Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-120
A Challenging Complication of Percutaneous Coronary Intervention – Stent Edge Dissection and Intimal Hematoma Formation
By Withanage Narmada Madhubhashini Perera, Gamini Galappaththy, Chamidi Isanka Hasani Siriwardane, Naigalage Upananda Ajith Dissanayake
Presenter
Withanage Narmada Madhubhashini Perera
Authors
Withanage Narmada Madhubhashini Perera1, Gamini Galappaththy1, Chamidi Isanka Hasani Siriwardane1, Naigalage Upananda Ajith Dissanayake1
Affiliation
The National Hospital of Sri Lanka, Sri Lanka1,
View Study Report
TCTAP C-120
CORONARY - Complications (Coronary)
A Challenging Complication of Percutaneous Coronary Intervention – Stent Edge Dissection and Intimal Hematoma Formation
Withanage Narmada Madhubhashini Perera1, Gamini Galappaththy1, Chamidi Isanka Hasani Siriwardane1, Naigalage Upananda Ajith Dissanayake1
The National Hospital of Sri Lanka, Sri Lanka1,
Clinical Information
Patient initials or Identifier Number
MR R.M.
Relevant Clinical History and Physical Exam
A 52 year old diagnosed patient with hypertension, dyslipidemia and ischemic heart disease got admitted to the hospital for further interventions. Two months prior to the current admission, he got Non ST elevation myocardial infarction which was managed medically. During the past two months he had angina on moderate exertion. He was hemodynamically stable on admission and systemic examination did not reveal significant findings.
Relevant Test Results Prior to Catheterization
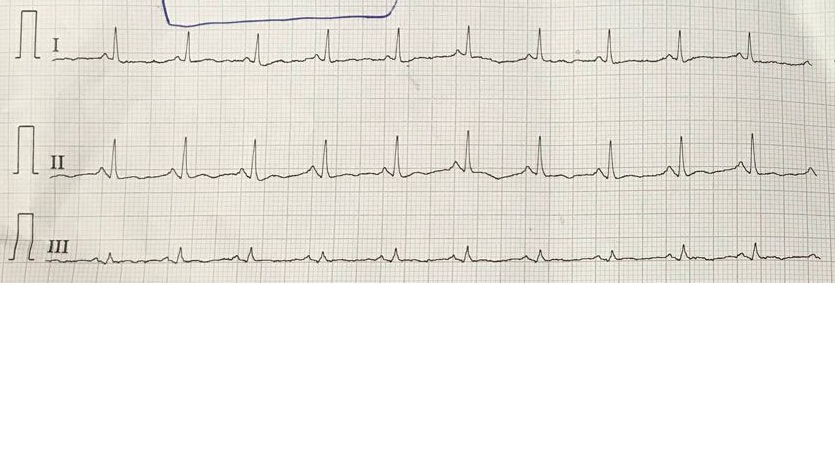
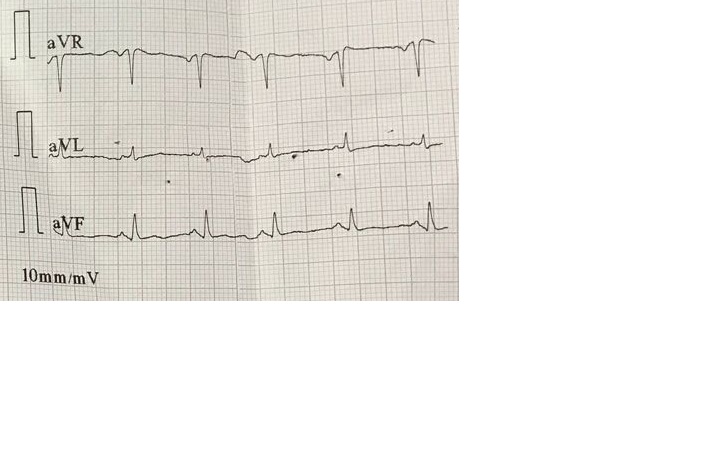
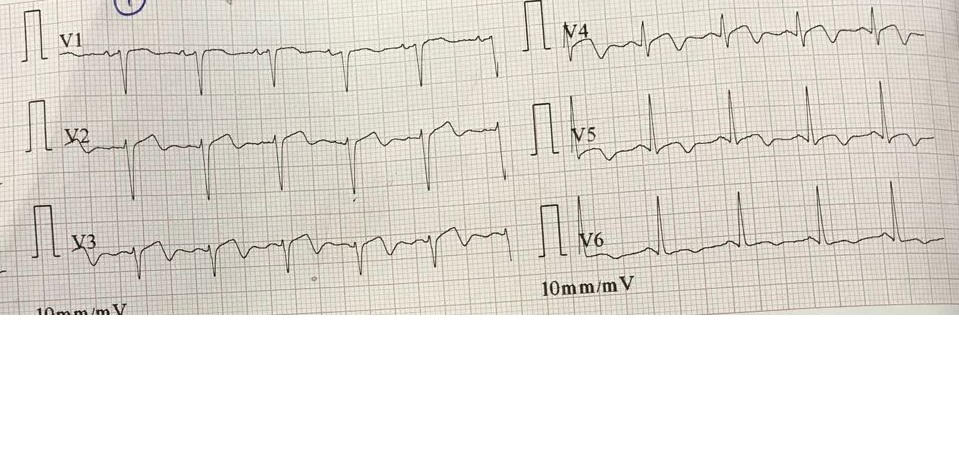
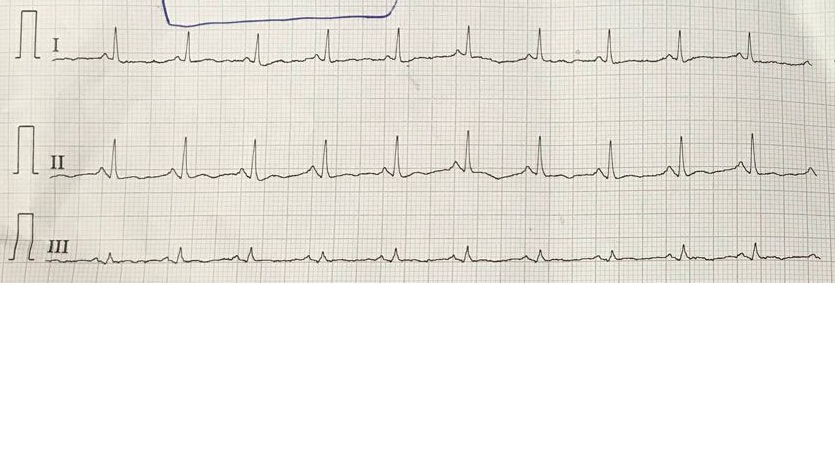
