Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-151
Rebuilding After the Fall: A Case With Traumatic Subclavian Artery Occlusion
By Donna Shu-Han Lin
Presenter
Donna Shu-Han Lin
Authors
Donna Shu-Han Lin1
Affiliation
Shin Kong Wu Ho-Su Memorial Hospital, Taiwan1,
View Study Report
TCTAP C-151
ENDOVASCULAR - Peripheral Vascular Disease and Intervention
Rebuilding After the Fall: A Case With Traumatic Subclavian Artery Occlusion
Donna Shu-Han Lin1
Shin Kong Wu Ho-Su Memorial Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
G3xxx66
Relevant Clinical History and Physical Exam
A 70-year-old man presented at the clinic with left arm numbness
for one month. His past medical history was significant for hypertension and type 2 diabetes, both of which were well-controlled. He admitted to have fallen at home three months prior to presentation but did not seek medical help at that time. Since one month ago, he started to note coldness and numbness throughout his left arm, followed by progressive gangrene of the second finger after a small cut in the finger (figures A, B).




Relevant Test Results Prior to Catheterization
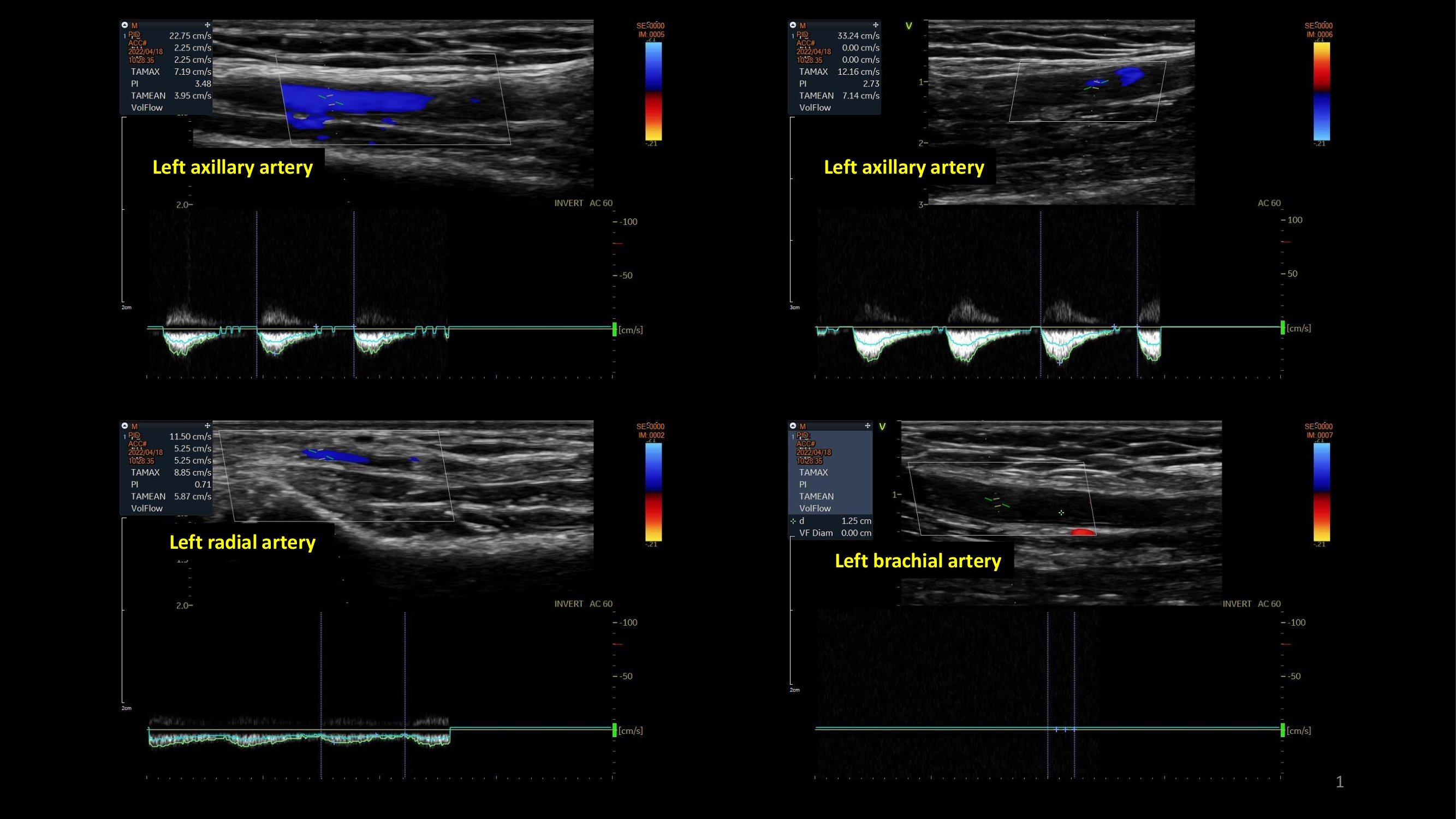
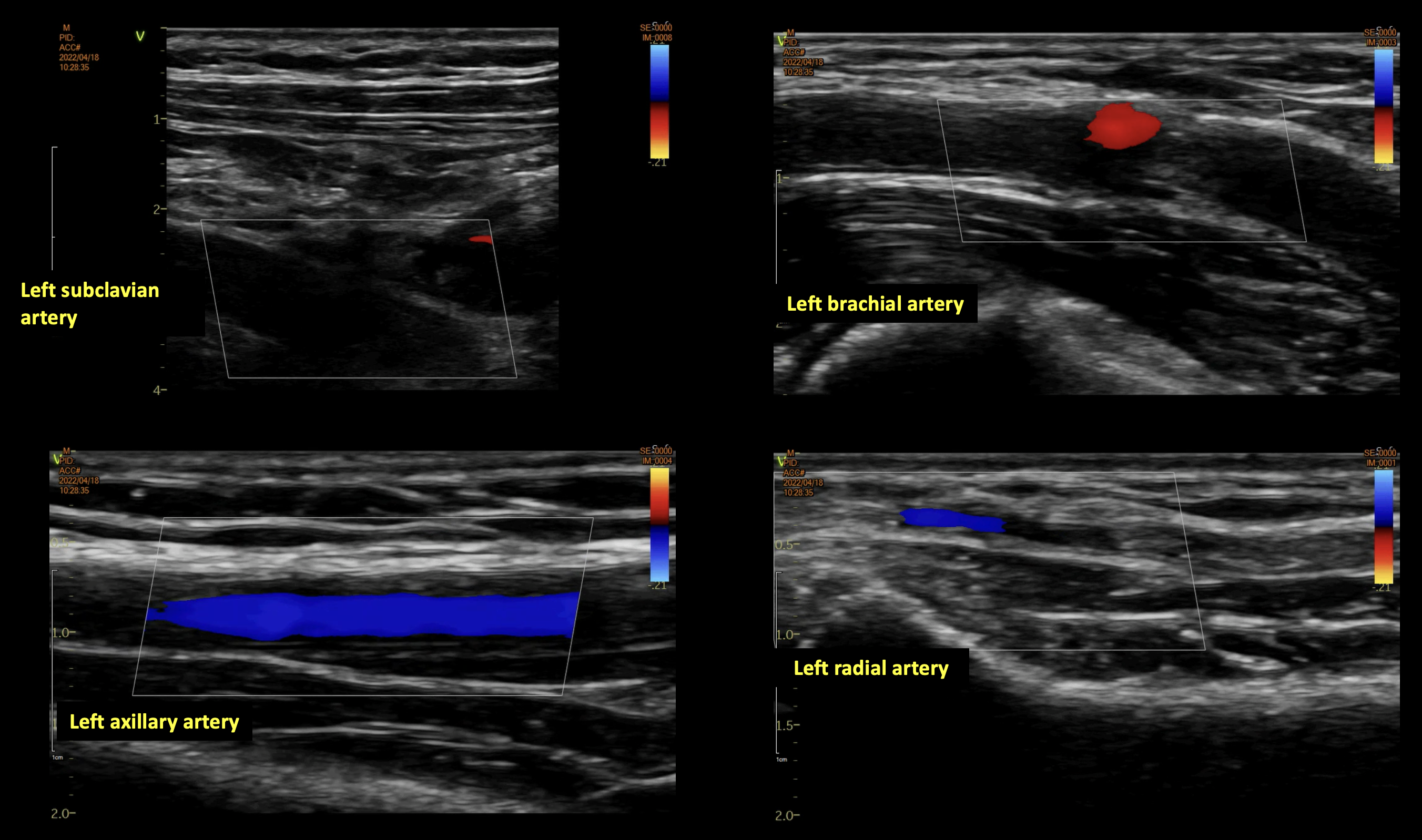
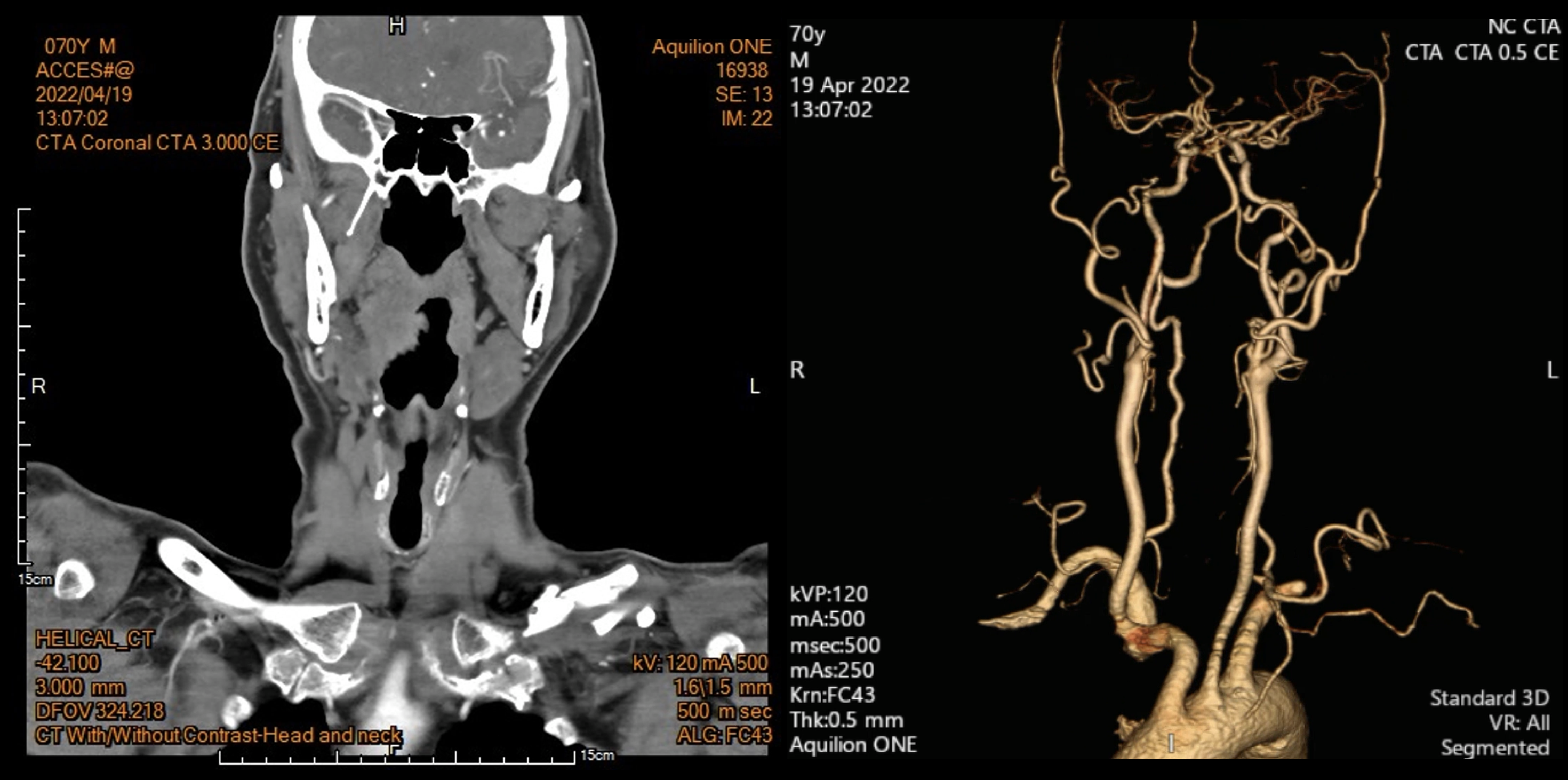
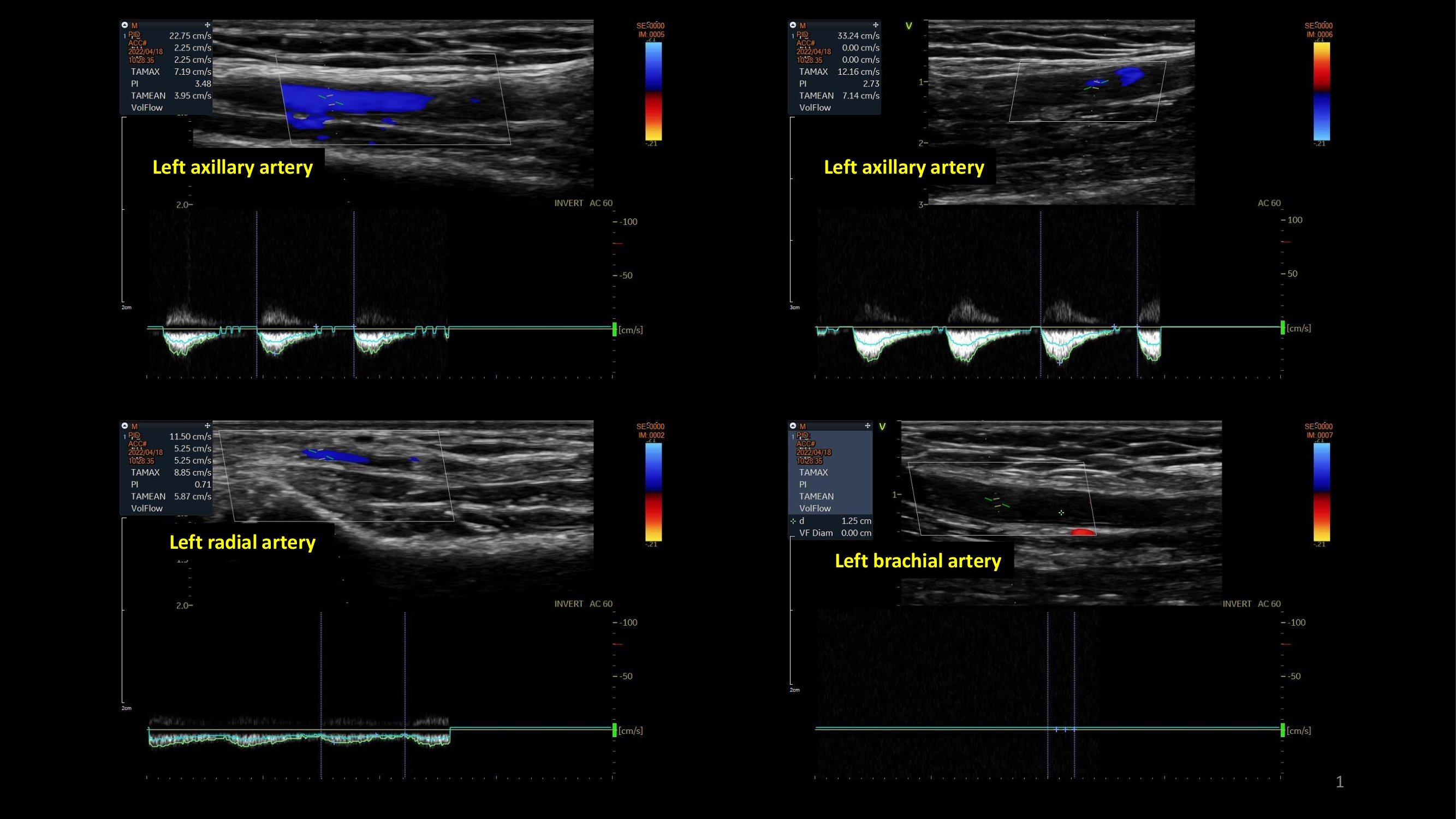
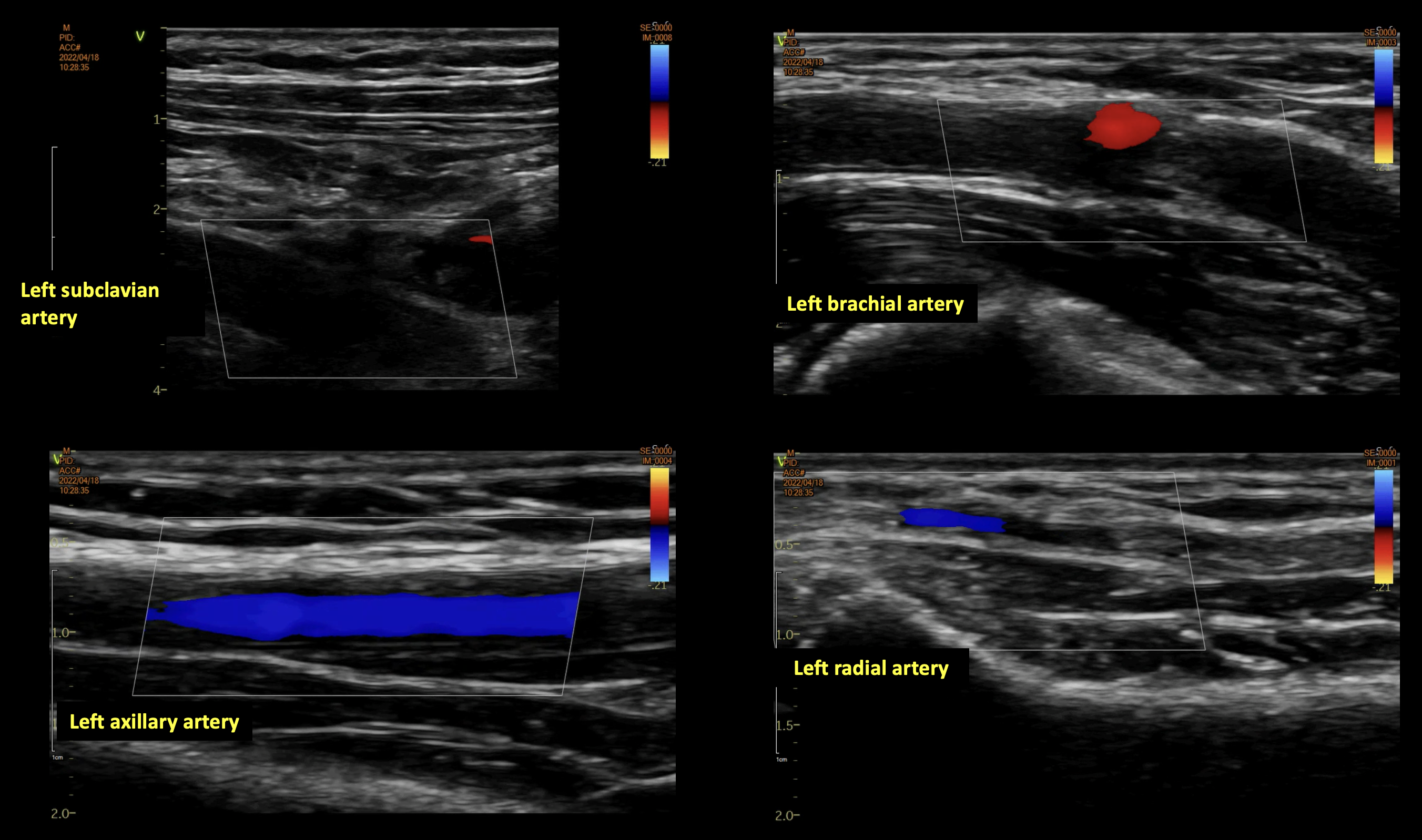
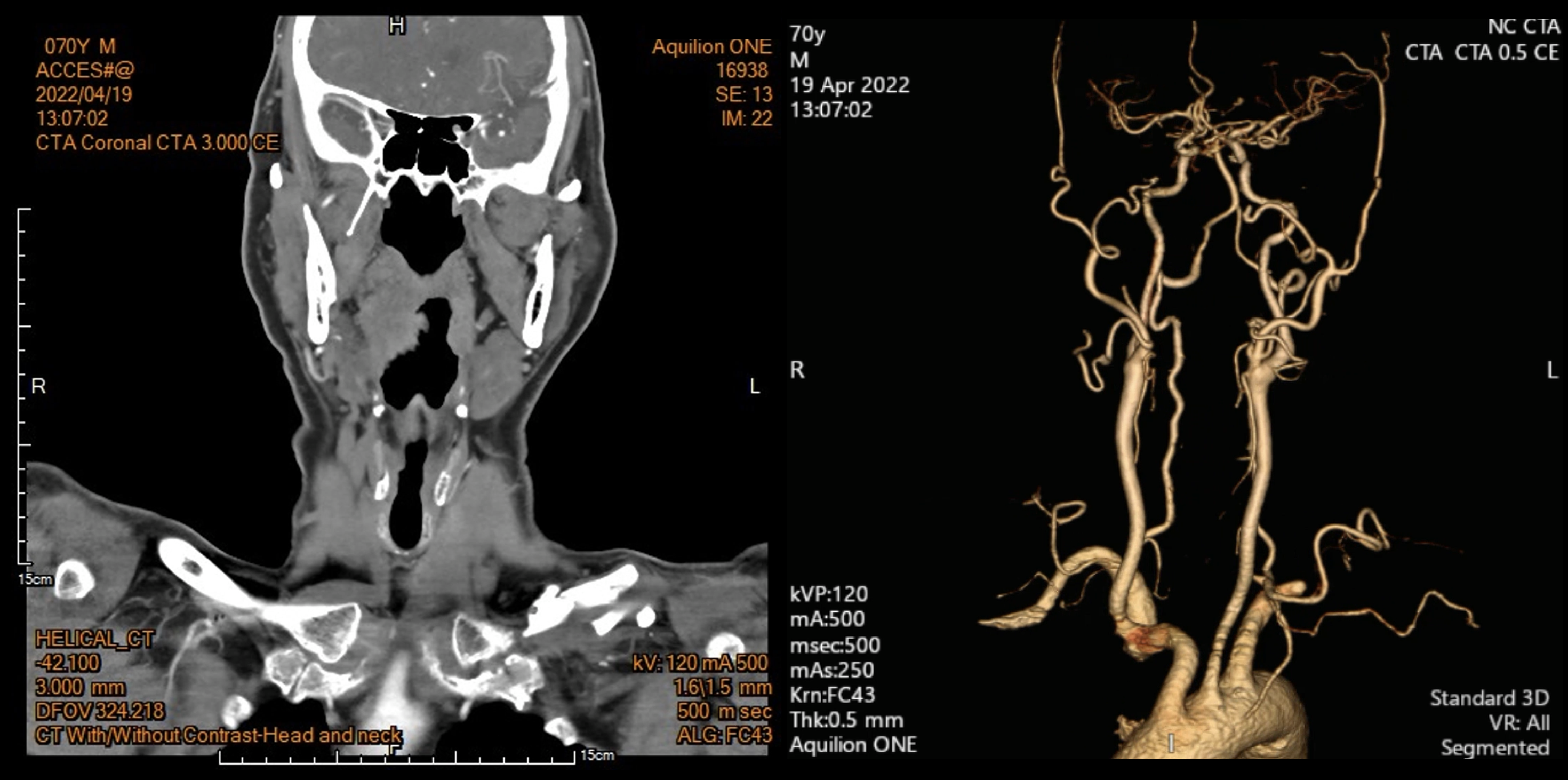
Vascular duplex of the upper limbs found occlusion of the left subclavian artery, with very poor flow throughout the left axillary, brachial, radial and ulnar arteries (figures C, D). A CT was arranged and found left clavicular fracture with non-union and surrounding hematoma, with occlusion