Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-026
It Takes Time to Break a Heart: Delayed Inferoseptal Pseudoaneurysm With Rupture Causing Ventricular Septal Defect Following Inferior Myocardial Infarction and Percutaneous Angioplasty
By Khai Chih Teh, Tjen Jhung Lee, Balachandran Kandasamy, Azmee Mohd Ghazi
Presenter
Khai Chih Teh
Authors
Khai Chih Teh1, Tjen Jhung Lee1, Balachandran Kandasamy2, Azmee Mohd Ghazi1
Affiliation
National Heart Institute, Malaysia1, Subang Jaya Medical Centre, Malaysia2,
View Study Report
TCTAP C-026
CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS)
It Takes Time to Break a Heart: Delayed Inferoseptal Pseudoaneurysm With Rupture Causing Ventricular Septal Defect Following Inferior Myocardial Infarction and Percutaneous Angioplasty
Khai Chih Teh1, Tjen Jhung Lee1, Balachandran Kandasamy2, Azmee Mohd Ghazi1
National Heart Institute, Malaysia1, Subang Jaya Medical Centre, Malaysia2,
Clinical Information
Patient initials or Identifier Number
461606
Relevant Clinical History and Physical Exam
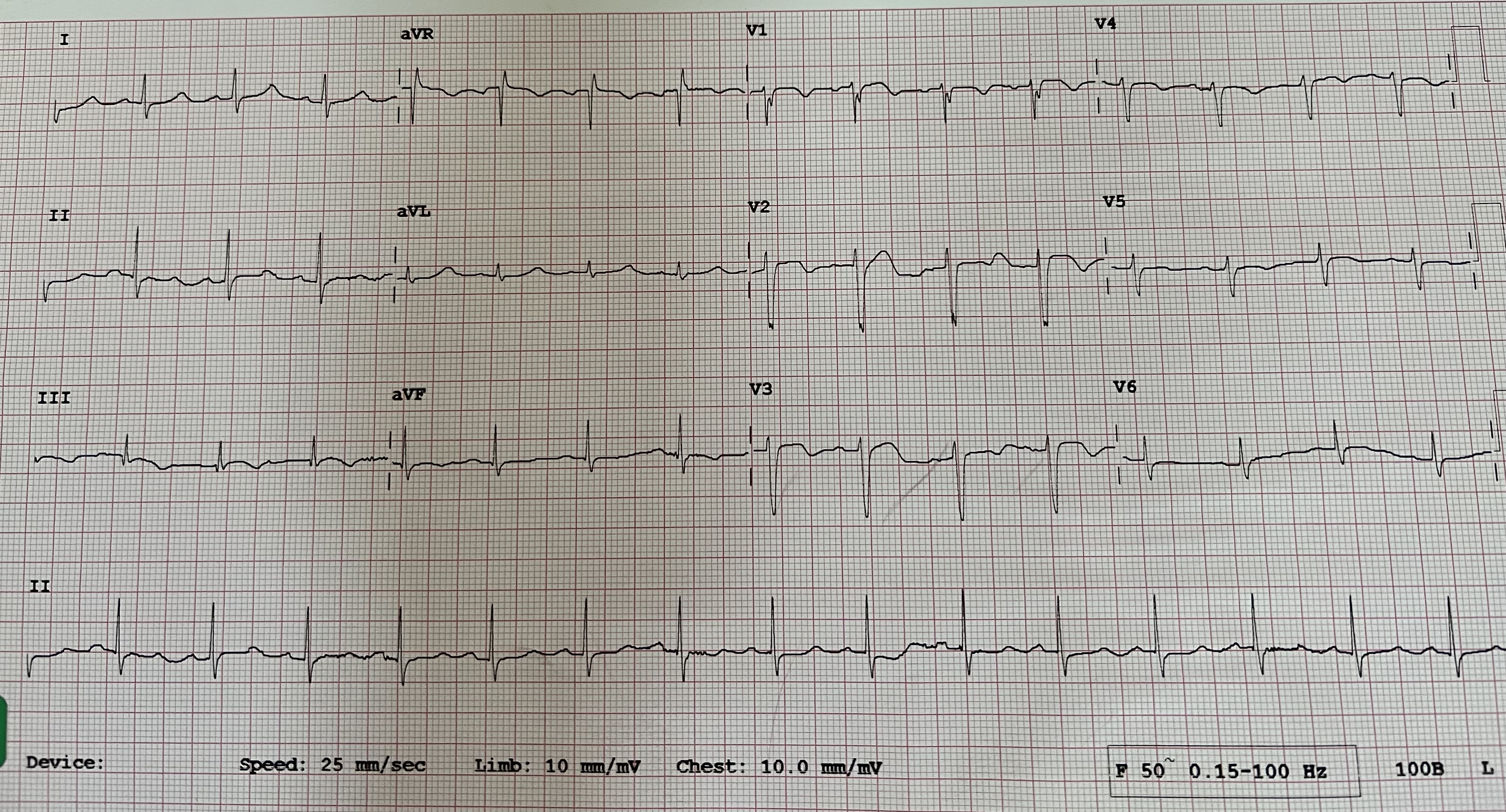
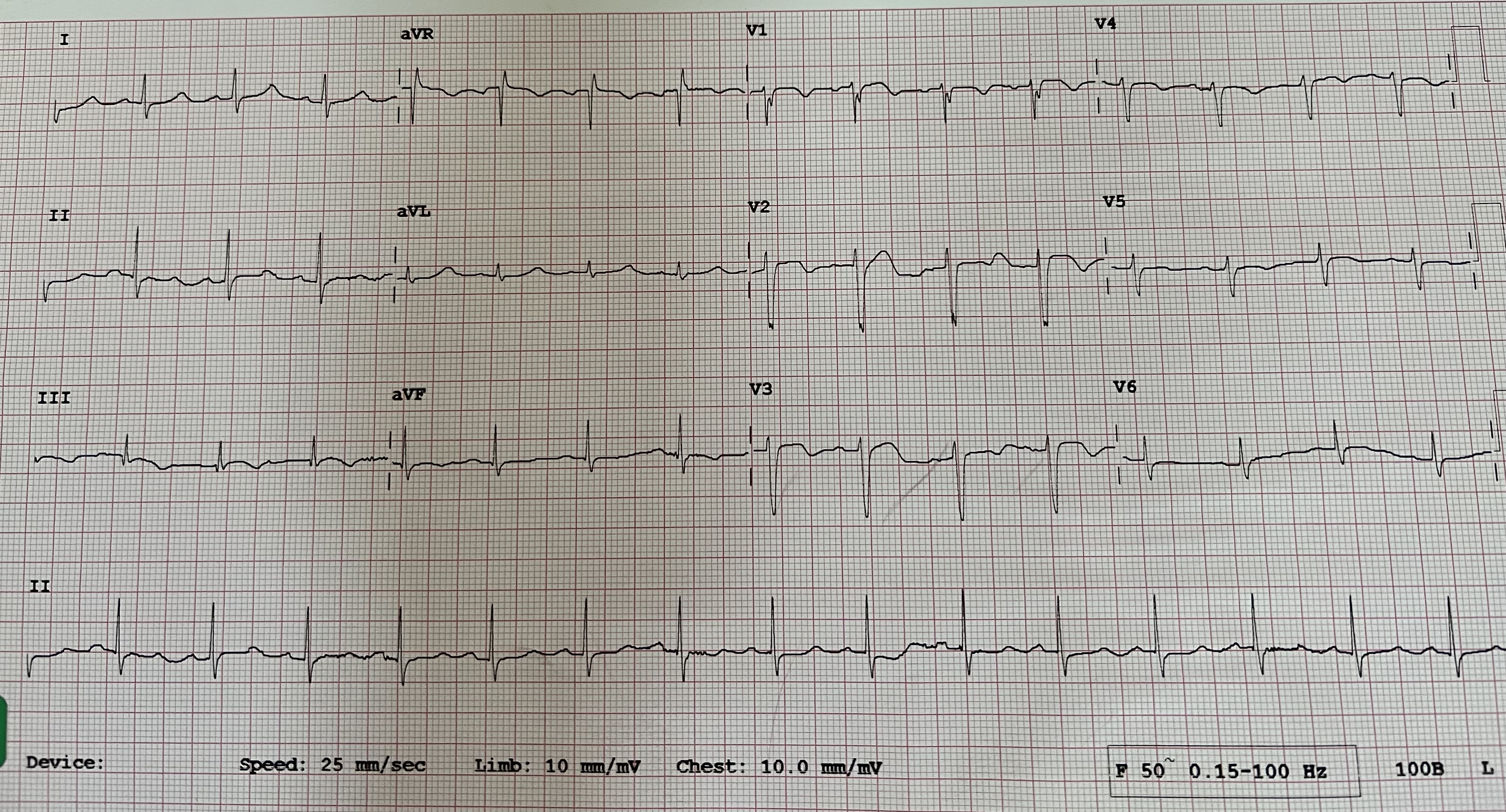
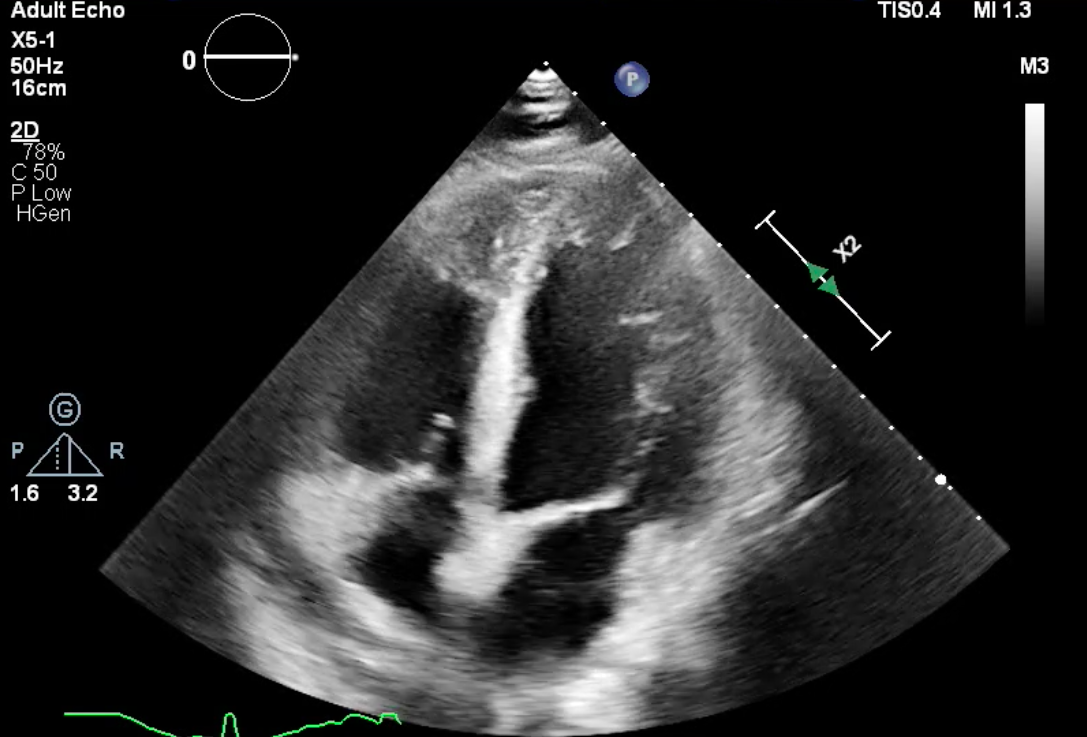
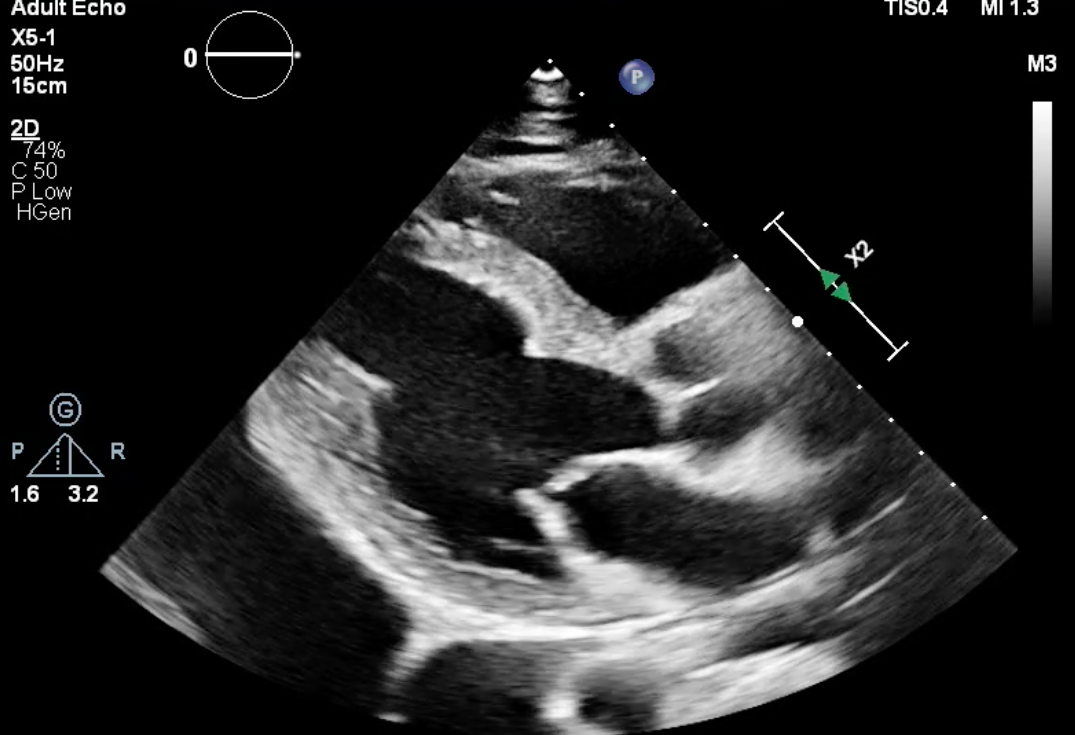
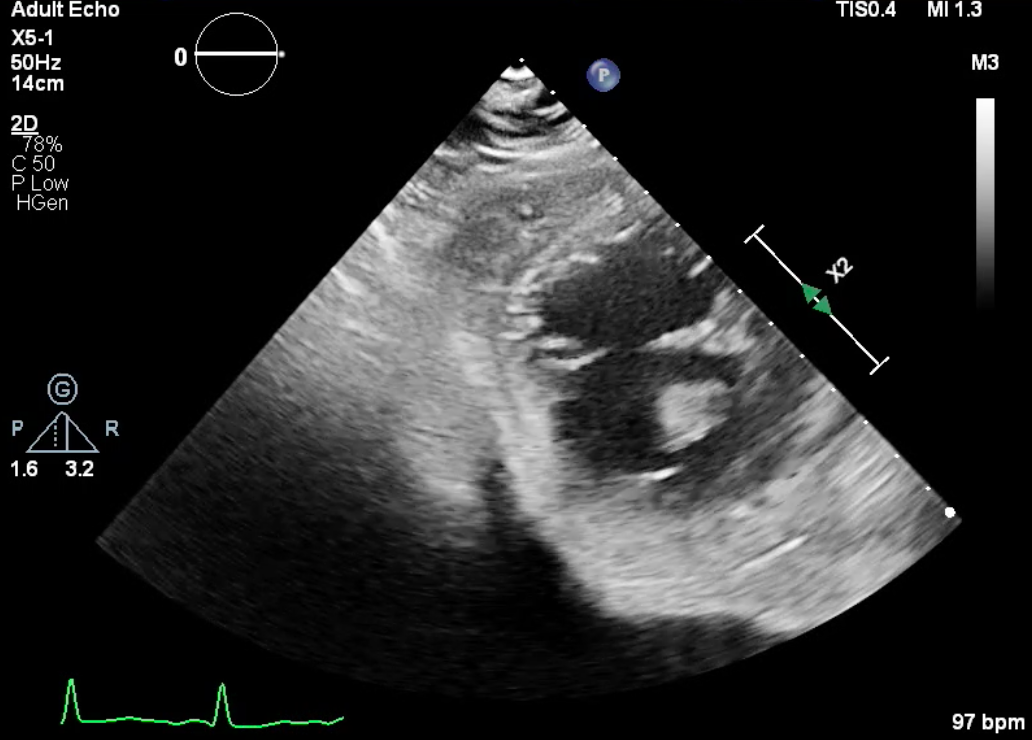
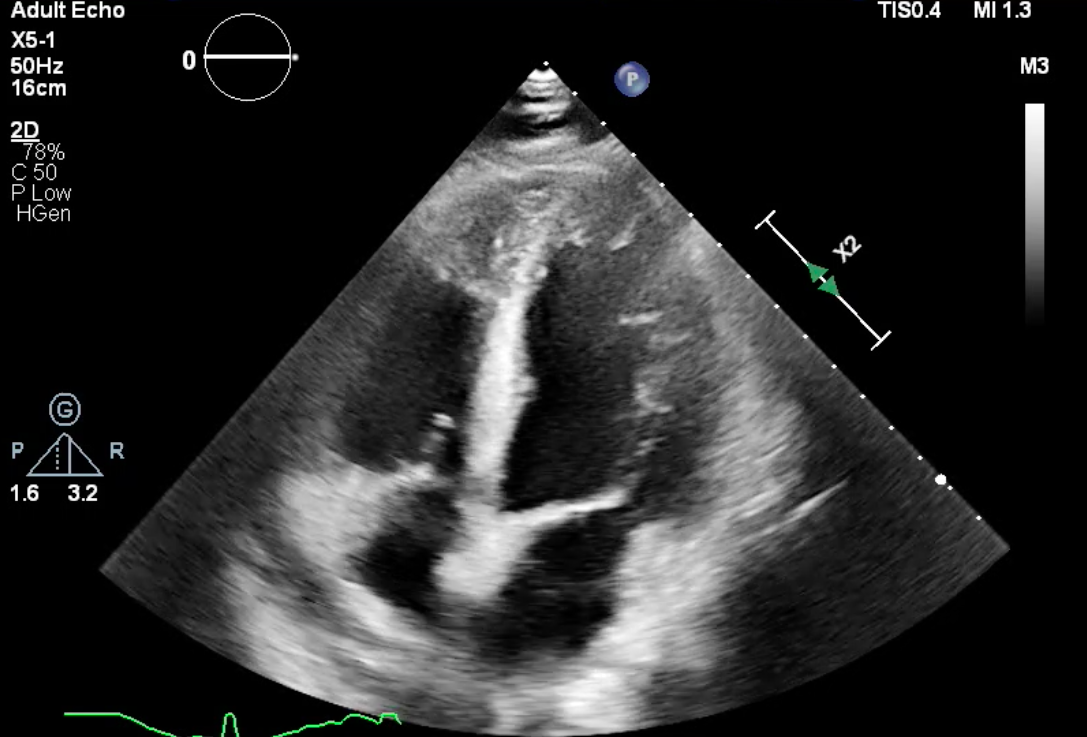
70 year old male diabetic, hypertensive and CKD 3a present to district hospital in June 2021 with chest pain and