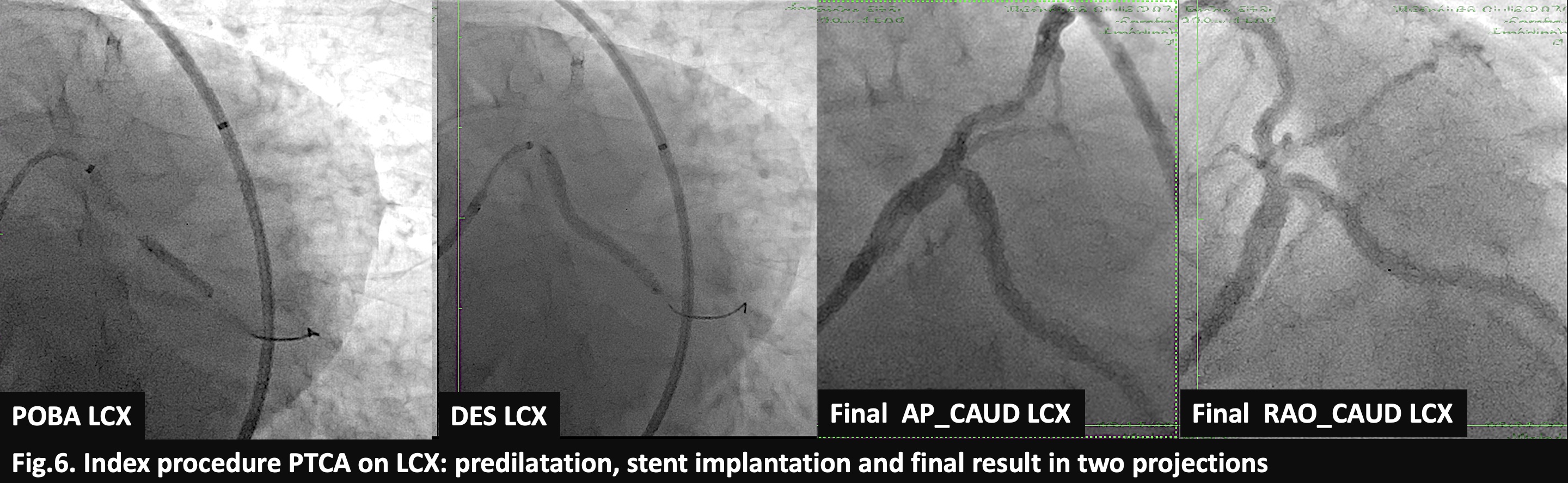
Coronarography from the femoral artery (Fig. 4) demonstrated RCA and LAD free of stenosis and doubtful stenoses at proximal and mid LCX. At OCT (Fig. 5) both stenoses on LCX were critical while the left main was normal. GuideLiner enabled us to pre-dilate the stenoses on LCX and we placed a long 3,0 x 38 mm Zotarolimus eluting stent obtaining good angiographic results (Fig. 6). The final OCT wasn't performed because of of an inability to pass with the probe the proximal stent edge.