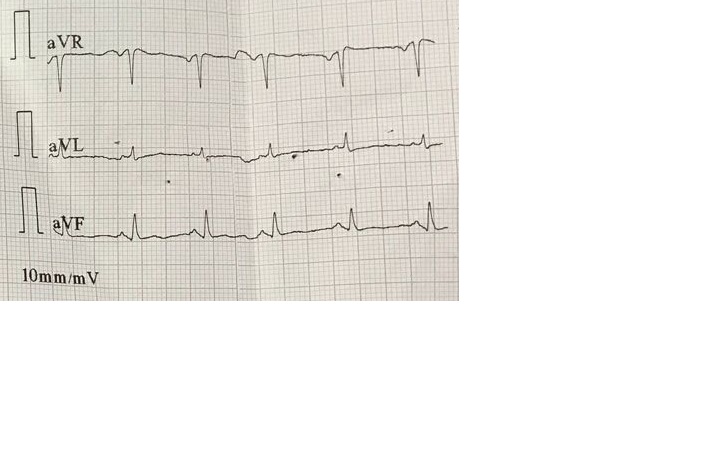
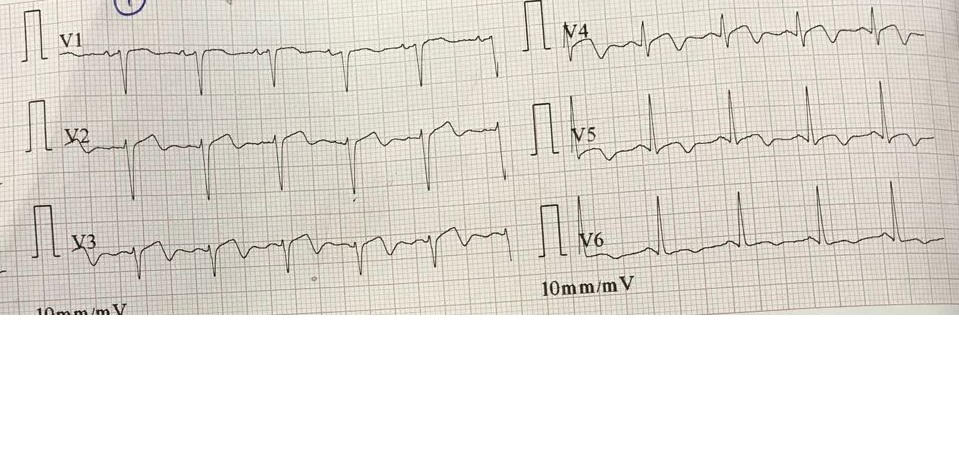
His electrocardiogram showed type A Wellen's pattern. His ejection fraction was 50% with mild anterior hypokinesia. Other than that his trans-thoracic echocardiogram was normal. His hematological and biochemical investigations were normal.
Relevant Catheterization Findings
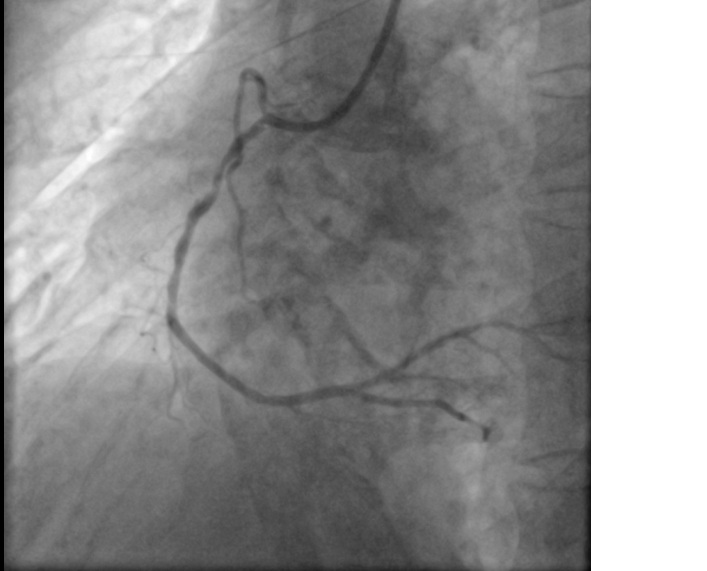
He had dominant right coronary artery with proximal to mid vessel long segment moderate to severe disease, maximum 95% stenosis. In the left side there was a 95% stenosis in the distal left main coronary artery. Left circumflex artery had 99% ostial lesion followed by proximal to mid vessel long segment severe disease, maximum 90% stenosis. Second obtuse marginal branch had ostio-proximal 80% stenosis and left anterior descending artery had ostial 80% stenosis.