hypotension. ECG shows inferior ST elevation and he was thrombolysed for inferior MI. Physical examination showed no murmur. ECHO LVEF 50%, mid to apical inferior hypokinesia, no septal defect or valve abnormality. PCI to RCA and circumflex were uneventful. He presented in July 2021 with heart failure and ECHO showed ruptured septal pseudoaneurysm with ventricular septal defect.
Relevant Test Results Prior to Catheterization
ECG Q III, T inversion V2 V3 V4
LVEF 50% mid to apical inferior hypokinesiano septal or valvular defects
Creatinine 193 umol/ltrop T 106 pg/ml
LVEF 50% mid to apical inferior hypokinesiano septal or valvular defects
Creatinine 193 umol/ltrop T 106 pg/ml
Relevant Catheterization Findings
Left main: normal
Left anterior descending: diffuse moderate disease from ostium to mid LAD; bridging mid LAD
Left circumflex: severe stenosis in distal LCx
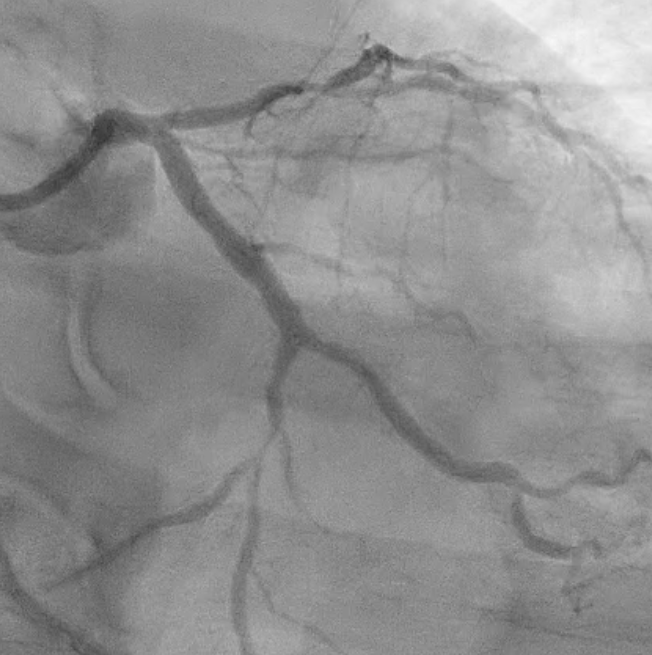
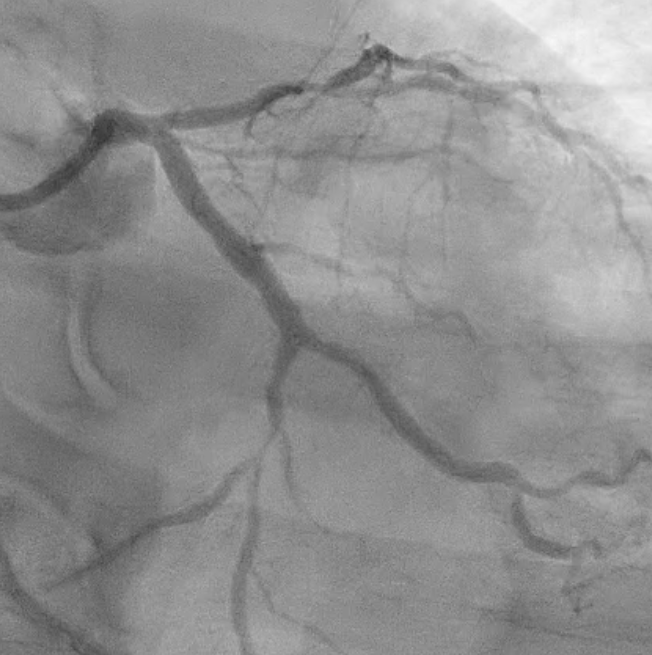
Right coronary: diffuse mild disease proximal to mid RCAsevere stenosis with ulcerated plaque in distal RCA into RPL branch
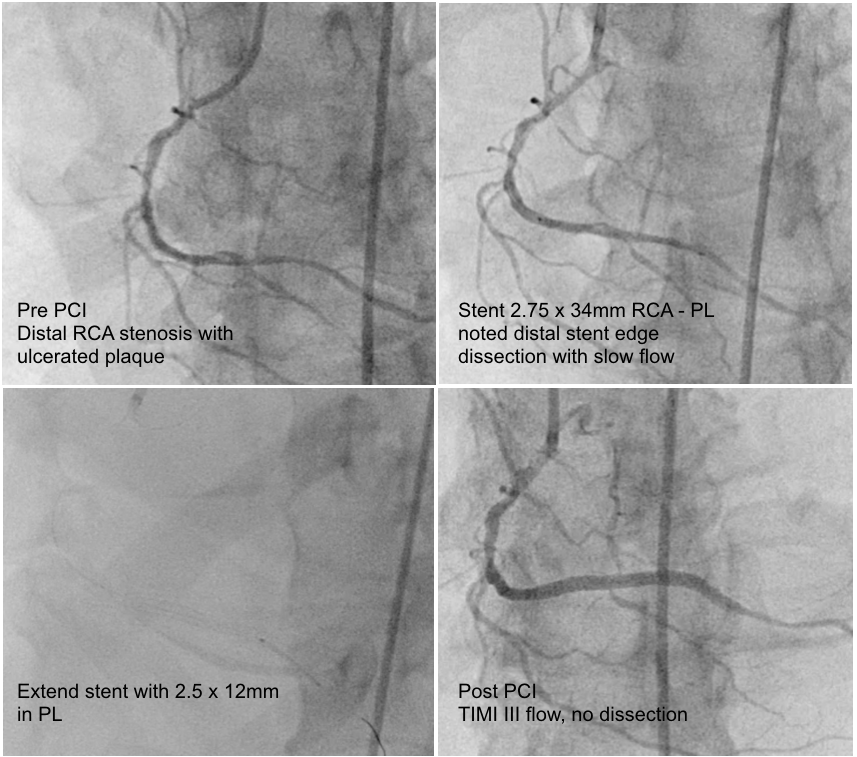
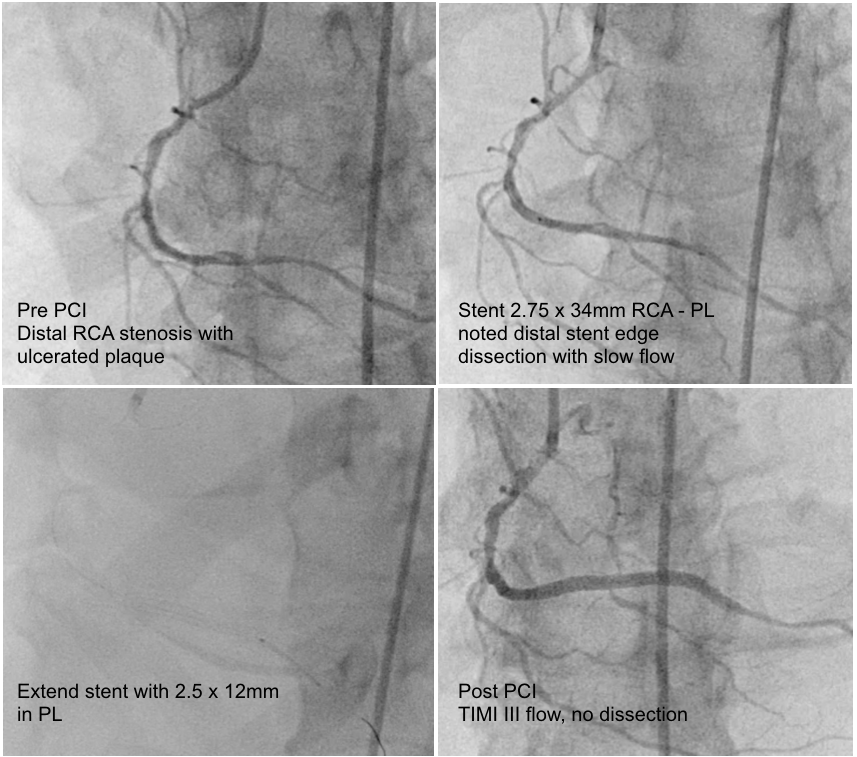
PCI to RCA: RESOLUTE ONYX 2.75 x 34mm into PL, then extended stent ONYX 2.5 x 12mm in PL for distal stent edge dissection
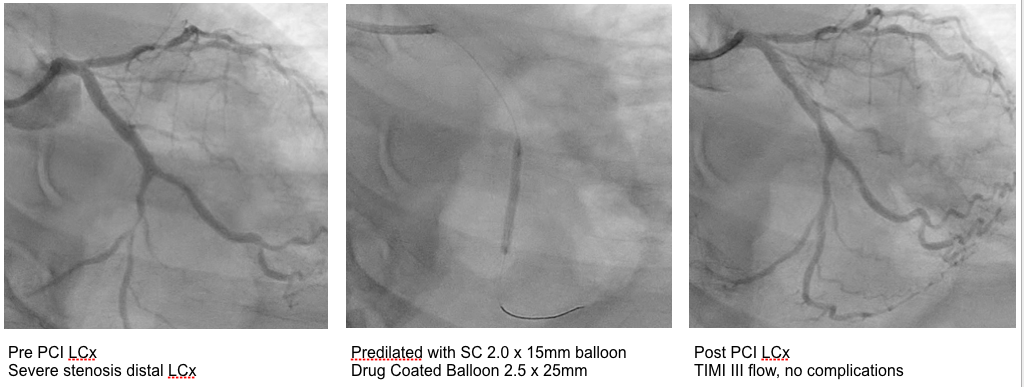
PCI to LCx: Drug Eluting Balloon ESSENTIAL 2.5 x 25mm

Left anterior descending: diffuse moderate disease from ostium to mid LAD; bridging mid LAD
Left circumflex: severe stenosis in distal LCx
Right coronary: diffuse mild disease proximal to mid RCAsevere stenosis with ulcerated plaque in distal RCA into RPL branch
PCI to RCA: RESOLUTE ONYX 2.75 x 34mm into PL, then extended stent ONYX 2.5 x 12mm in PL for distal stent edge dissection
PCI to LCx: Drug Eluting Balloon ESSENTIAL 2.5 x 25mm

Interventional Management
Procedural Step
PCI to RCA was performed with JR 3.5 guide and workhorse wire to PL branch. Distal RCA to PL was stented with RESOLUTE ONYX 2.75 x 34mm but noted distal stent edge dissection with slow flow, decided to extend stent with ONYX 2.5 x 12mm. Final results TIMI III flow.
