Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-112
A Challenging Case Report: A Novel Approach in Distal Vessel Perforation
By Suchat Sricholwattana, Thitima Limjaroen, Vorarit Lertsuwunseri, Wasan Udayachalerm
Presenter
Suchat Sricholwattana
Authors
Suchat Sricholwattana1, Thitima Limjaroen2, Vorarit Lertsuwunseri2, Wasan Udayachalerm2
Affiliation
HRH Maha Chakri Sirindhorn Medical Center, Thailand1, King Chulalongkorn Memorial Hospital, Thailand2,
View Study Report
TCTAP C-112
CORONARY - Complications (Coronary)
A Challenging Case Report: A Novel Approach in Distal Vessel Perforation
Suchat Sricholwattana1, Thitima Limjaroen2, Vorarit Lertsuwunseri2, Wasan Udayachalerm2
HRH Maha Chakri Sirindhorn Medical Center, Thailand1, King Chulalongkorn Memorial Hospital, Thailand2,
Clinical Information
Patient initials or Identifier Number
Mr.CK
Relevant Clinical History and Physical Exam
A 76-year-old man with known medical history of type 2 diabetes, hypertension, hyperlipidemia, old stroke, and recent NSTEMI with left main and triple vessel disease presented with chest discomfort without clinical signs of congestive heart failure. His vital signs were stable. Cardiac and respiratory examination were unremarkable.
Relevant Test Results Prior to Catheterization
The electrocardiogram revealed normal sinus rhythm with ST-segment elevation in limb lead aVR and diffuse ST-segment depression in precordial leads V1-V6. His echocardiogram showed preserved left ventricular systolic function with ejection fraction of 60% and infero-posterior wall hypokinesia. There was no significant valvular abnormalities or pericardial effusion.
Relevant Catheterization Findings
His coronary angiogram revealed severe calcification along coronary arteries with high SYNTAX score of 36; 50% stenosis at left main coronary artery, 90% stenosis at proximal LAD, 90% stenosis at proximal LCx