Interventional Management
Procedural Step
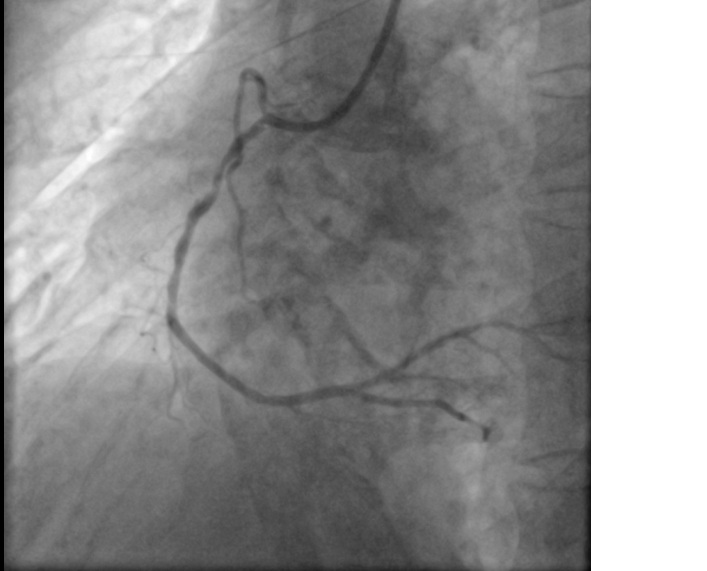
Right coronary artery was stented directly with 3 X 48 mm drug eluting stent. Then distal left circumflex artery stented with 2.75 X 28 mm drug eluting stent. Proximal circumflex artery stented from ostium with 3 X 23 mm drug eluting stent and it was overlapped with the distal stent. Left main coronary artery to left anterior descending artery was stented with 3.5 X 12 mm drug eluting stent. Post procedure coronary angiogram showed good result with TIMI 3 flow. Ten hours after the procedure patient developed ischemic type of chest pain and electrocardiogram showed ST segment elevation in aVR with wide spread horizontal ST depression. Check coronary angiogram revealed 99% stenosis in