of the left subclavian artery without involvement of the left vertebral artery (figure E).
Relevant Catheterization Findings
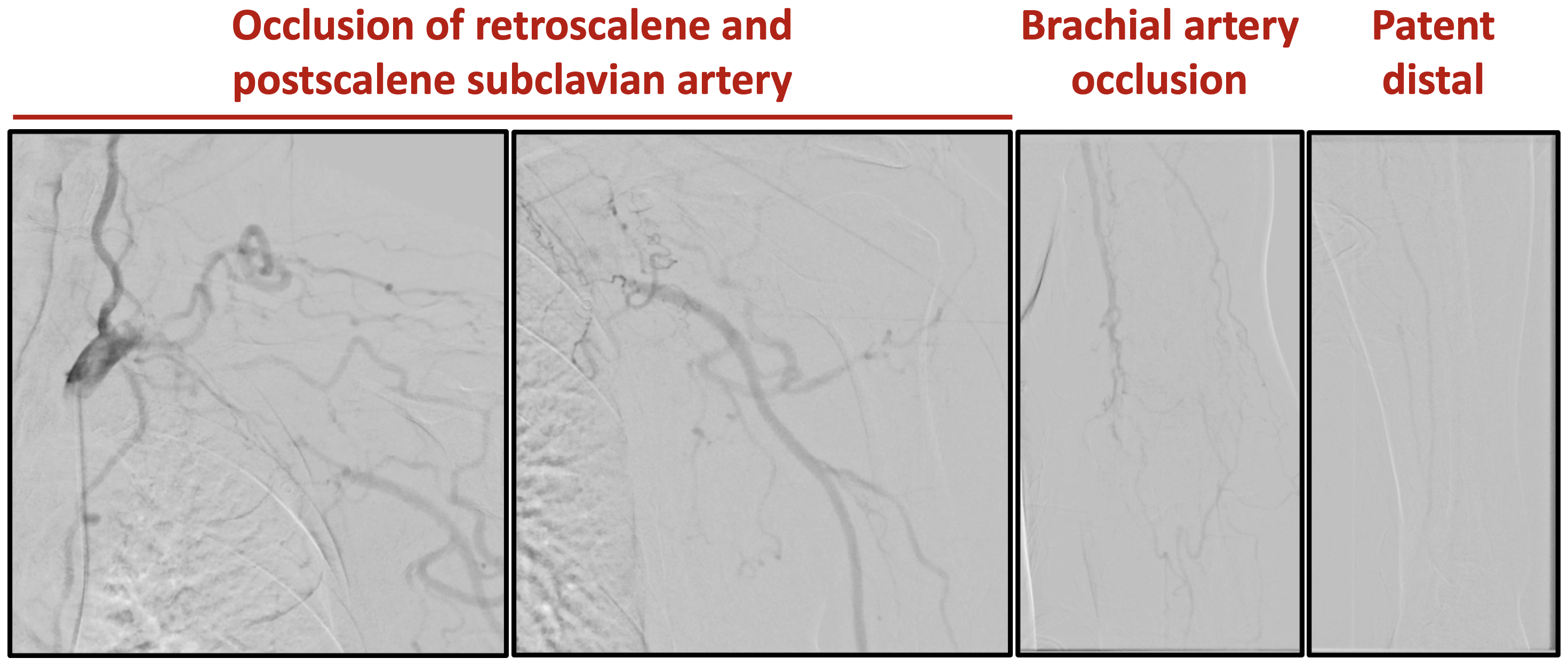
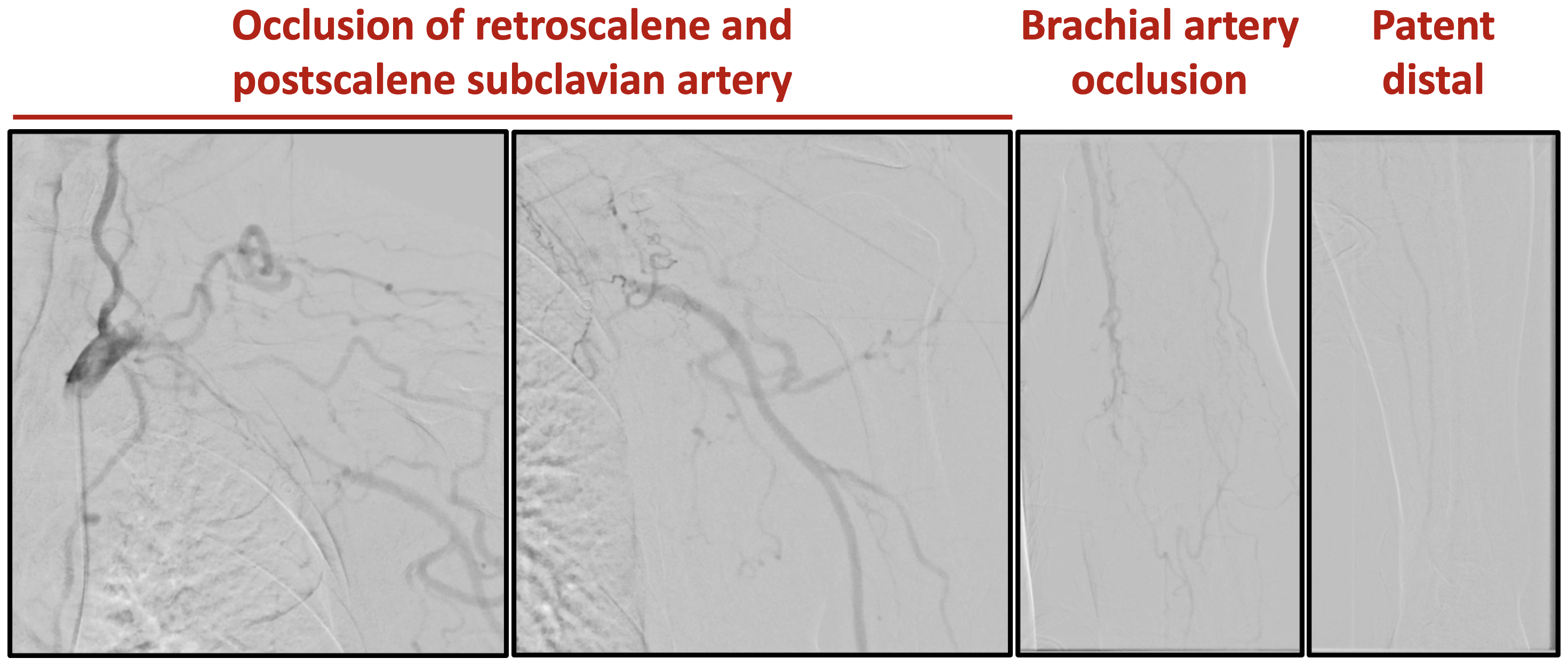
Left clavicular fracture with subclavian artery extravasation, pseudoaneurysm formation followed by thrombosis was suspected. Diagnostic angiography confirmed preserved left vertebral artery, occlusion of the retroscalene and postscalene subclavian artery, with recanalization in the axillary artery (figure F). The brachial artery also seemed occluded or stenosed.
