Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-007
Catastrophic Nightmare in an ACS Patient With Calcified and Torturous LM Bifurcation Lesion
By Shu Yu Tang, Jen-Kuang Lee
Presenter
Shu Yu Tang
Authors
Shu Yu Tang1, Jen-Kuang Lee1
Affiliation
National Taiwan University Hospital, Taiwan1,
View Study Report
TCTAP C-007
CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS)
Catastrophic Nightmare in an ACS Patient With Calcified and Torturous LM Bifurcation Lesion
Shu Yu Tang1, Jen-Kuang Lee1
National Taiwan University Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
5162199
Relevant Clinical History and Physical Exam
A 67-year-old woman had undergone routine hemodialysis thrice a week and had a history of hypertension, asthma, heavily treated peripheral vascular disease, paroxysmal atrial fibrillation and heavily treated coronary artery disease. She developed chest pain and diaphoresis in a routine hemodialysis course and was sent to ED room presenting as bradycardia (PR 49) without delirium, hypotension or desaturation at ED room. No crackles or wheezes were been heard. Her extremities are warm.
Relevant Test Results Prior to Catheterization
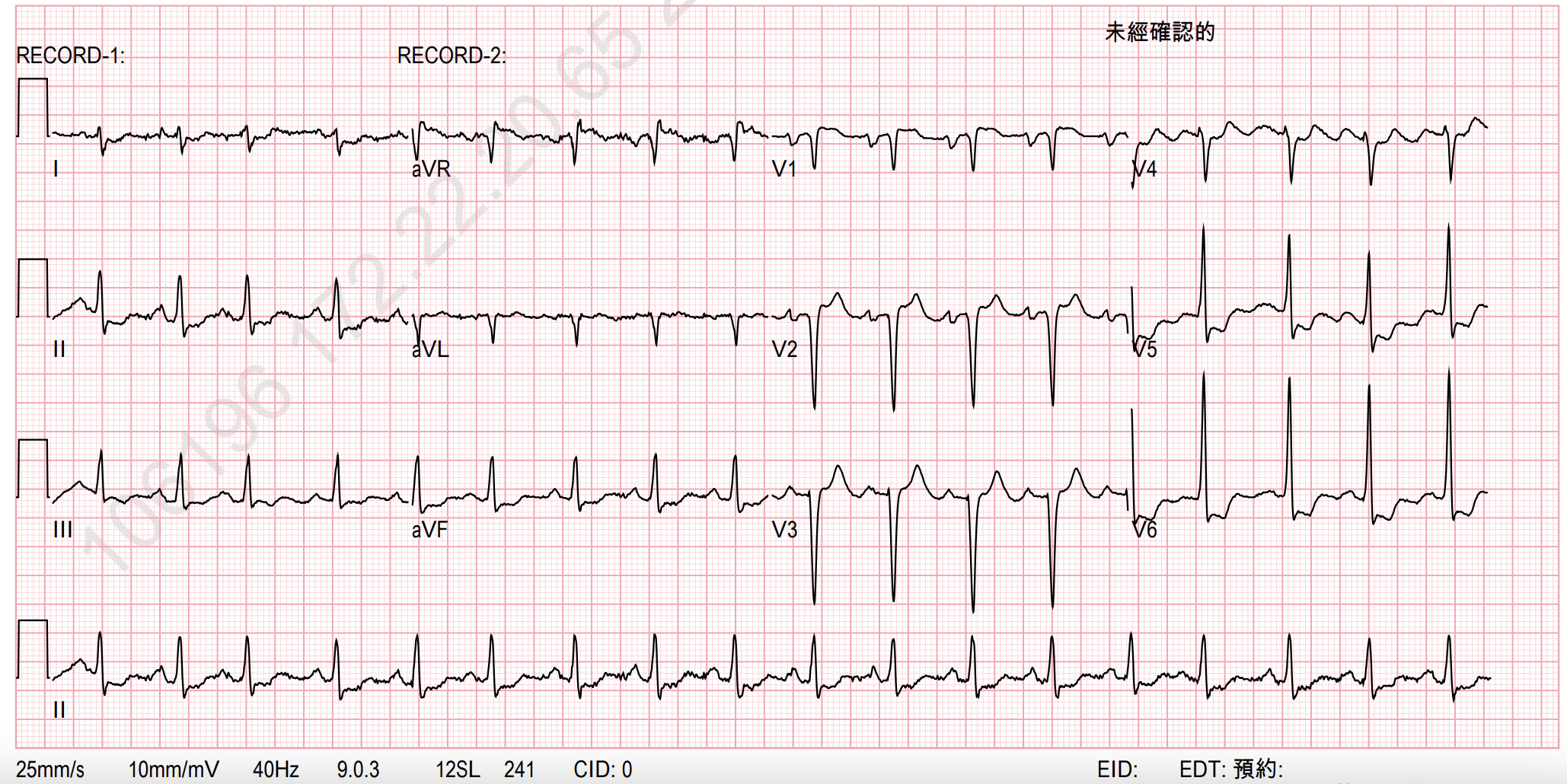