Interventional Management
Procedural Step
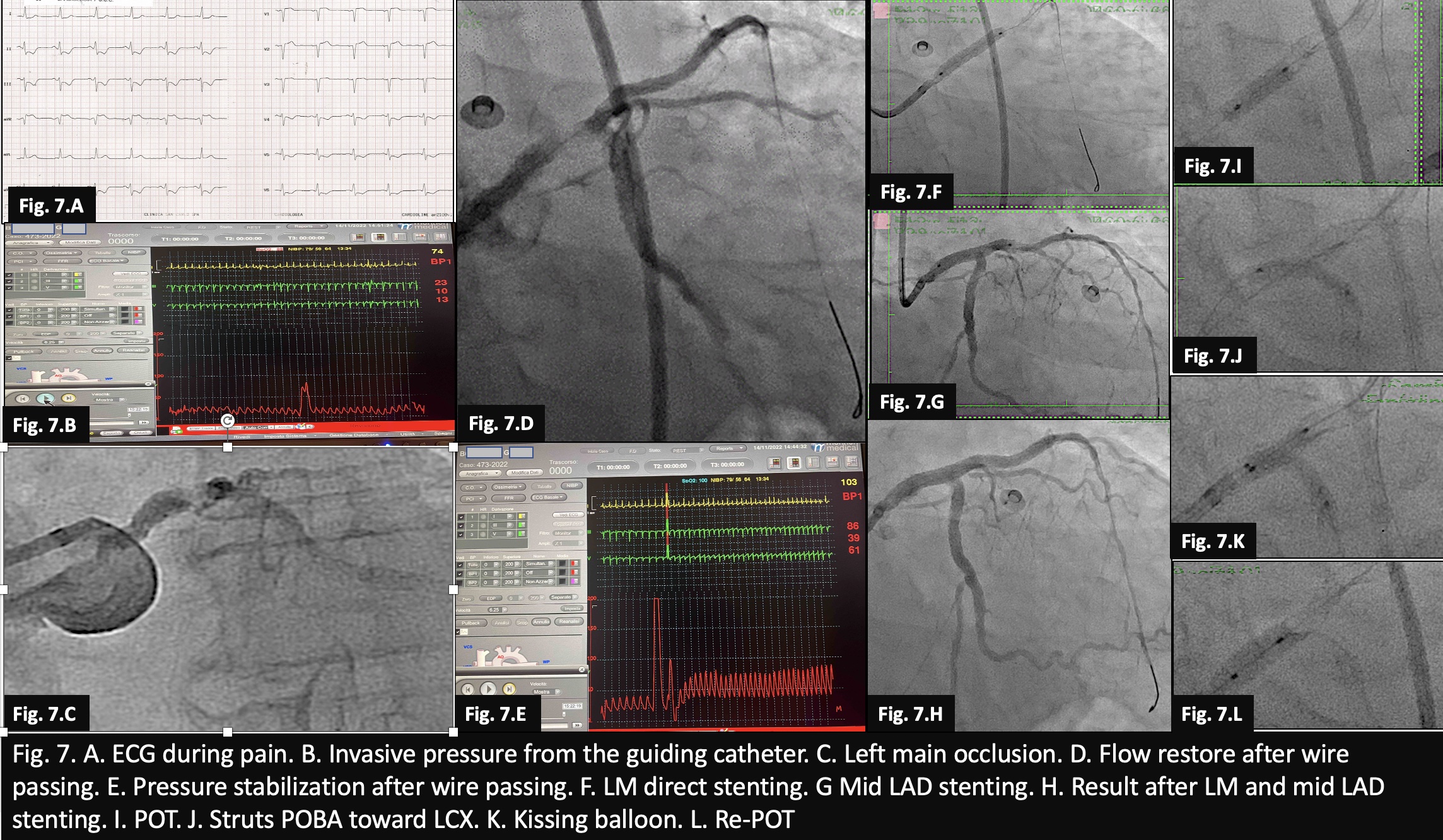
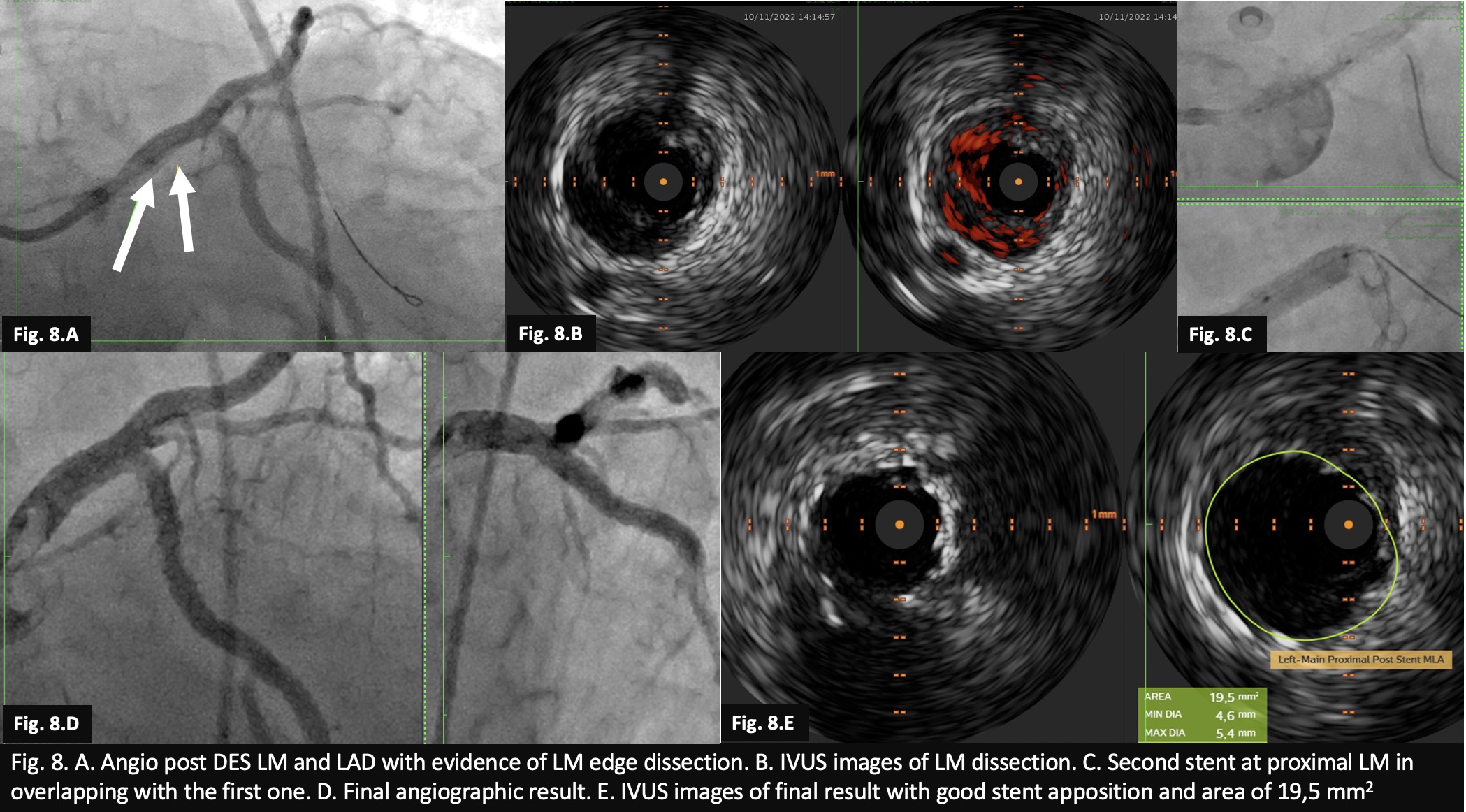
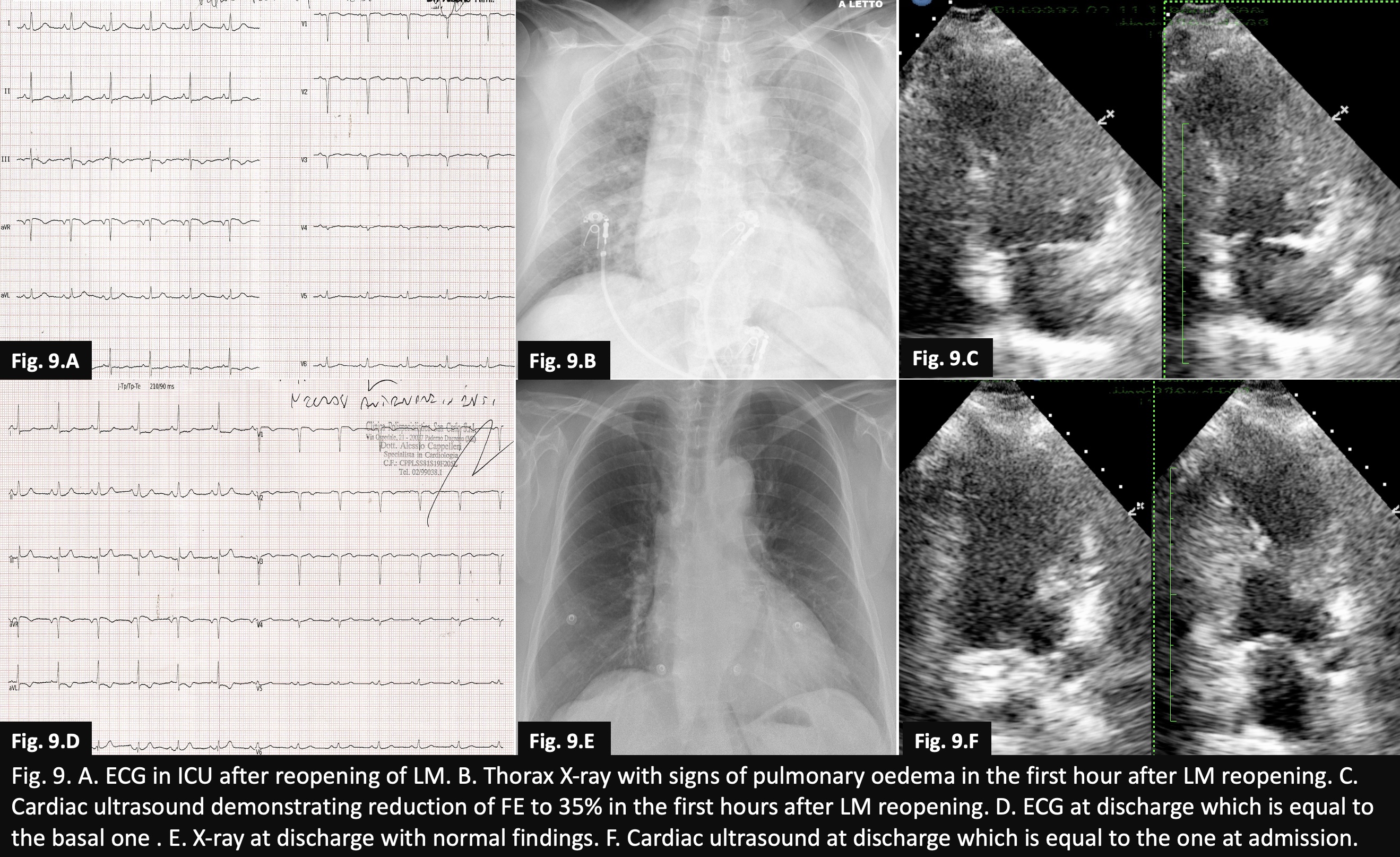
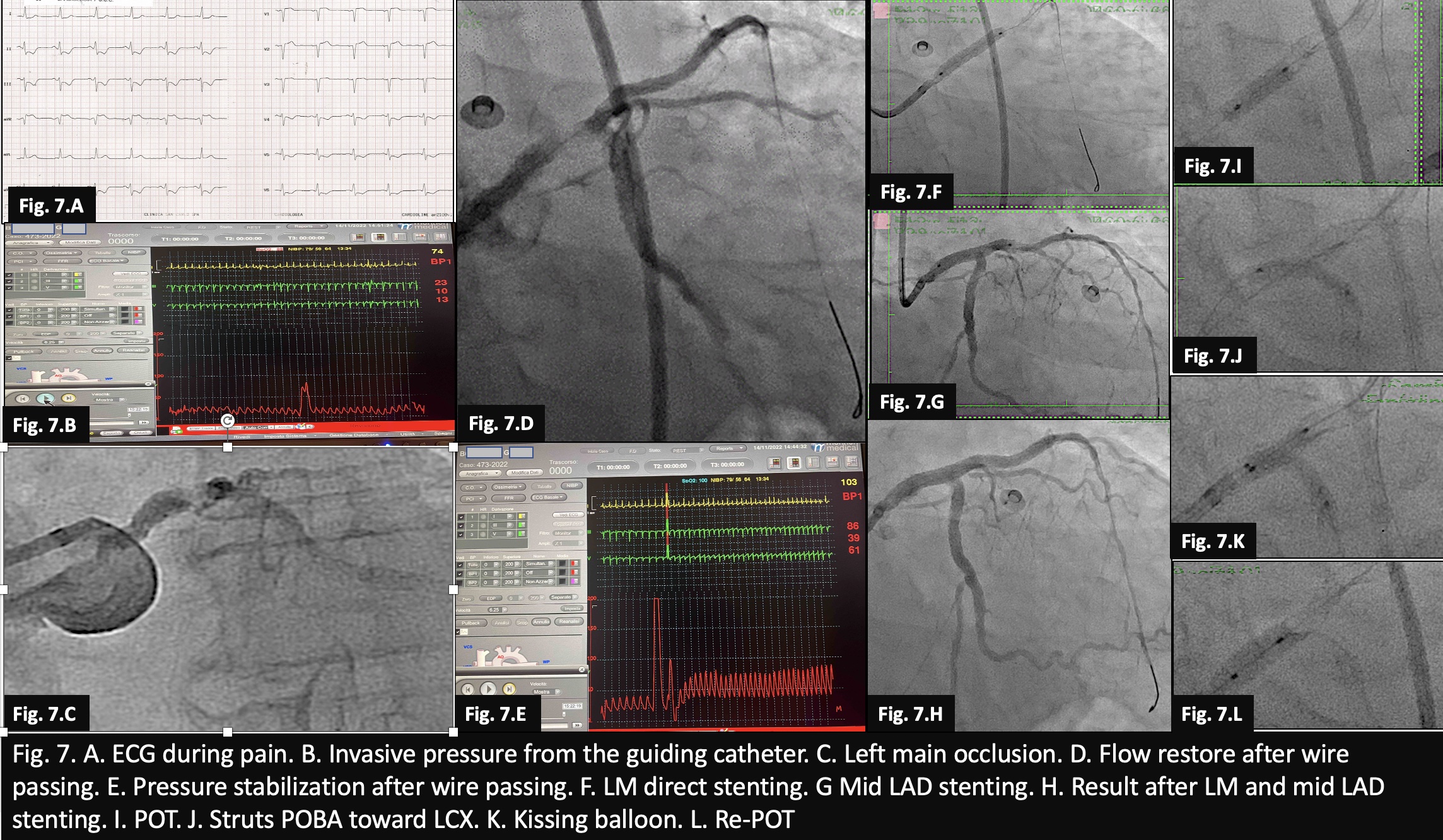
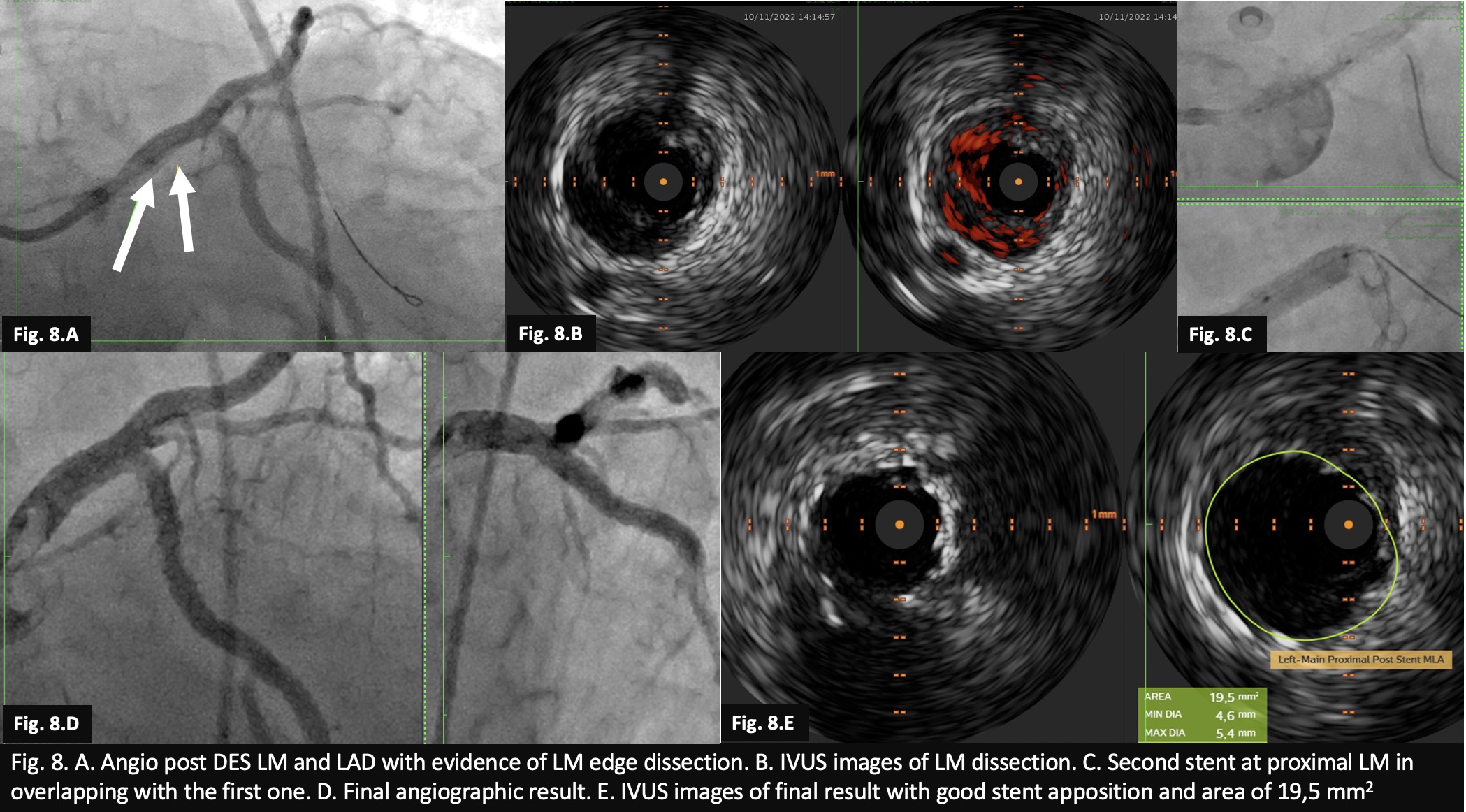
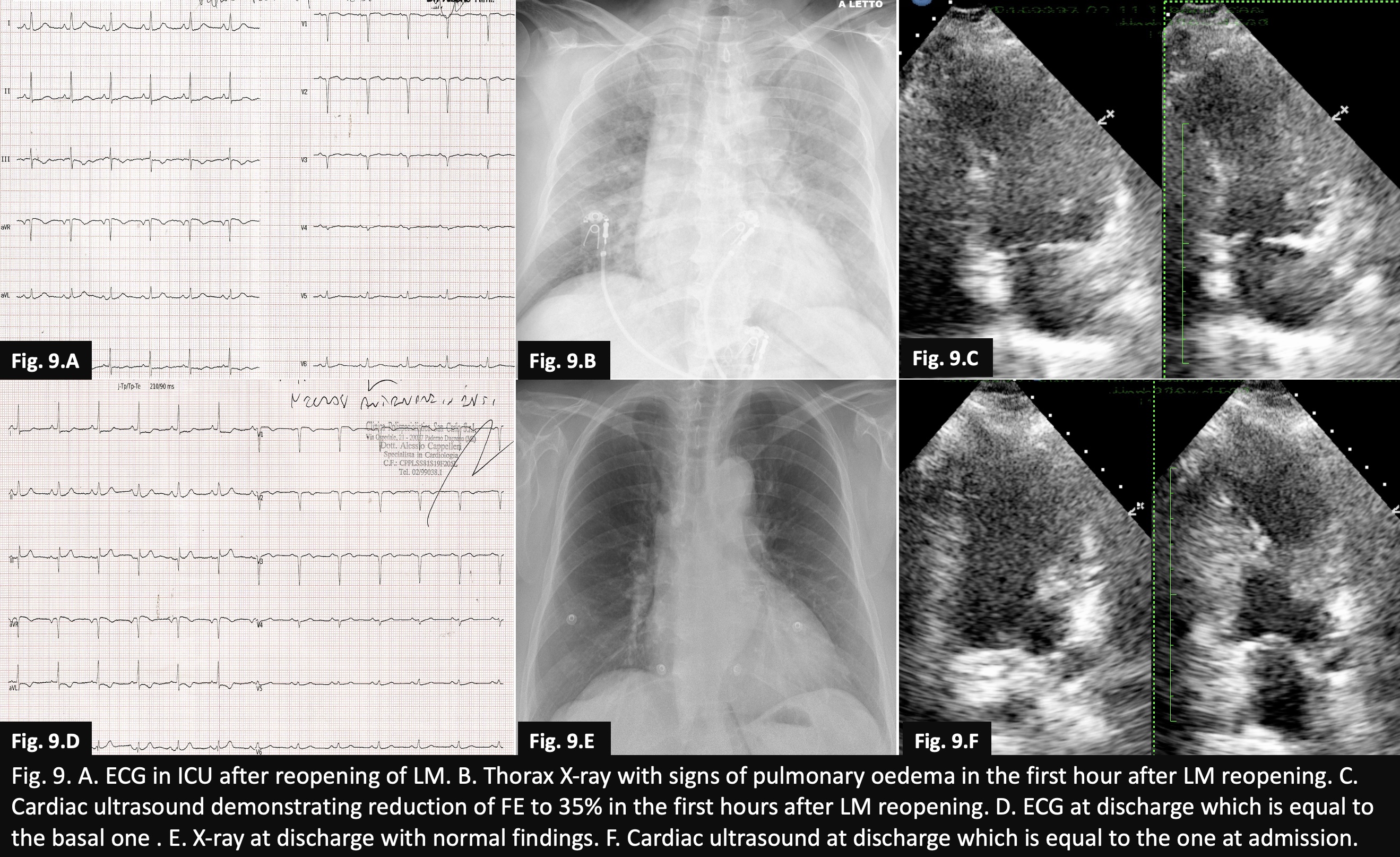
A few minutes later she complained of chest pain with anterior ST