and OM2, 90% stenosis at proximal RCA, and chronic total occlusion (CTO) at the mid RCA (J-CTO score of 2). Collateral vessels originating from LCx to RCA territories were observed.
Interventional Management
Procedural Step
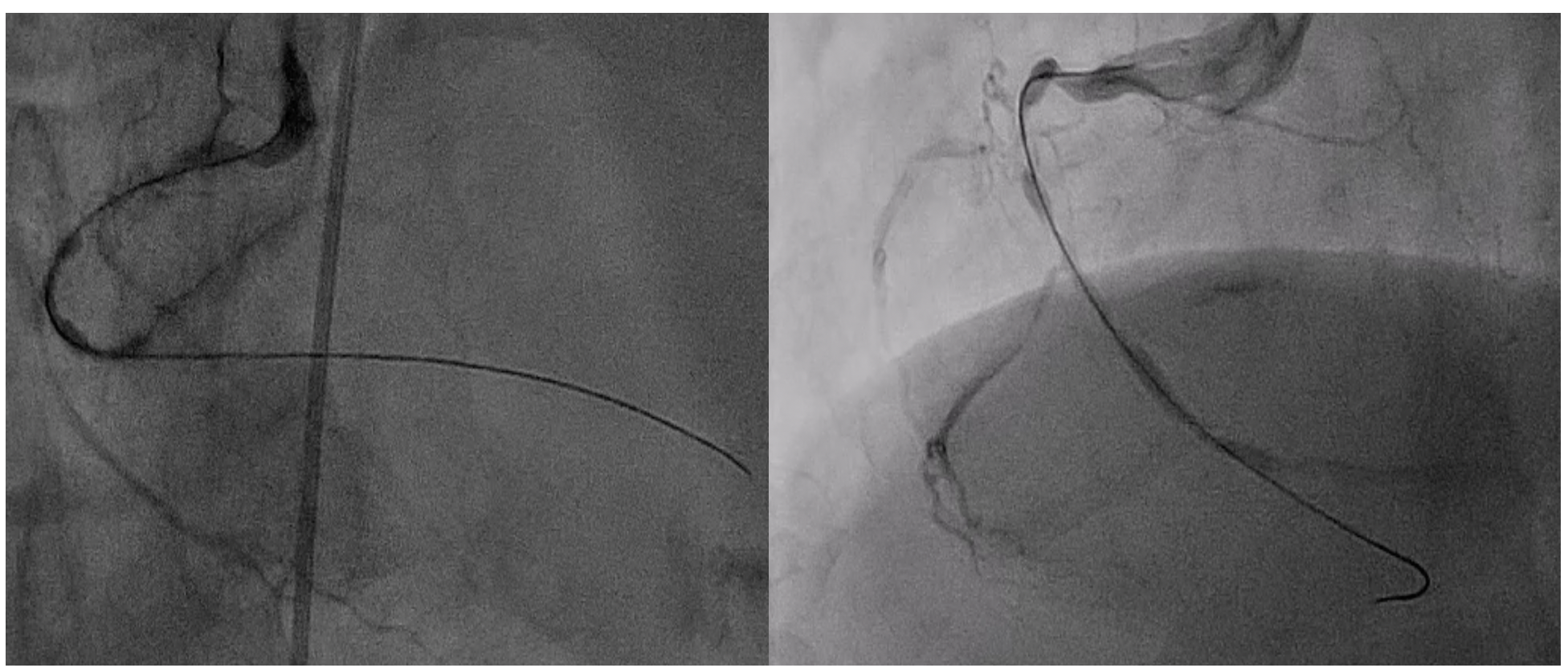
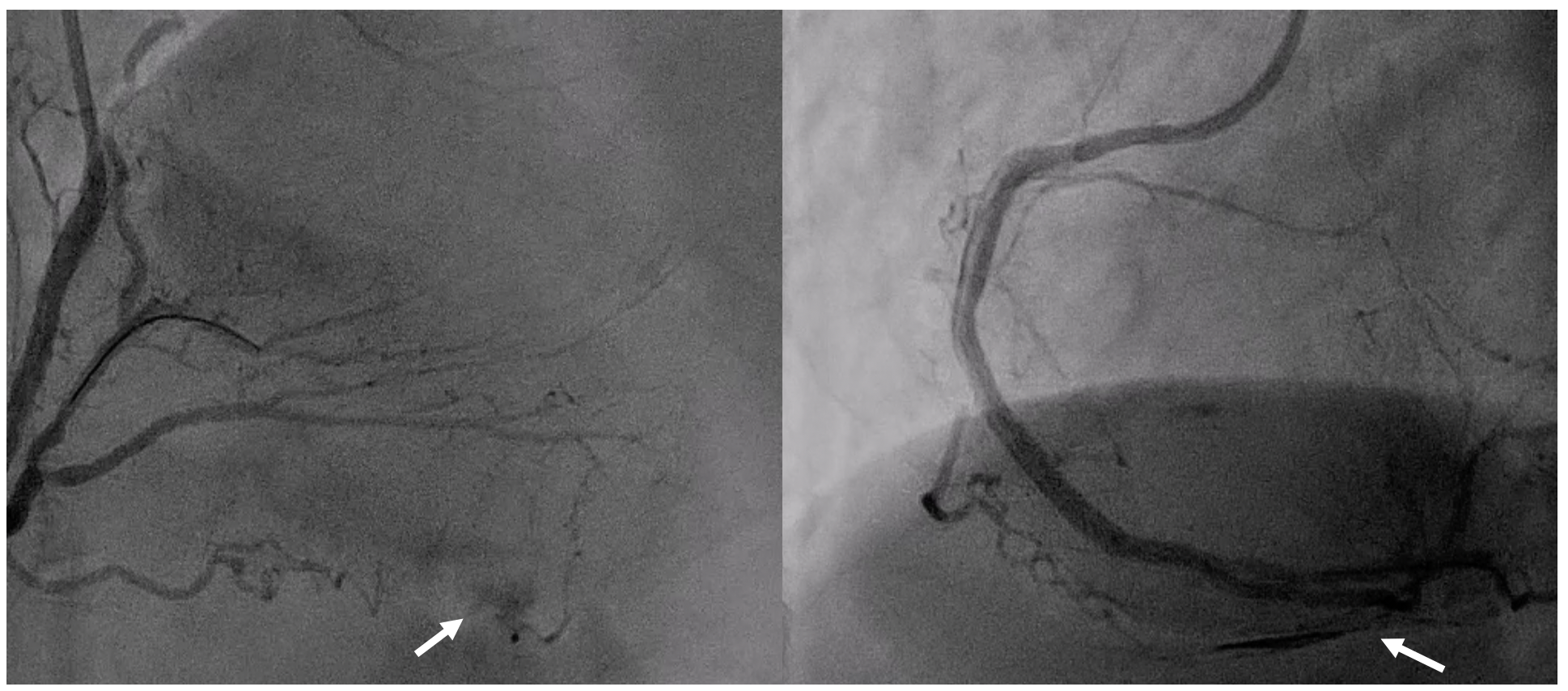
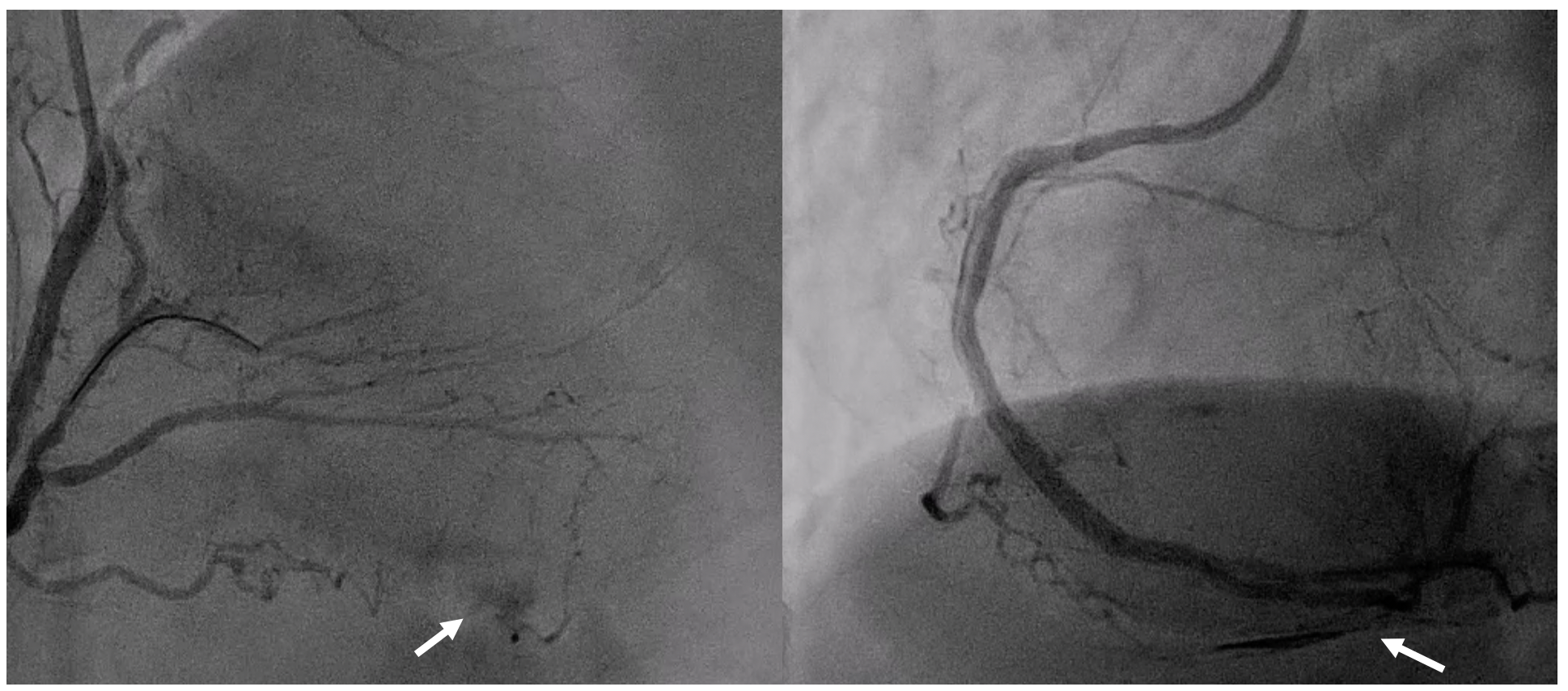
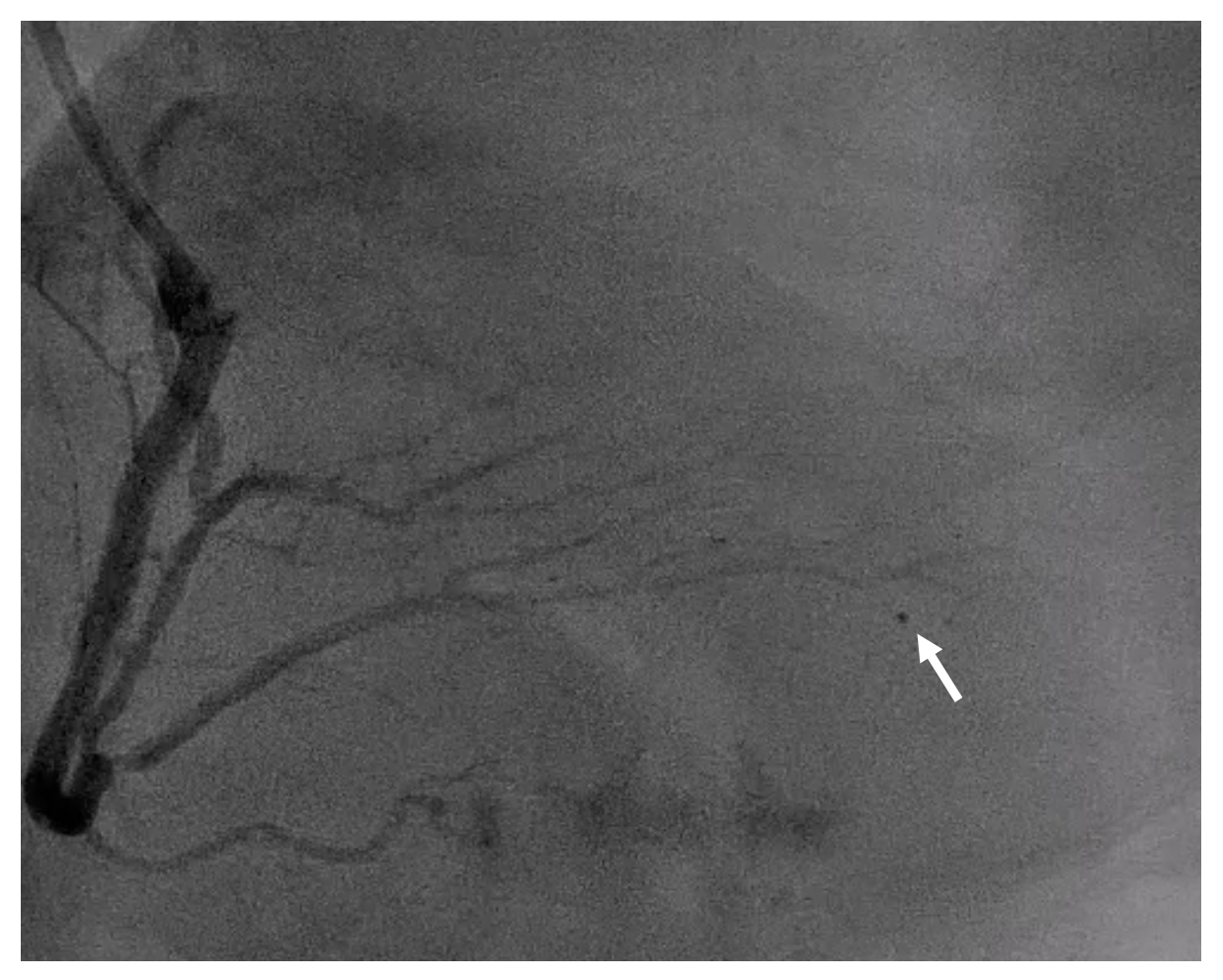
Staged PCI at CTO of mid RCA was done with antegrade approach using a 6-Fr system sheath with XBRCA guiding catheter via femoral artery. First, we used Fielder XT-R guidewire but was unable to pass the CTO. We then exchanged the guidewire to Gaia Next 2 which successfully passed the lesion but microcatheters (Finecross and Caravel) could not. Small balloon (Ryurei 1.0x5 mm) was then dilated up to 14 ATM, but lesion was undilatable. Tornus microcatheter was used but still unable to cross the distal cap of CTO. Rotational atherectomy with RotaLink Burr 1.25 mm, speed 180,000 RPM was attempted for 16 runs but failed. Again, Gaia Next 2 guidewire was used and Ryurei balloon 1.0x5 mm was successfully crossed the CTO. Buddy wire technique with Sion blue guidewire was used. NC Euphora balloon 2.5x15 mm with additional predilatation of 25 ATM was done at proximal to mid RCA. Gaia Next 2 guidewire was removed, and PCI with Sirolimus-Eluting stents 3.0x40 mm and 3.5x30 mm were done at mid and proximal RCA. Coronary angiogram after PCI showed PDA perforation suspected from Gaia Next 2 guidewire. Echocardiogram showed moderate amount of pericardial effusion without tamponade effects. We promptly placed Finecross microcatheter just proximal to the perforation site. Continuous negative suction from the microcatheter was done for 5 minutes which showed progressively disappearing extravasation. The final angiogram demonstrated good coronary blood flow to the PDA with no residual perforation.