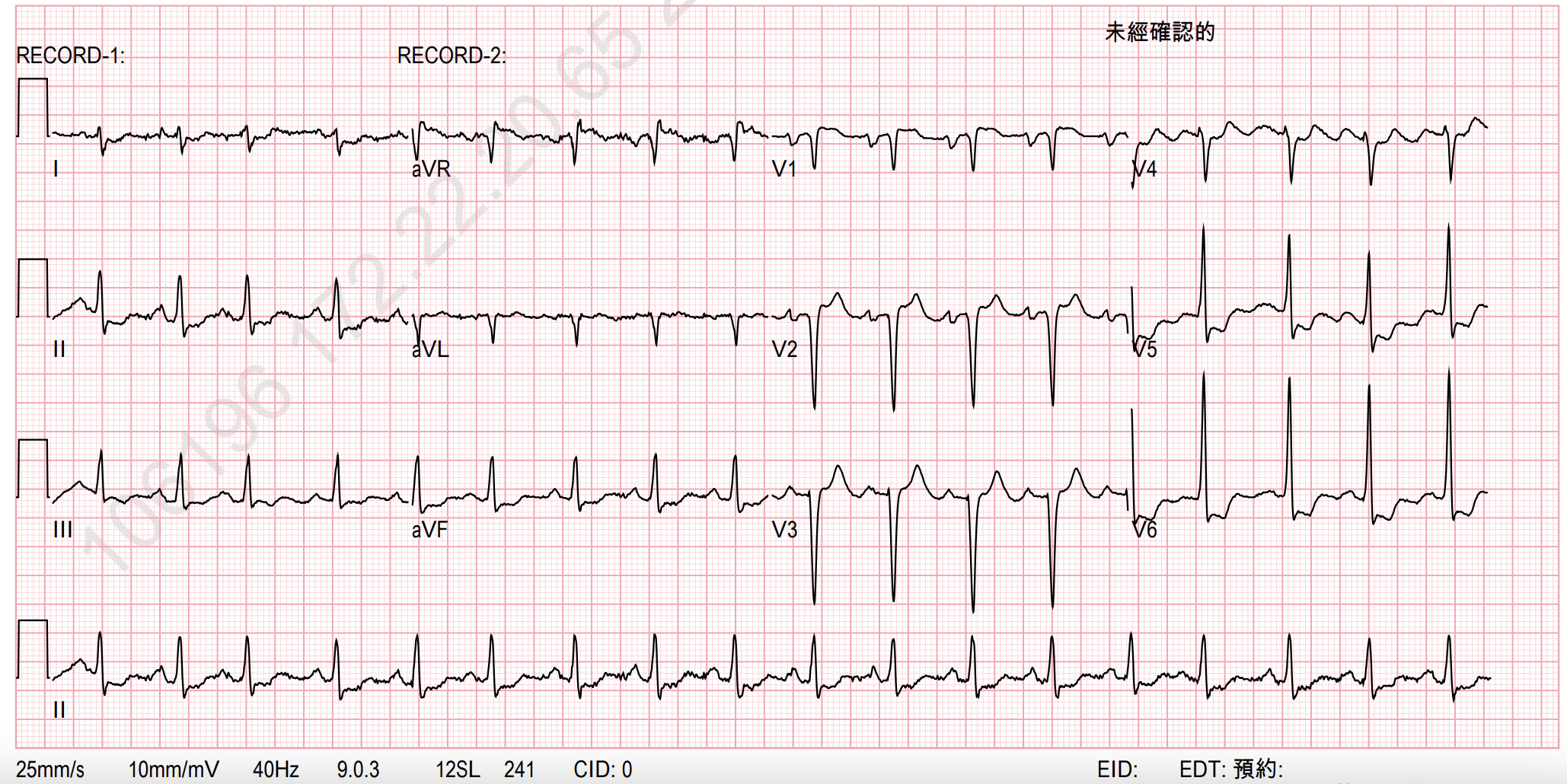
She had underwent angiogram and intervention in 2020, when drug eluting stents were depolyed at LAD chronic total occlusion and RCA after performing rotational atherectomy. Initial lab data showed elevated troponin-T up to 4391ng/L, CK 94U/L, and CK-MB 9.85ng/mL. The ECG showed normal sinus rhythm at ED, but it turned to STD at lead II, III, aVF, V5, and V6, and