Staged PCI to Circumflex was performed a week later with EBU 3.5 guide, drug coated balloon ESSENTIAL 2.5 x 25mm to mid distal circumflex with final results TIMI III flow and no complications. Patient was discharged well.
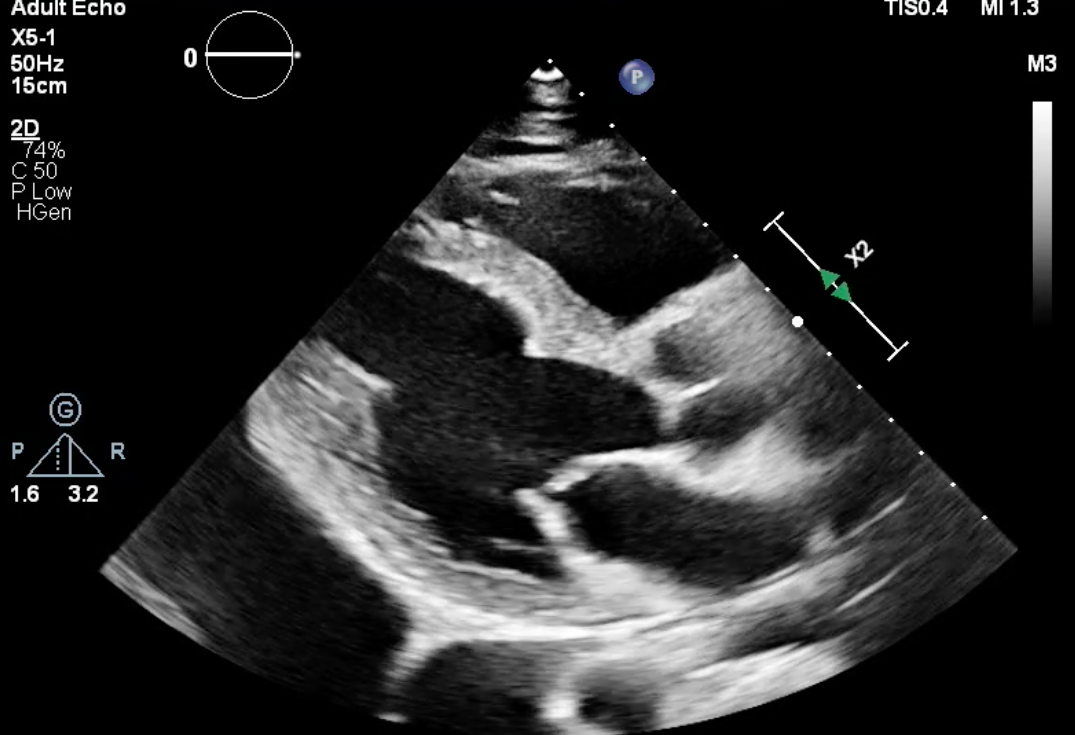
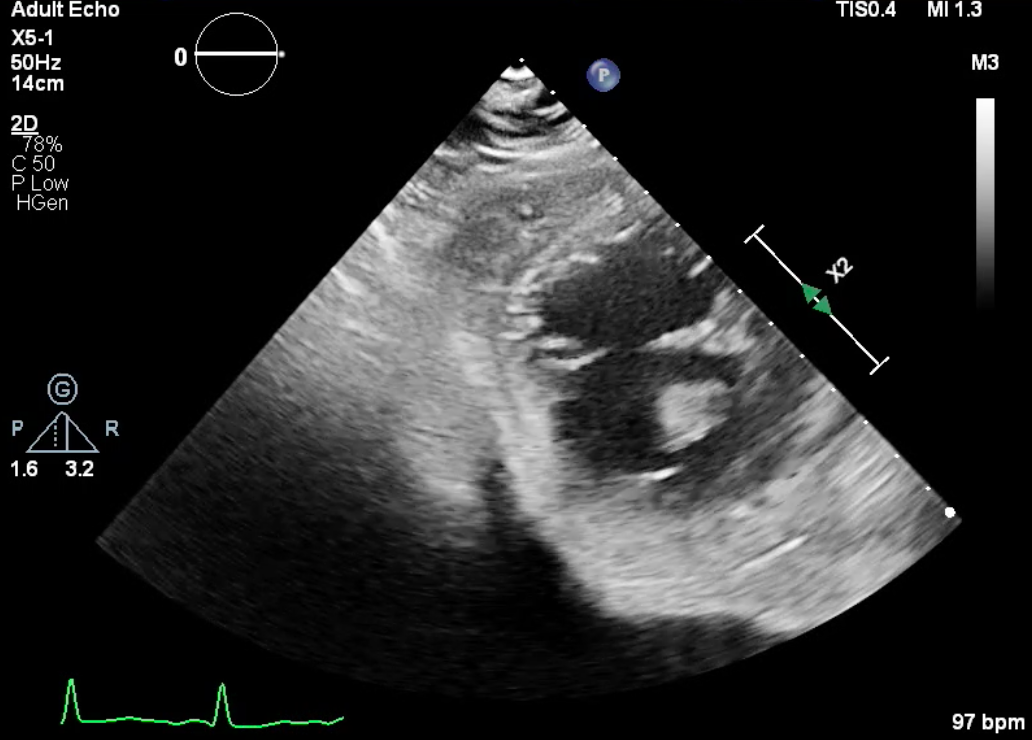
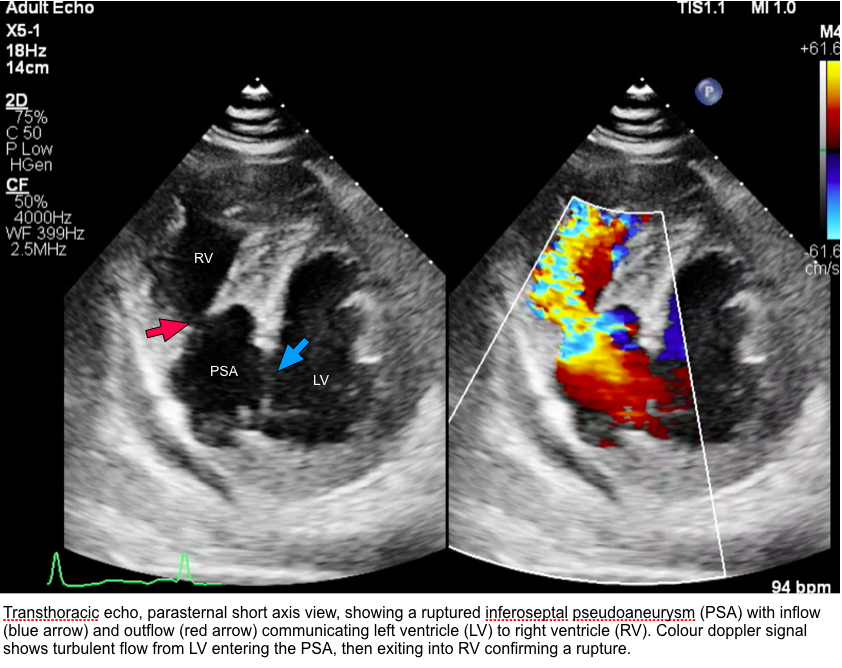
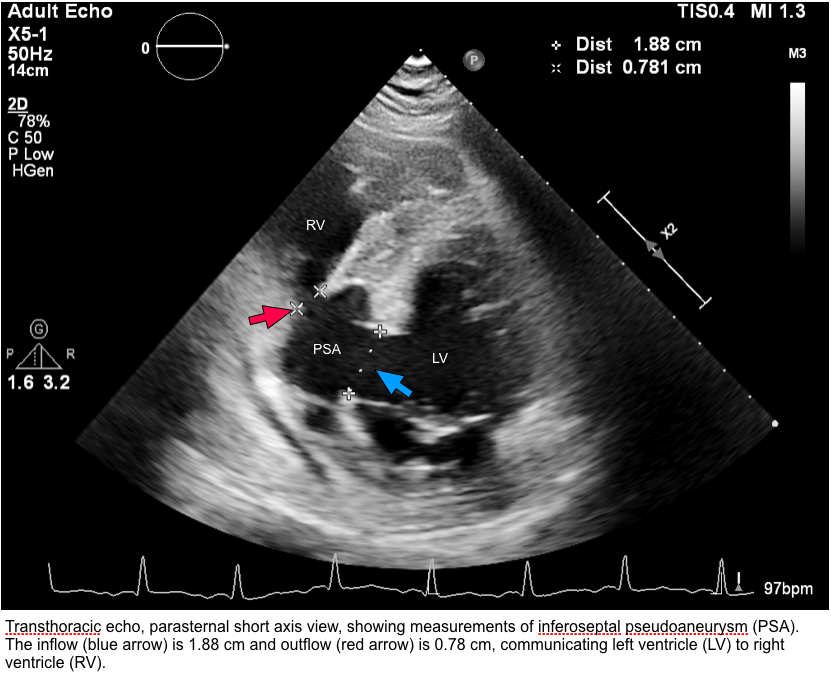
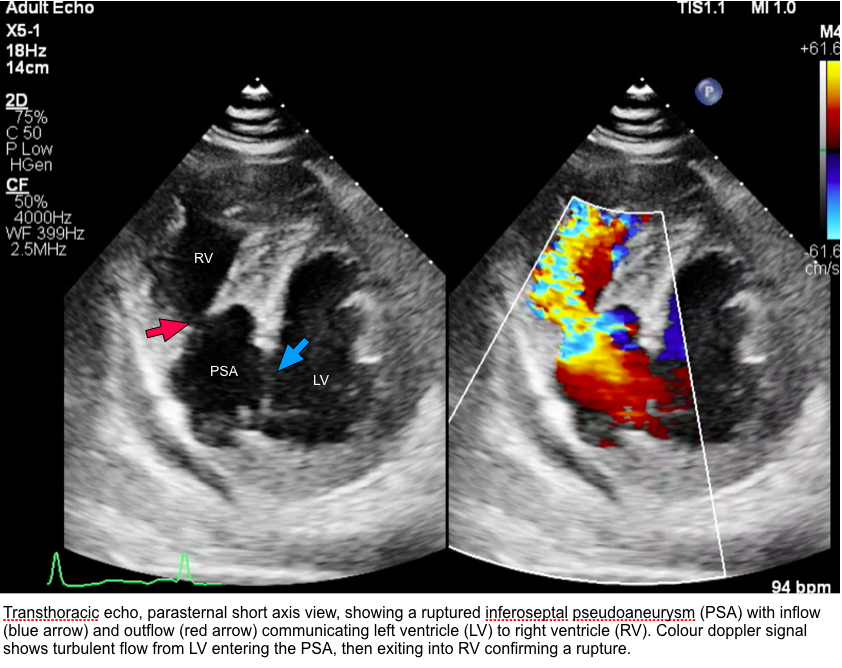
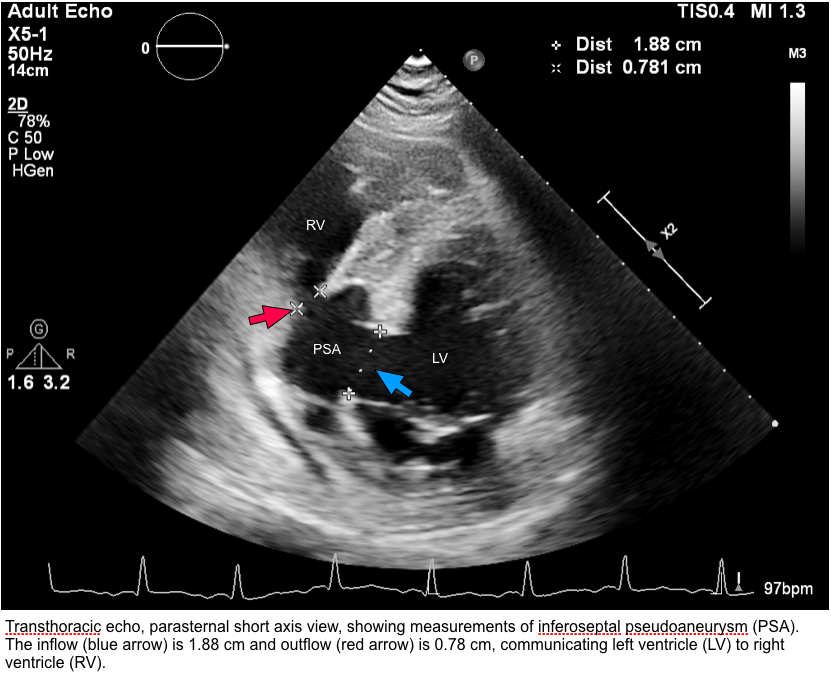
He presented a month later with heart failure symptoms. Auscultation revealed bibasal crepitations and a harsh pansystolic murmur over his precordium. ECHO showed poor LV systolic function 40 - 45% with thinned out LV inferoseptal and inferior wall. There was a large ruptured pseudoaneurysm over basal inferoseptal wall, with left to right shunt through the ventricular septal rupture (VSR) into the right ventricle. The pseudoaneurysm inlet measured 1.8cm with a 0.78cm outlet draining into the right ventricle. Peak gradient across the septal defect was 79 mmHg. The right ventricle was dilated with TAPSE 1.3cm. Valves were uneventful.