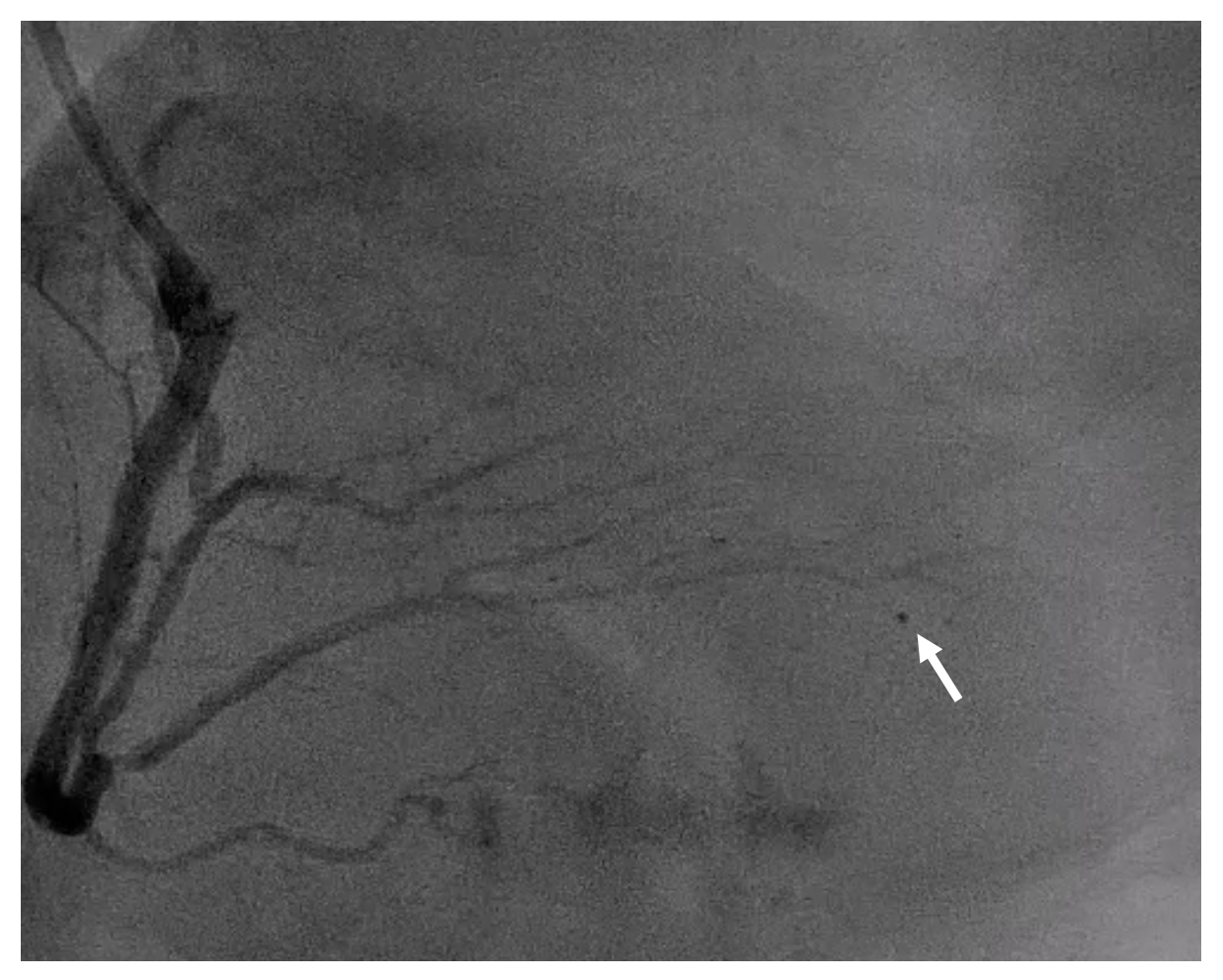
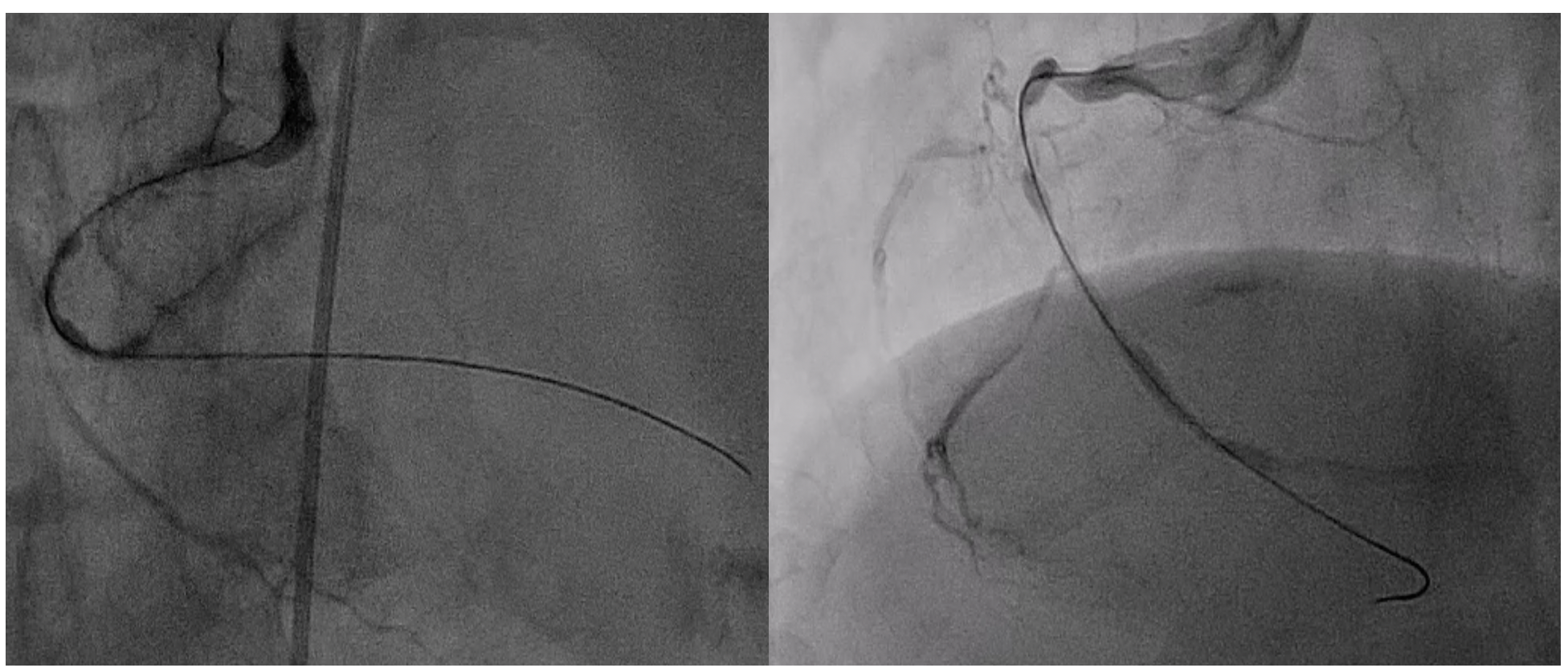
Case Summary
CTO PCI is associated with an increased risk of fatal complications including distal vessel perforation. Inadvertent or uncontrolled advancement of a guidewire can result in perforation, particularly stiff, tapered, and polymer-jacketed guidewires. Recommended treatment strategies include prolonged balloon inflation, fat or coils embolization, and covered stent implantation. In our case, we used continuous negative suction technique using microcatheter with indeflator which can control the perforation by limiting blood flow to perforation site. This approach may provide a novel and successful therapeutic option for distal vessel perforation, particularly in small vessel perforation.