STE at aVR after the first session of hemodialysis at ICU.
Relevant Catheterization Findings
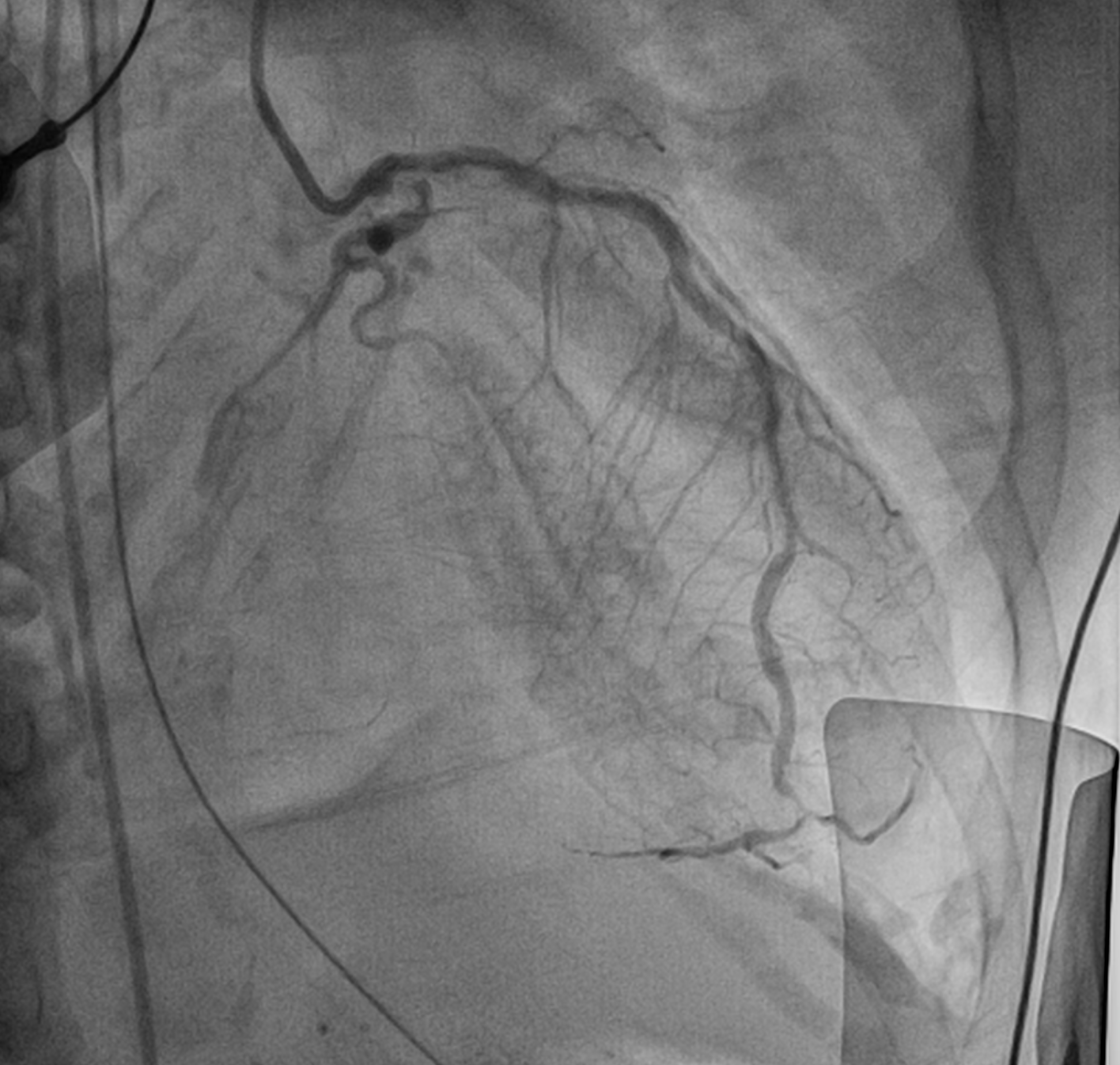
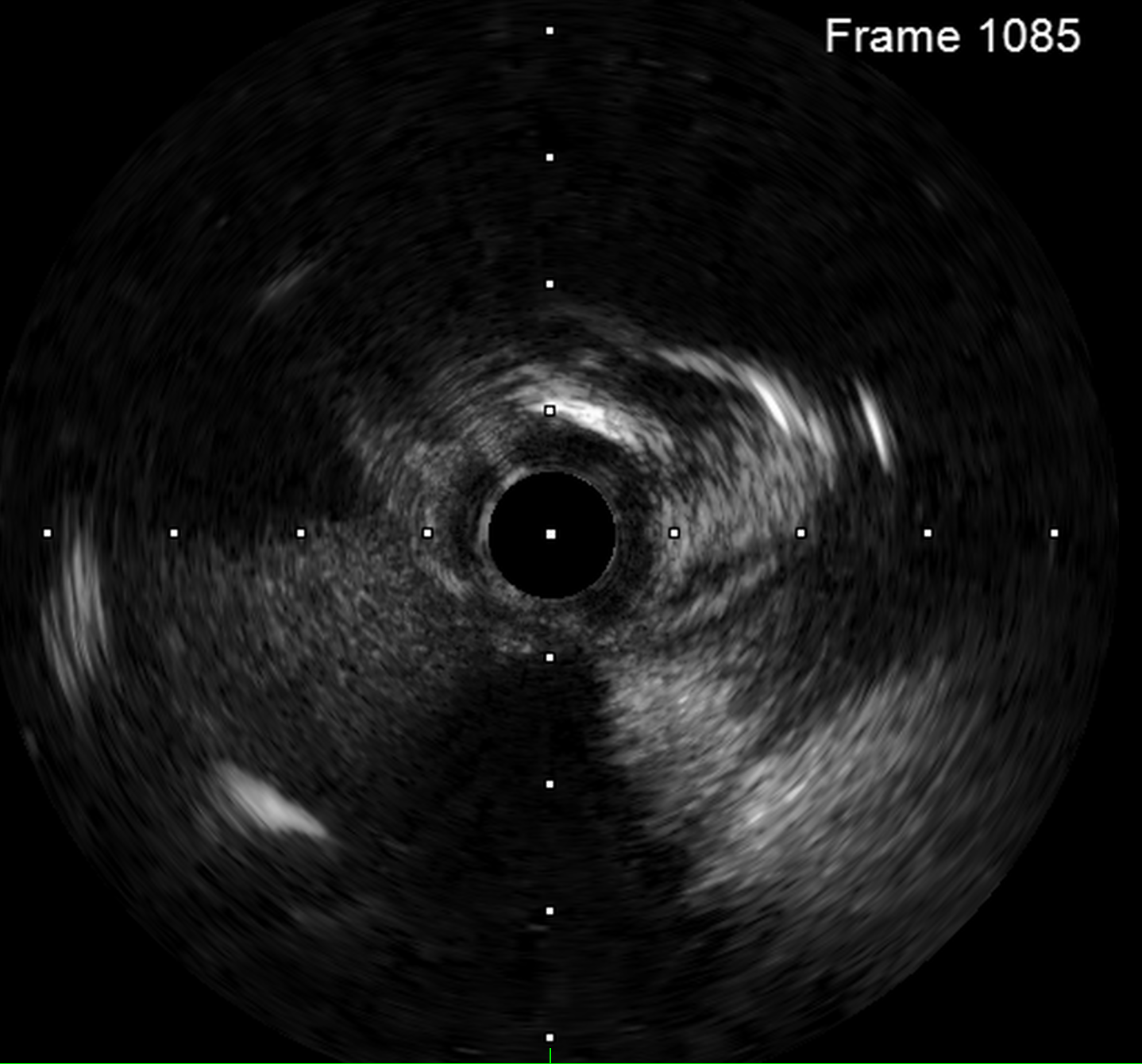
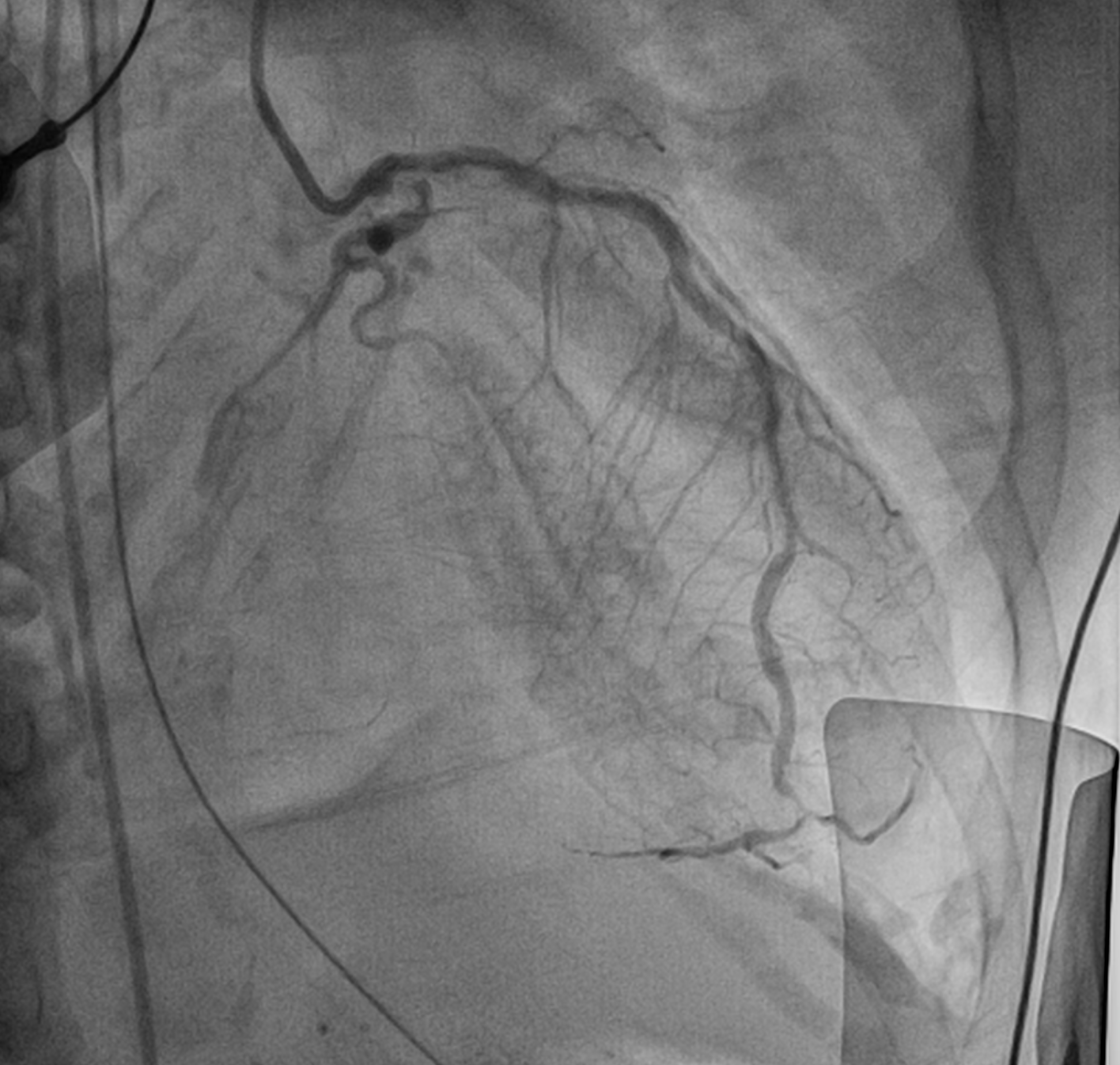
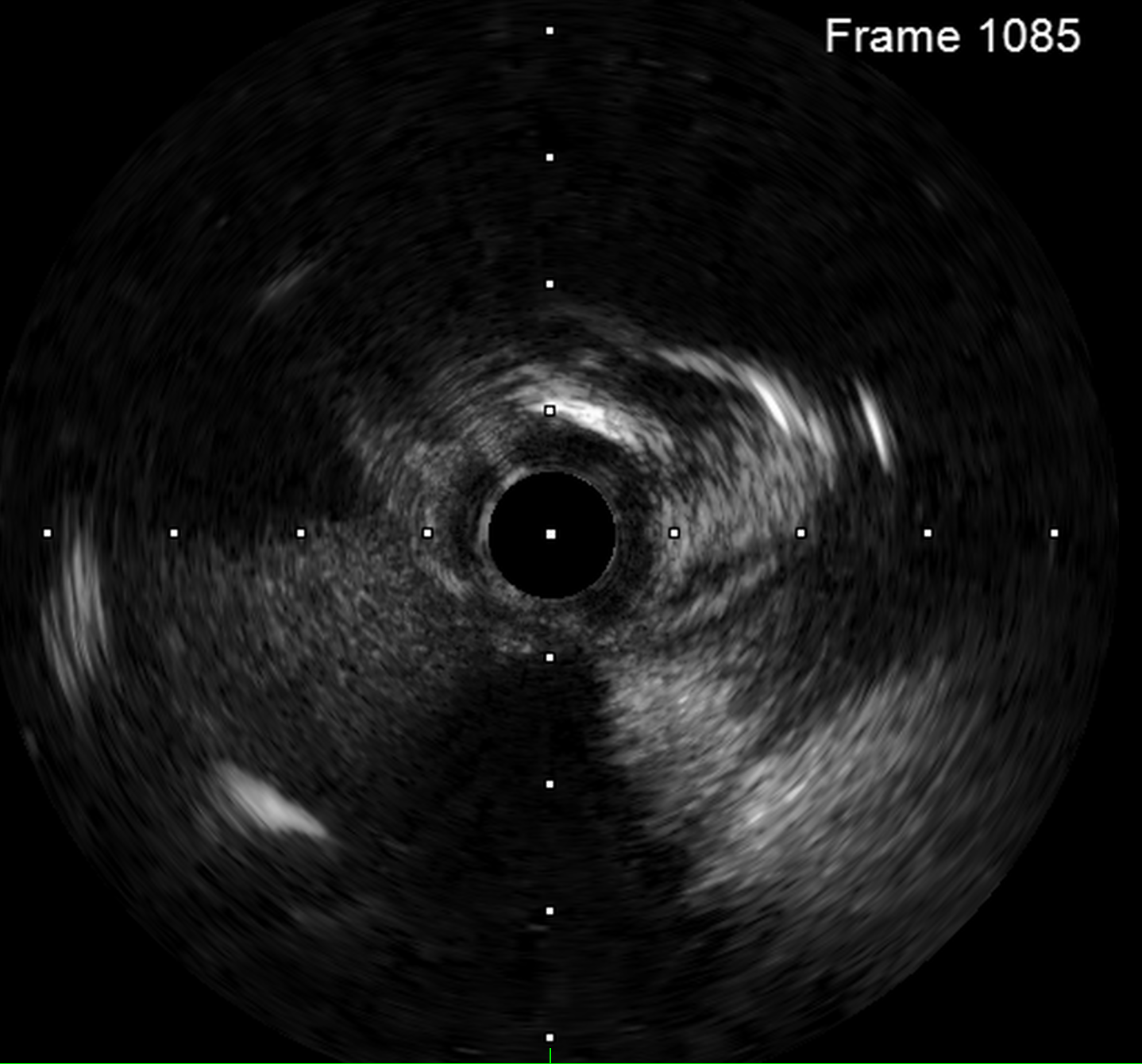
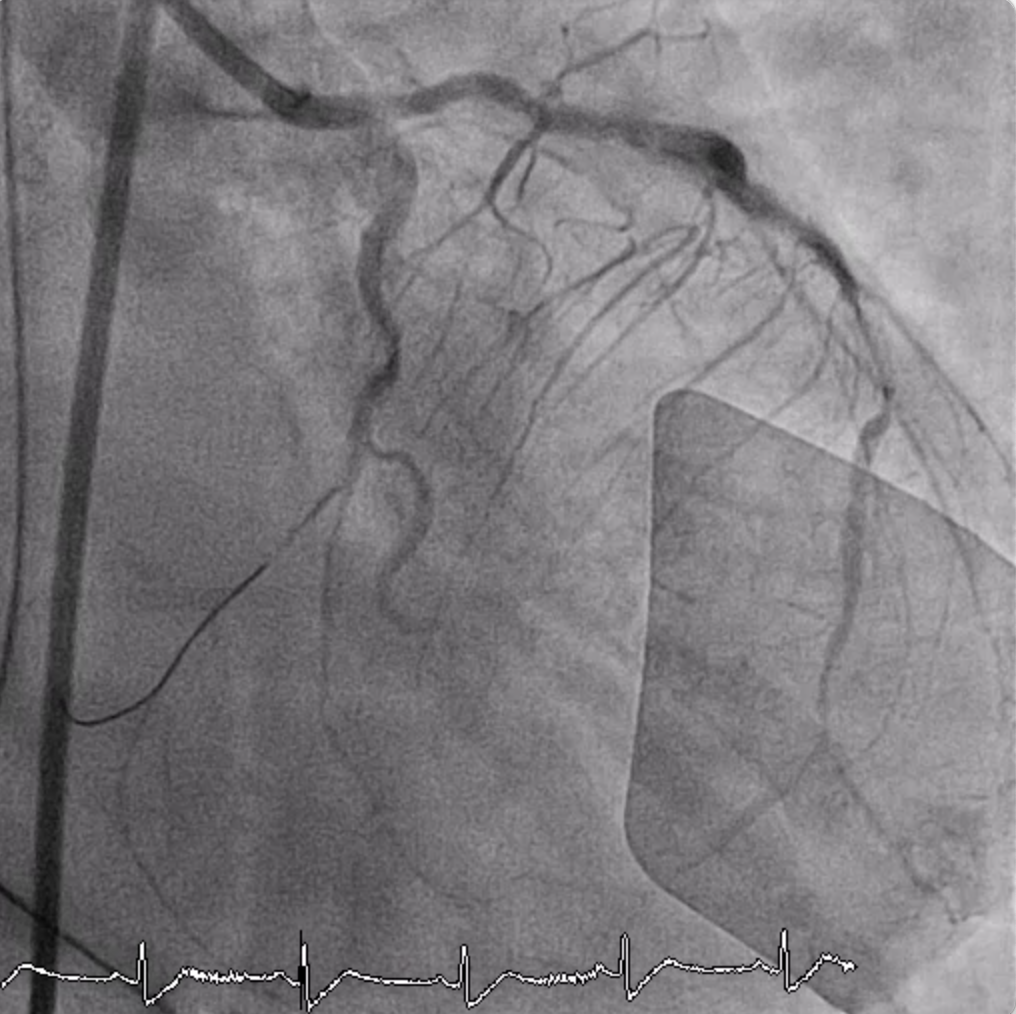
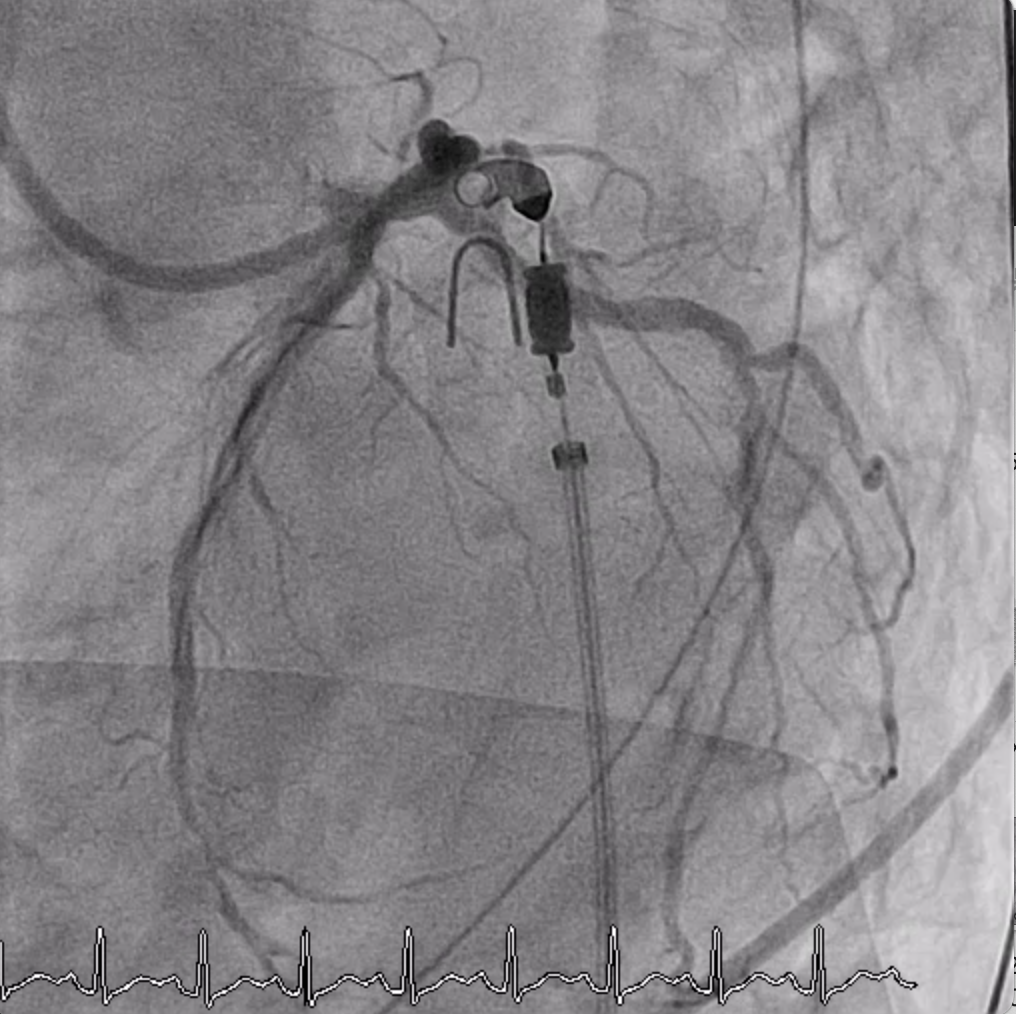
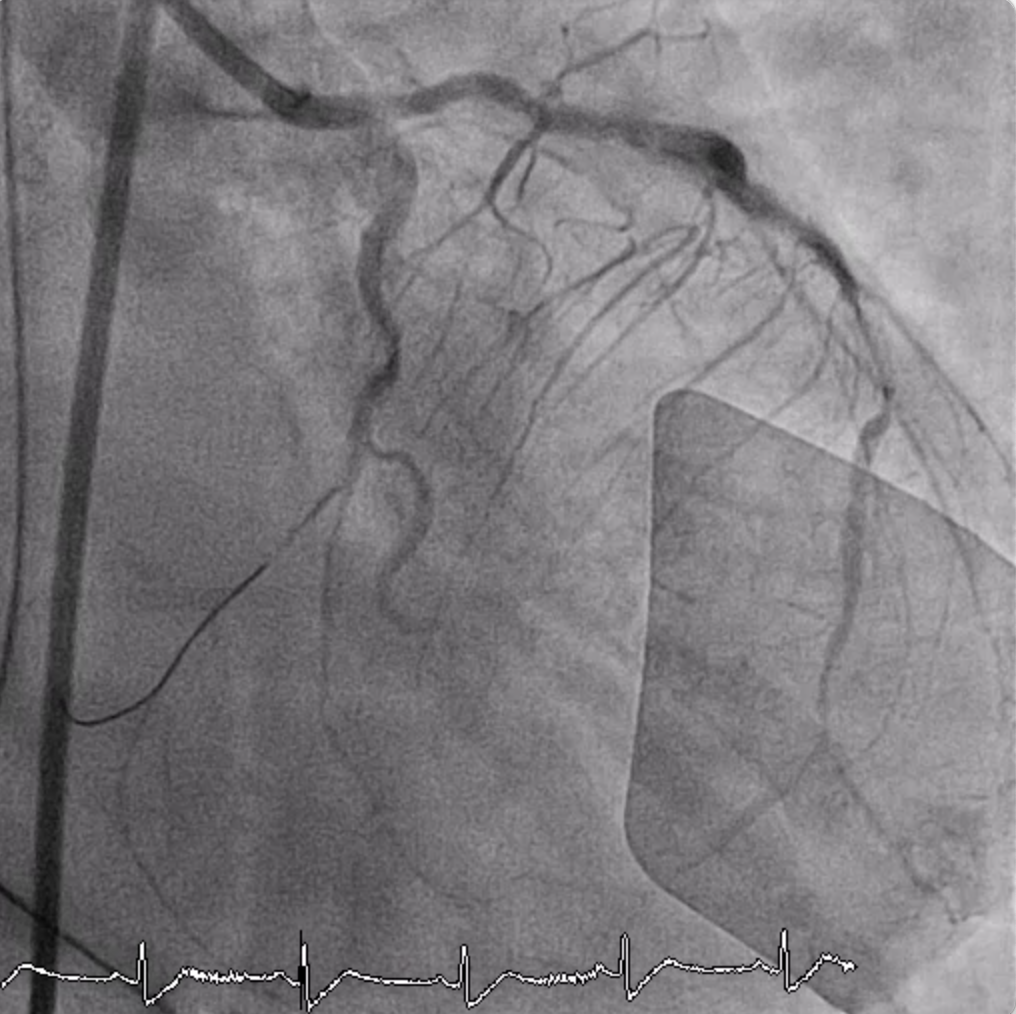
Coronary angiogram showed triple vessel disease, diffuse heavily calcified vessels, with distal LM 30% stenosis, proximal LAD 70% stenosis, ostial LCx 90% stenosis, and ostial RCA 70% stenosis. The LM bifurcation lesion was Medina (1,1,1). The ISR part at middle LAD and middle RCA both were below 50%. The distal LCx proper were small calliber. IVUS showed eccentric calcification with 180 degree at the narrowest ostial LCx.