He was referred to cardiothoracic surgeon for surgical correction of VSR however he was deemed high risk for surgery, and the patient refused surgical intervention. He was optimized on antifailure medication and was discharged stable with plans for percutaneous closure of VSR later.
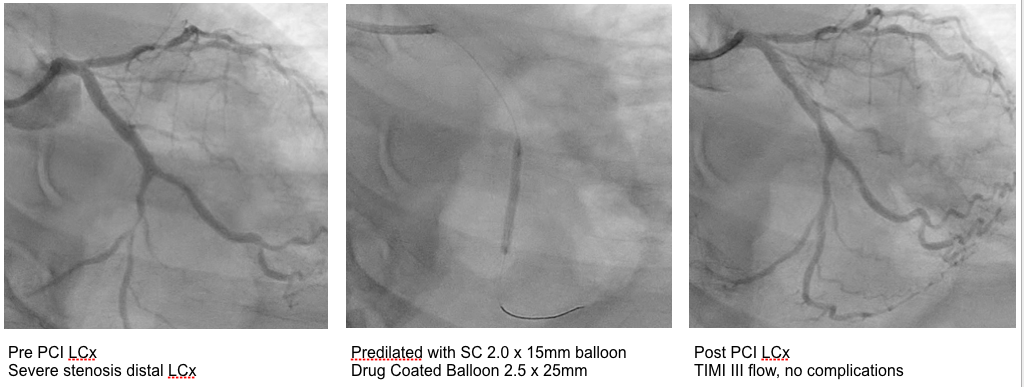
Staged PCI to Circumflex was performed a week later with EBU 3.5 guide, drug coated balloon ESSENTIAL 2.5 x 25mm to mid distal circumflex with final results TIMI III flow and no complications. Patient was discharged well.
He presented a month later with heart failure symptoms. Auscultation revealed bibasal crepitations and a harsh pansystolic murmur over his precordium. ECHO showed poor LV systolic function 40 - 45% with thinned out LV inferoseptal and inferior wall. There was a large ruptured pseudoaneurysm over basal inferoseptal wall, with left to right shunt through the ventricular septal rupture (VSR) into the right ventricle. The pseudoaneurysm inlet measured 1.8cm with a 0.78cm outlet draining into the right ventricle. Peak gradient across the septal defect was 79 mmHg. The right ventricle was dilated with TAPSE 1.3cm. Valves were uneventful.
He was referred to cardiothoracic surgeon for surgical correction of VSR however he was deemed high risk for surgery, and the patient refused surgical intervention. He was optimized on antifailure medication and was discharged stable with plans for percutaneous closure of VSR later.
Case Summary
This case documents a rare delayed ventricular septal pseudoaneurysm 1 month following an inferior MI and successful PCI to coronary arteries, with subsequent rupture into the right ventricle forming a left to right shunting ventricular septal defect (VSR). Ventricular septal pseudoaneurysms occur following transmural infarction of the septum and formation of a thin walled cavity, with high risk of rupture compared to true aneurysms. Early detection is by ECHO or MRI. Urgent surgical correction is indicated however risks are high due to friability of infarcted tissue complicating closure of the defect. Conservative management is common but mortality due to biventricular failure remains high.