Interventional Management
Procedural Step
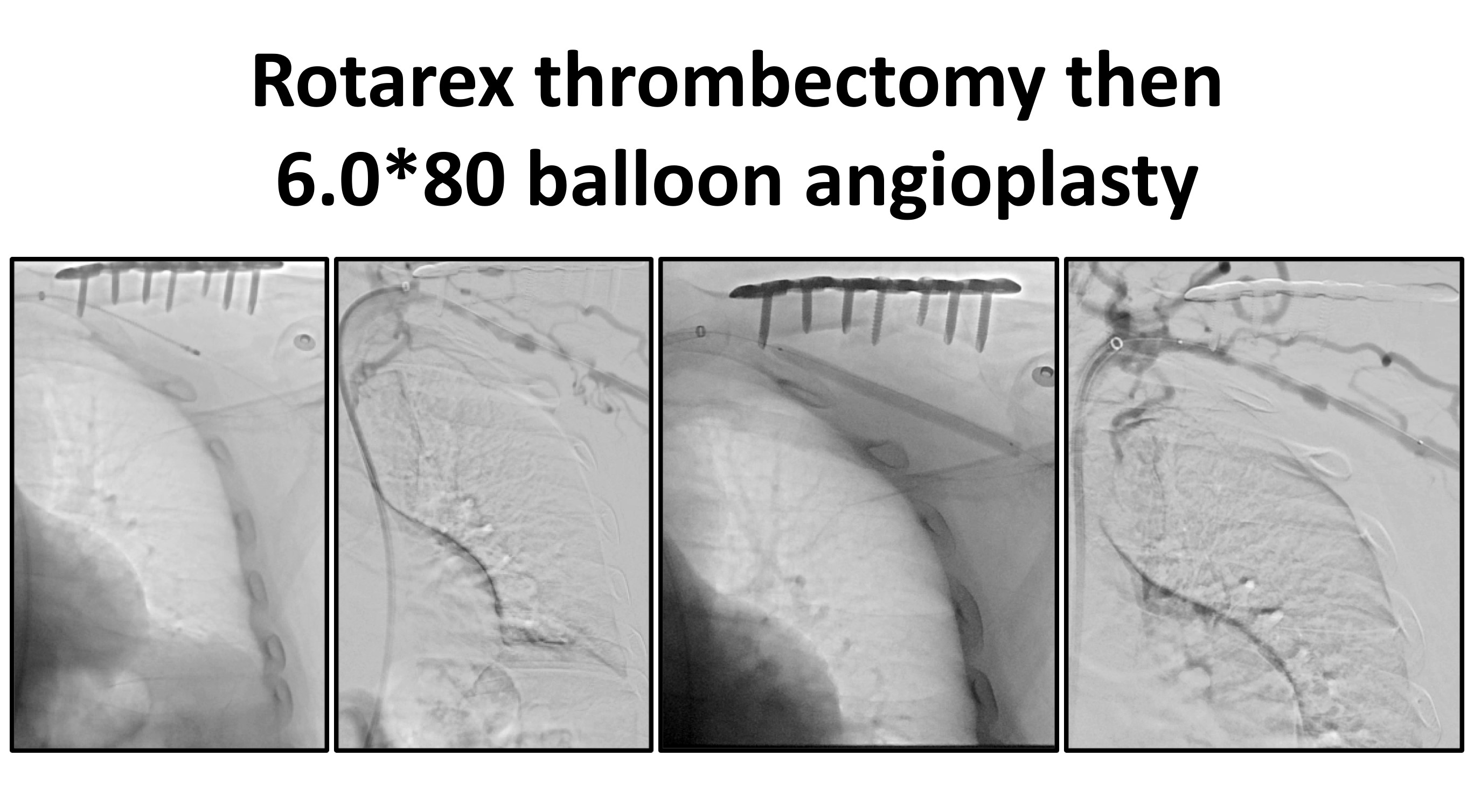
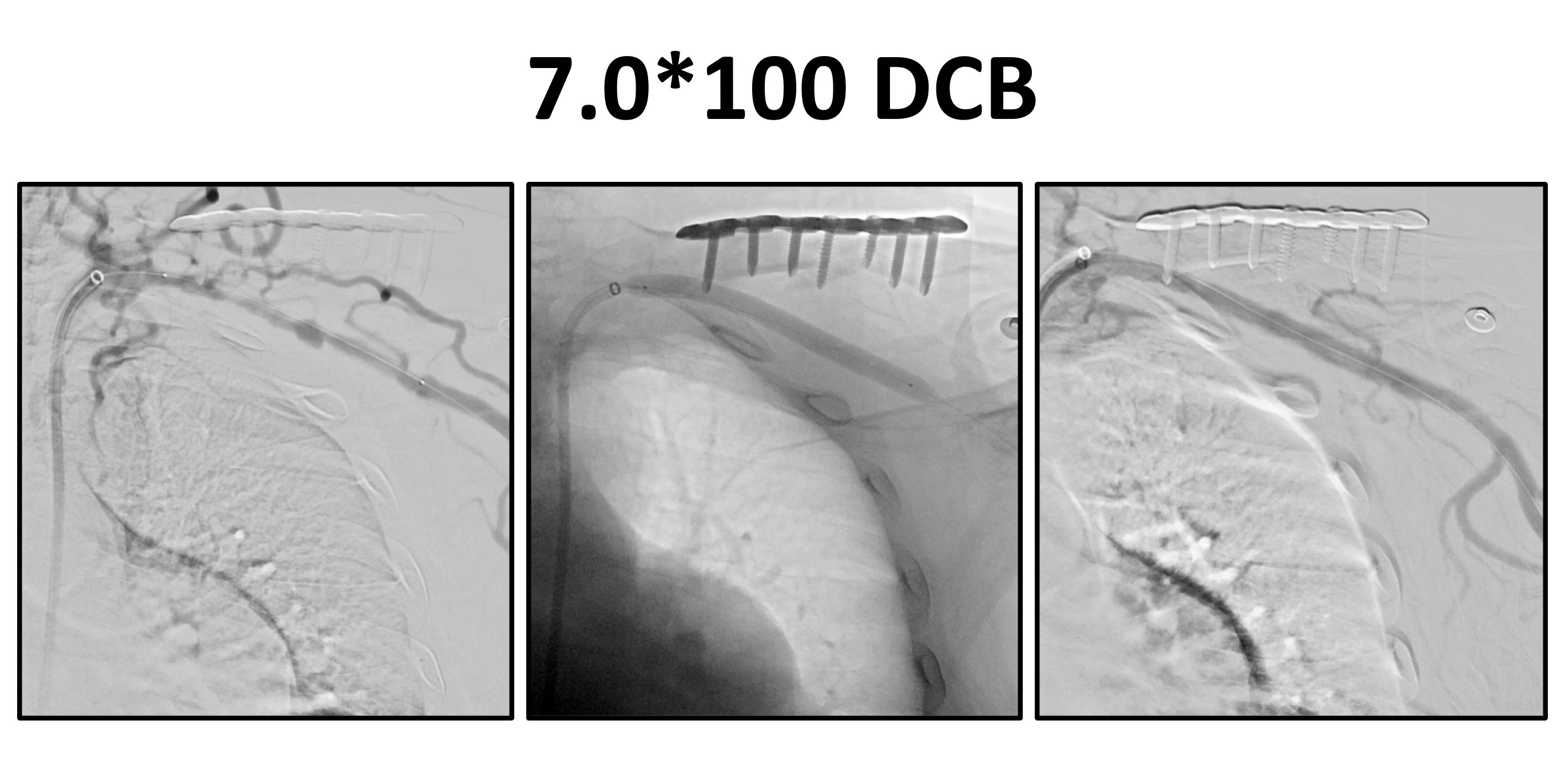
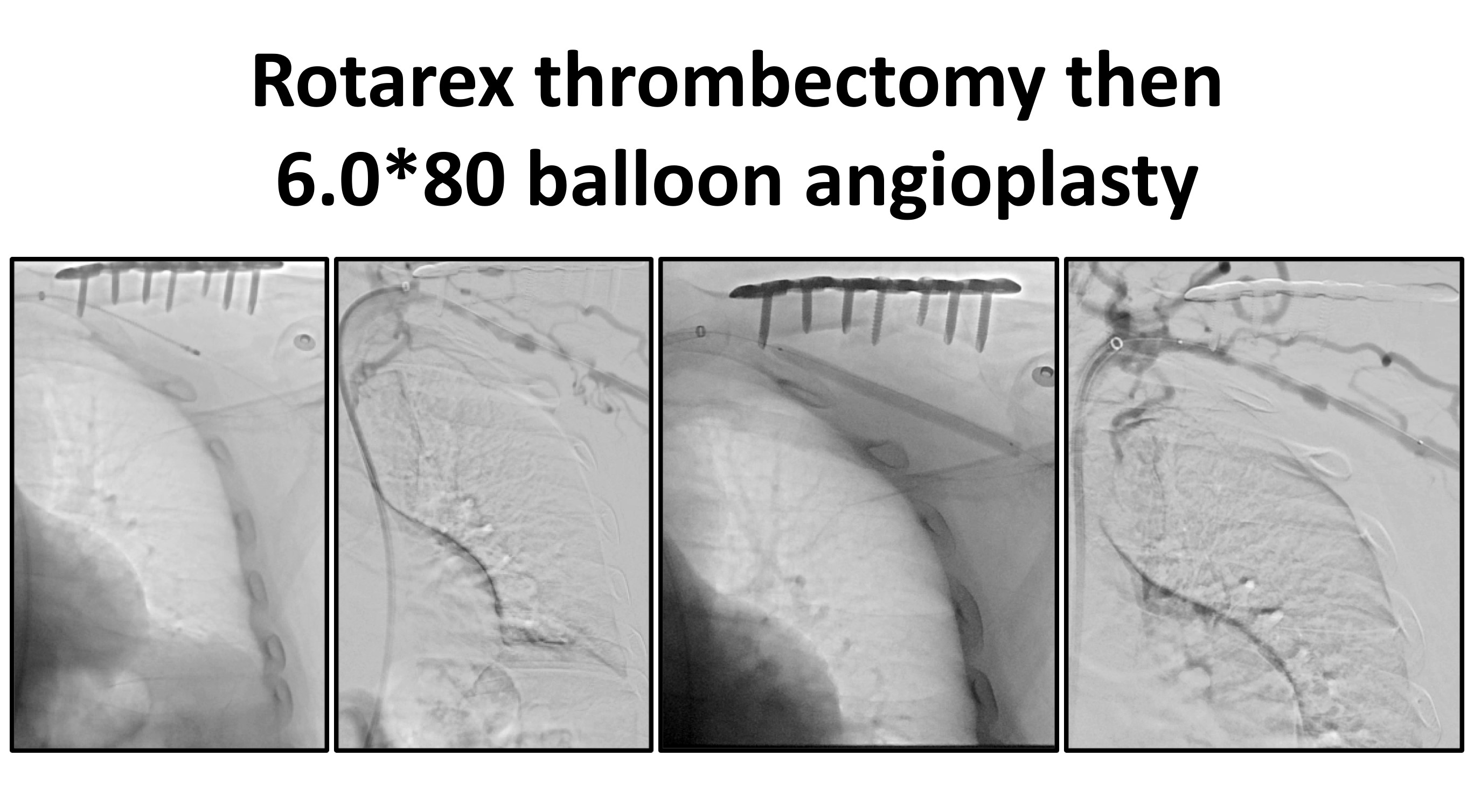
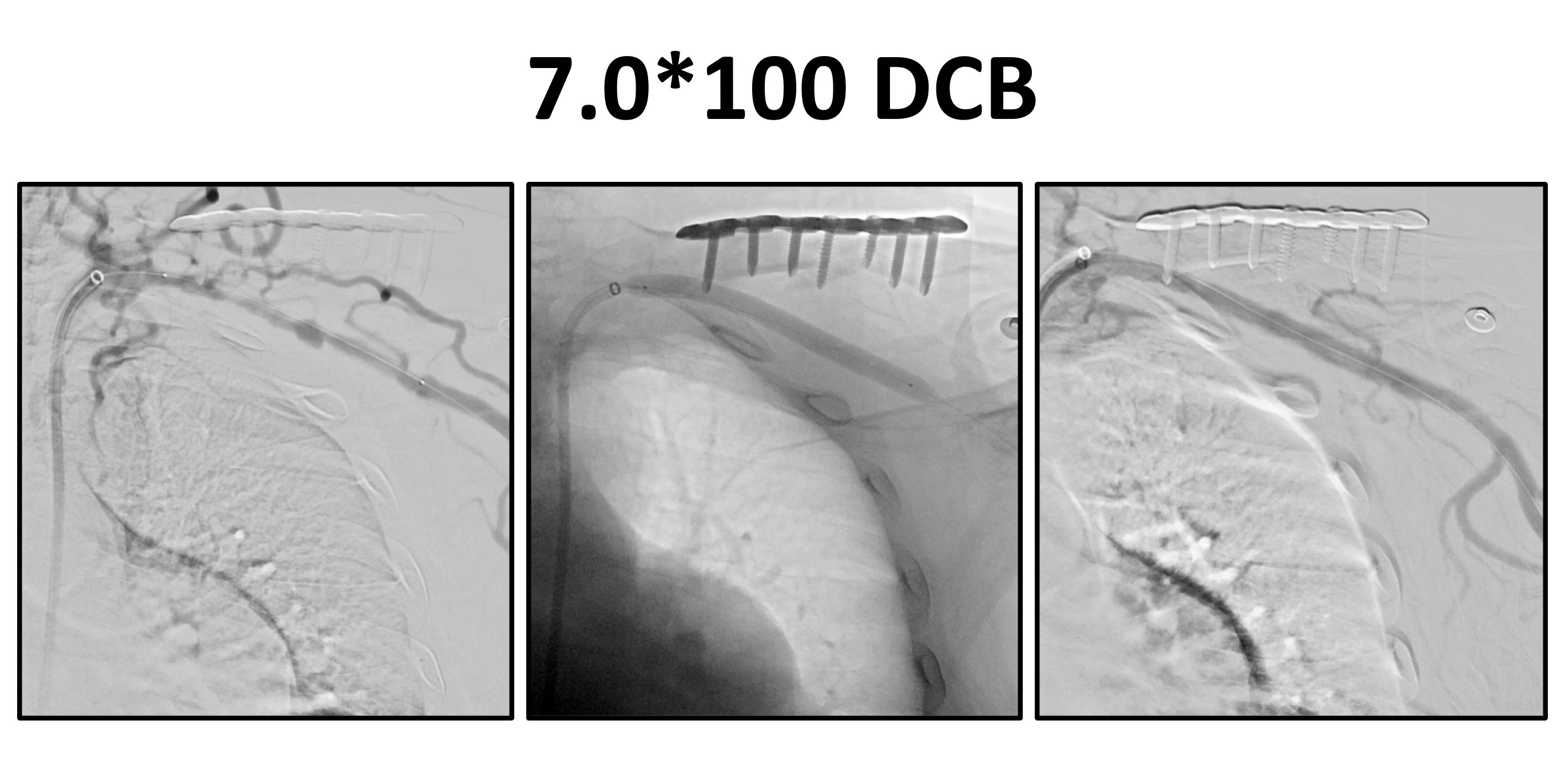
The patient first received open reduction and internal fixation of his fracture. Left clavicular fracture with fragmented bone and hematoma at the fracture site but intact vessels were found intraoperatively. Because the CTO was likely due to thrombosis more than atherosclerosis, intraluminal wiring followed by thrombectomy and balloon angioplasty was planned. Started with an 8Fr antegrade system (8Fr 90cm sheath, 6Fr JR4 catheter, CXI 2.3*150 microcatheter) with a Gladius 0.014” then switched to Halberd 0.014” wire. However, distal cap of the CTO was difficult to penetrate. Attempted retrograde attack via the ulnar artery but failed to cross the brachial area. Returned to antegrade approach and finally entered the axillary artery with an Astato XS 20 wire. Dilated the entire CTO with an 2.0*15 balloon and checked IVUS. Performed thrombectomy with 6Fr Rotarex throughout the CTO, then 6.0*80 balloon angioplasty (figure G). Wired through the brachial artery CTO with Gladius 0.014” and entered the radial artery with knuckle technique. Sequential balloon dilatation from the radial to brachial arteries with 3.0*120 and 4.0*120 balloons but still poor flow was noted. IVUS showed heavy IMH in the brachial artery and further angioplasty was deferred. The subclavian artery was finally treated with a 7.0*100 DCB with good results (figure H). Good finger growth and triphasic blood flow in left arm arteries were evident 8 weeks later (figure I).