Interventional Management
Procedural Step
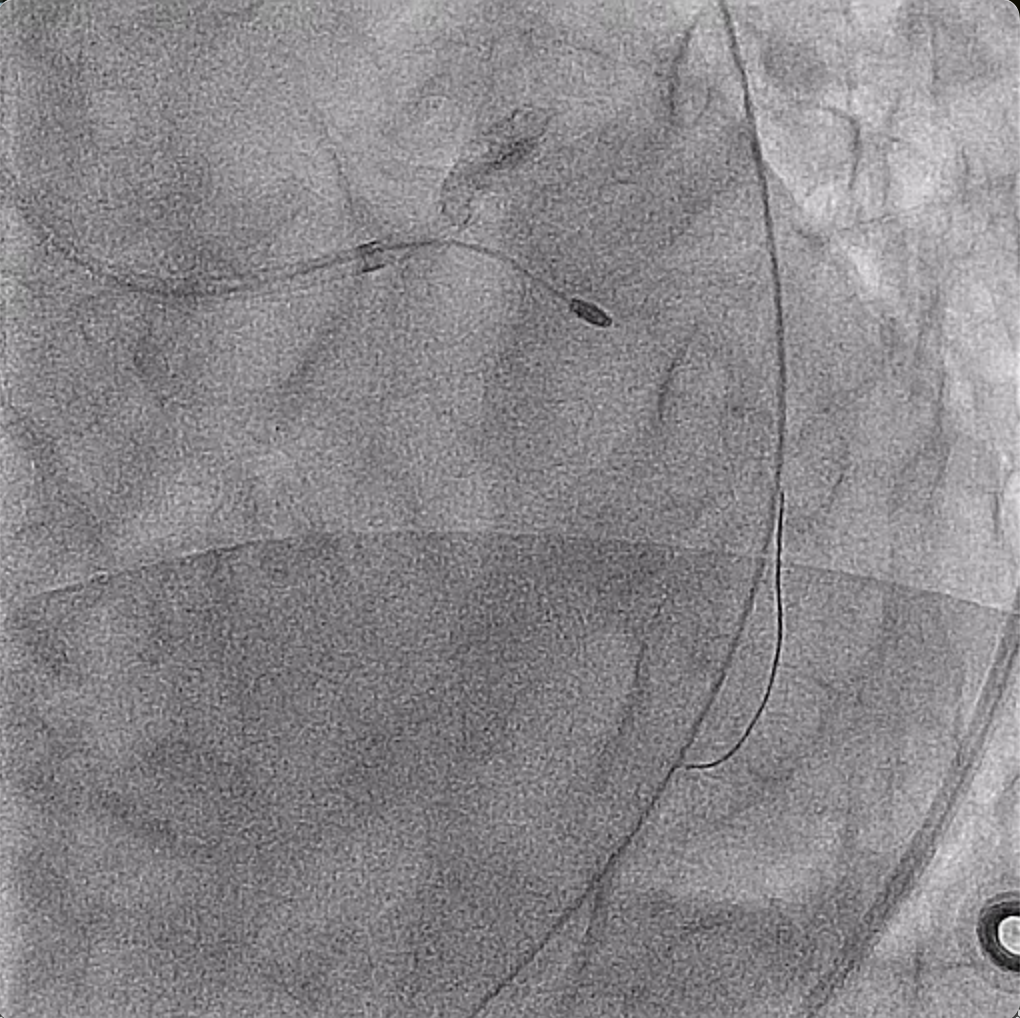
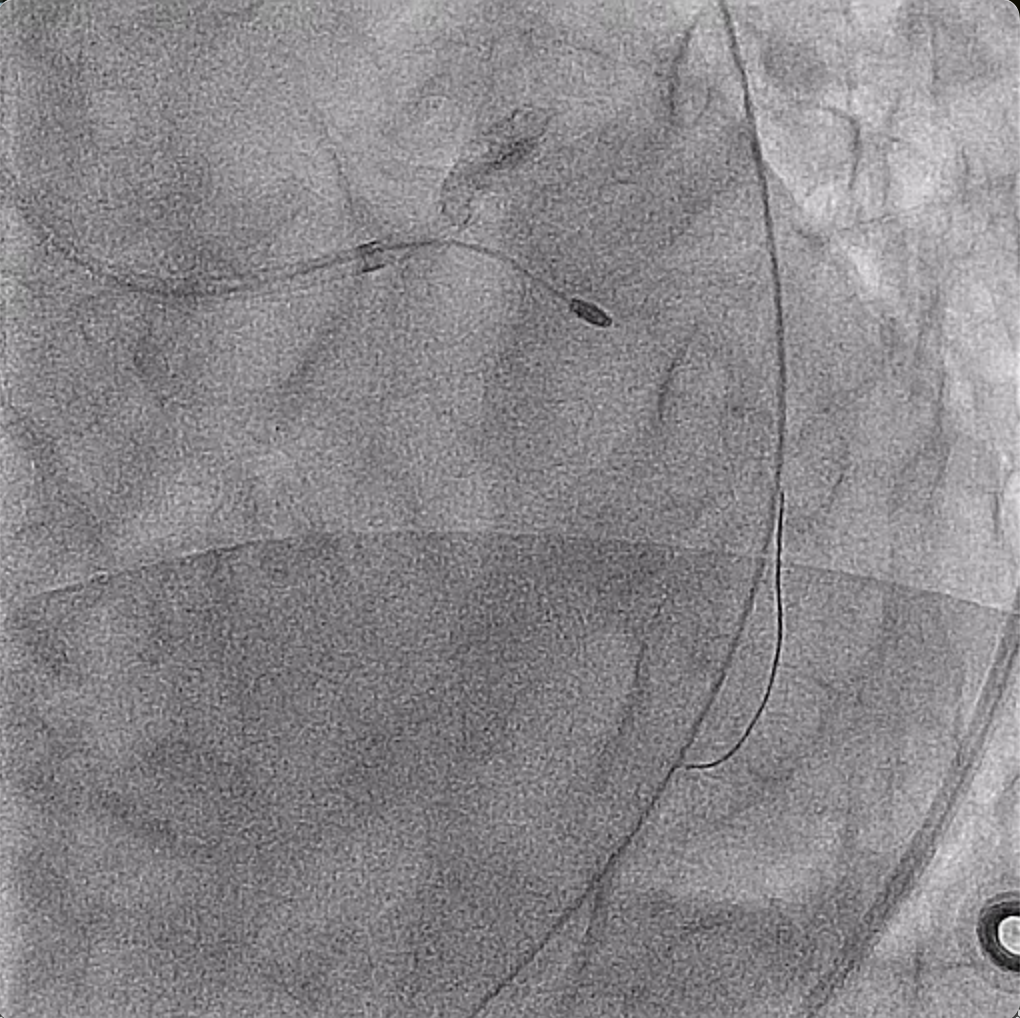
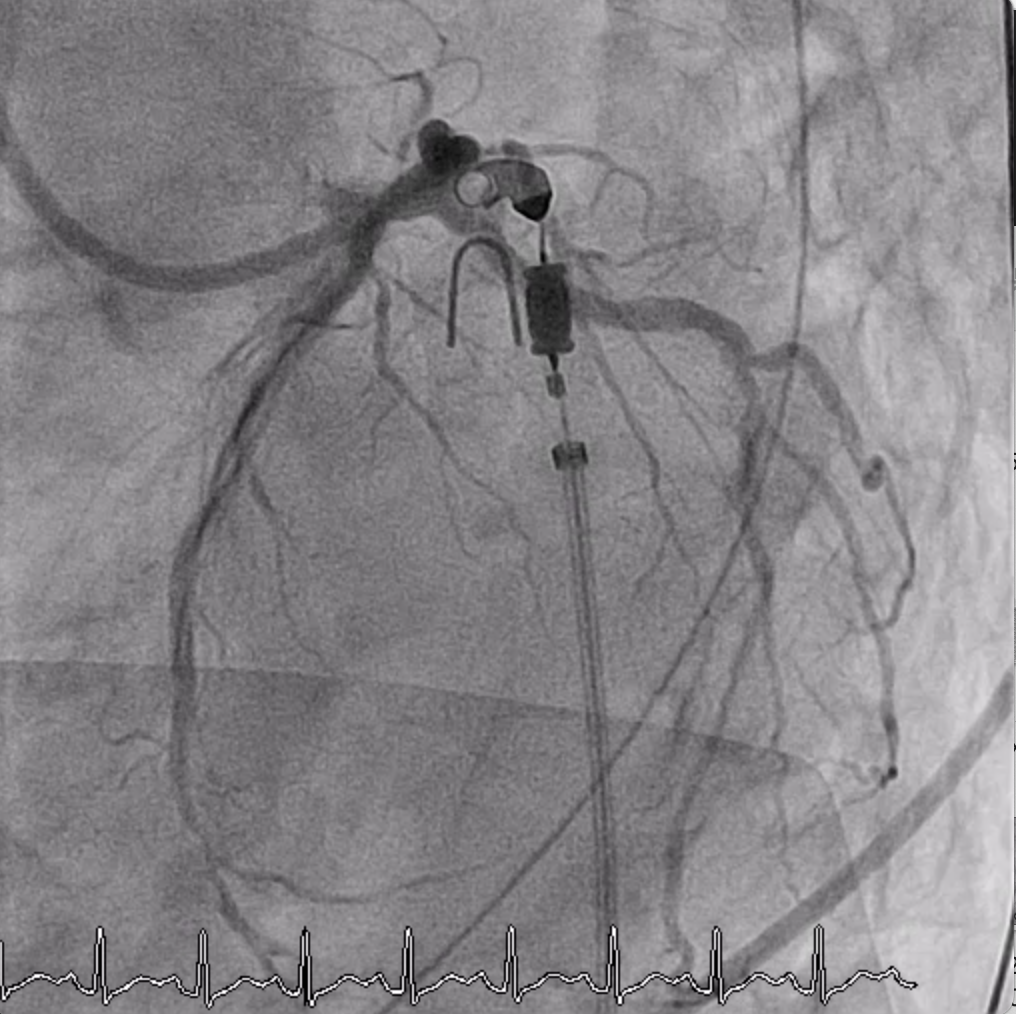
Placed a EBU 3.5 with side hole 7Fr guiding catheter via right femoral artery to left coronary artery. Placed a Fielder FC at dLCx and a BMW Elite at dLAD. Checked IVUS both along LCx and LAD sequentially for lumen size and plaque morphology evaluation. IVUS showed diffuse eccentric calcification along LCx and extended from ostial LCx to LM. The vessel size of pLCx/pLAD were 3.0/2.75mm. Performed rotational atherectomy by using Boston Rota Bur 1.75mm with a rota floppy wire along pLCx to LM up to 214,000rpm with 27 seconds. The angiogram showed TIMI 1 flow at pLCx and plaque shift to pLAD. Hypotension and bradycardia developed. Norepinephrine and epinephrine adminsitration started. Rechecked IVUS at LCx. IVUS showed intima distruption and asymmetric ovale oLCx. Performed balloon angioplasty with 3.0mm-sized semicompliance balloon along pLCx to LM, and deployed DES (Orsiro 3.0*22 + 3.0*18) along dLCx to LM by using Guideliner 5.5Fr. POT at LM was done with 3.5mm-sized balloon. IVUS showed good stent apposition but pseudoaneurysm. Another DES (Sierra 2.75*33) was placed at pLAD-LM by using culotte technique. Rewired Runthrough floppy to dLCx by using Crusade. Intermittent hypotension and bradycardia developed while intervented LAD, and IABP was placed via left femoral artery. Post-dilated LAD by using 2.75mm balloon and performed KBT by using 3.0/2.75mm balloons at LCx/LAD. Rechecked IVUS, and IVUS showed good stent apposition. The flow was TIMI 3. We stoped the procedure.
Case Summary
In a situation of ACS confronting heavily calcified bifurcation lesion was challenging. Patients undergoing hemodialysis were tend to had heavily calcified coronary vessels. Using rotablation in ACS with hemodynamic instability increased risk of no flow. Rotablation disrupted a calcified lesion at the side of wire bias. Using a stiffer wire (floppy Extrasupport) for wire bias may provide a better control of de-calcified direction to avoid vessel injury at contralteral side of vessel . A pseudoaneurysm after rotablation at ostial side branch was higly risky, which may lead to rupture or even death. With a successful bifurcation stenting strategy, pseudoaneurysm was secured in this situation.