depressions and ST elevation in aVR. The patient was transferred to the cath lab where the invasive pressure was 30/10 mmHg and the angio showed LM occlusion (Fig 7. A-C). With the passage of the guidewire the flow was restored and blood pressure rose to 85/40 mmHg (Fig. 7. D, E). Direct stenting of the LM 3,5 x 22 mm and mid LAD 3,0 x 22 mm was done (Fig. 7. F-H). Procedure was followed by POT, struts POBA toward LCX, kissing balloon and re-POT (Fig. 7. I-L) with good angio result but with LM dissection at proximal edge of the stent, confirmed by IVUS (Fig. 8. A, B). A third stent 5,0 x 12 mm was placed at the LM ostium in overlapping with the previous one (Fig. 8. C) with excellent angiographic and IVUS result (Fig. 8. D,E). All stents were Zotarolimus eluting. The patient was then transferred in CCU with normal blood pressure, free of pain, but dyspneic. ECG was without ST changes, while at X-ray pulmonary oedema was present, the FE was 35%, significantly reduced compared to the basal exam (Fig. 9. A-C) and the troponin TnI-HS rose to 25453 pg/mL. Treatment with CPAP, diuretics, antibiotics, DAPT, low dose vasodilators and beta-blockers and high dose statins was effective. At the 5th day, the patient was discharged asymptomatic, and his X-ray, ECG and echo were comparable to those taken on admission (Fig. 9. D-F).
Case Summary
Our case clearly demonstrates that sometimes even well-planned procedures with imaging can lead to life-threatening complications. In managing such devastating situations where time is of the essence for the patient's salvation and reducing organ damage, the key is the organized and synchronized behaviour of all personnel. Crucial is the operator's experience in confronting and successfully treating such dramatic situations.