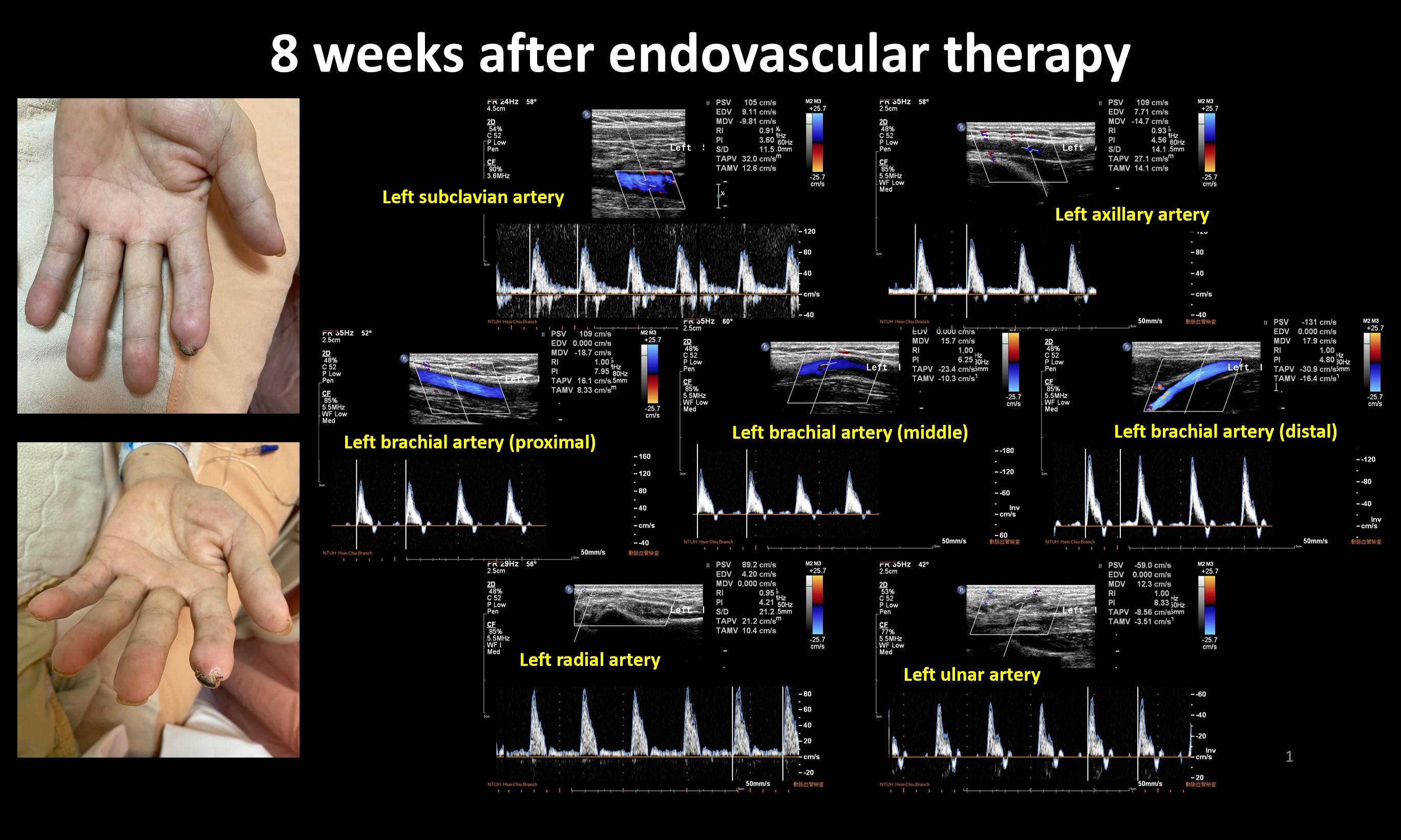
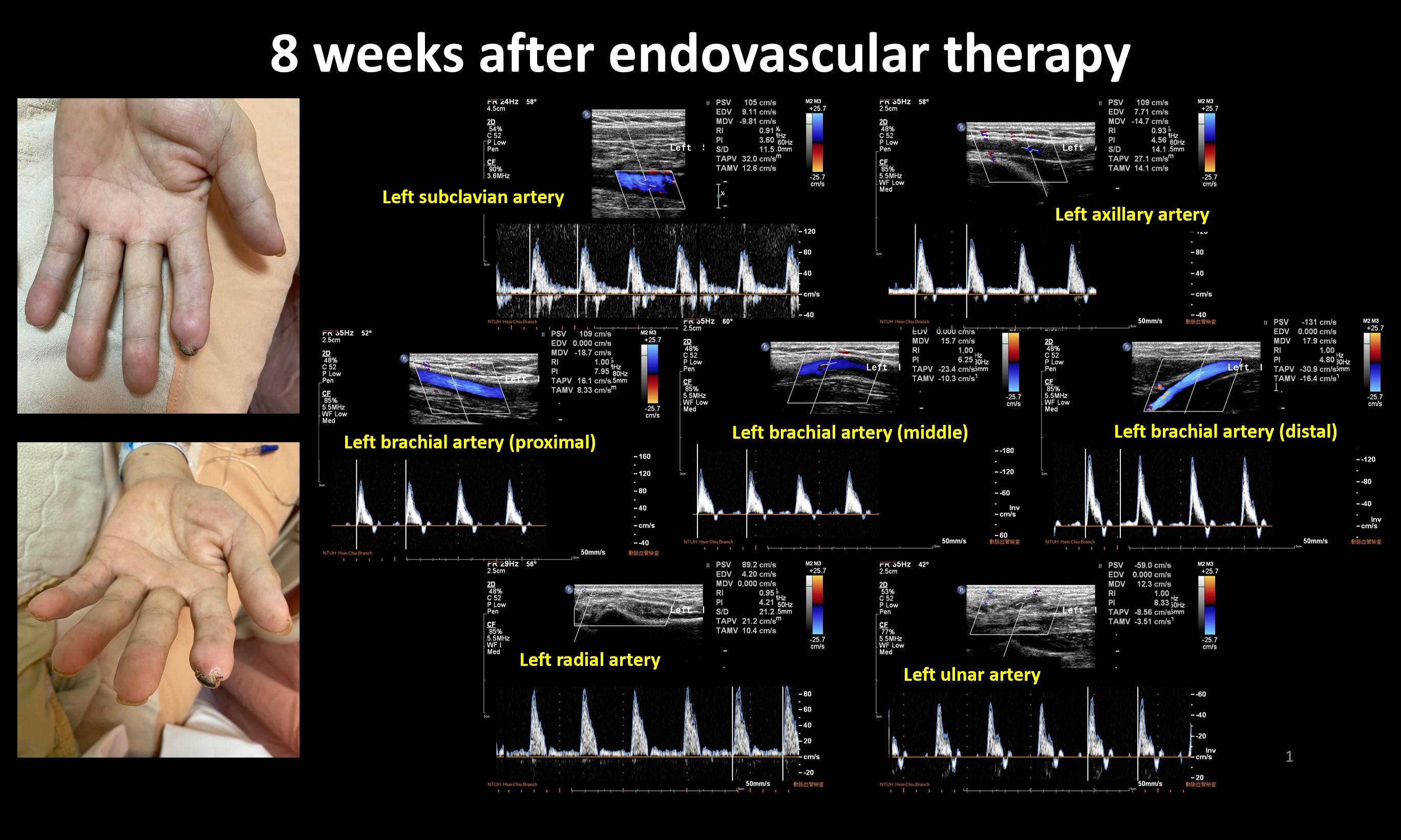
Case Summary
Presentation of subclavian artery thrombosis after clavicular injuries may be delayed, with thrombosis and stenosis likely both playing a role in late onset vascular occlusion. In vascular occlusions due to trauma-related thrombosis, thrombectomy and atherectomy devices may avoid the need for stenting if vessels are grossly intact after the injury. Although the pathogenesis of trauma-related vascular thrombosis differs from most atherosclerotic peripheral artery disease, intimal hyperplasia may occur after vascular injury for which drug-coated devices may be beneficial. Individualized treatment is crucial for patients with traumatic vascular injury to optimize outcomes.