left anterior descending artery just distal to the stent. It did not resolve with intra coronary nitroglycerin trinitrate. We stented the stenotic segment with 3 X 33 mm drug eluting stent and achieved TIMI 3 flow.
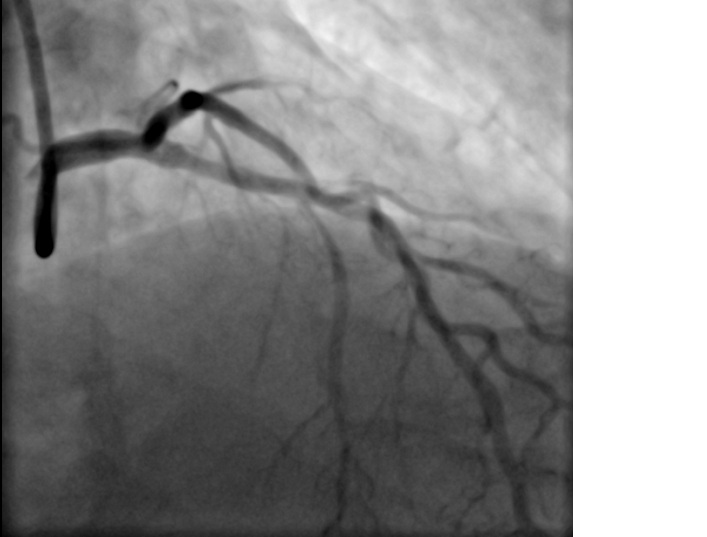
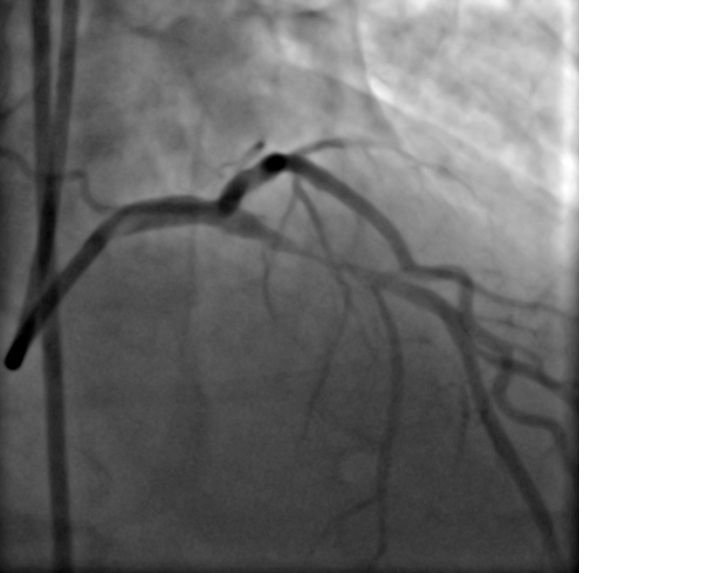

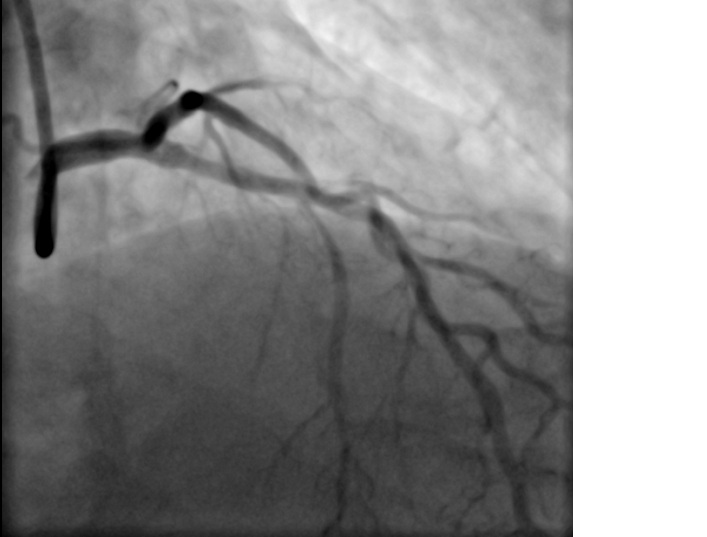
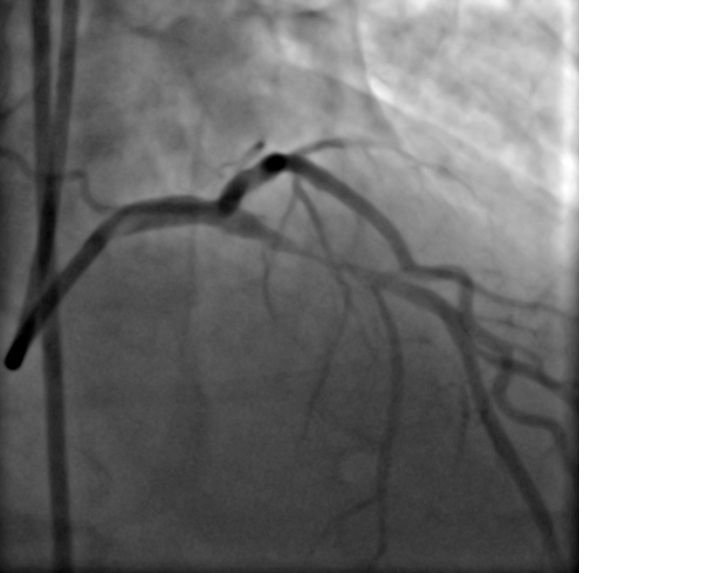

Case Summary
During retrospective analysis of the coronary angiography we found, post stent edge dissection in the left anterior descending artery. Therefore most likely cause for the post stent critical stenosis was medial dissection causing intramural hematoma as there was no thrombus burden within the lumen. Since it was an emergency we were unable to perform intravascular ultrasound [IVUS].


