Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-027
When Do We Do PCI to CTO Instead of Culprit Lesion in Patients With ACS?
By Sheng-Fu Liu, Mu-Yang Hsieh, Hsien-Li Kao
Presenter
Sheng-Fu Liu
Authors
Sheng-Fu Liu1, Mu-Yang Hsieh2, Hsien-Li Kao2
Affiliation
National Taiwan University Hospital Hsin-Chu Branch, Taiwan1, National Taiwan University Hospital, Taiwan2,
View Study Report
TCTAP C-027
CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS)
When Do We Do PCI to CTO Instead of Culprit Lesion in Patients With ACS?
Sheng-Fu Liu1, Mu-Yang Hsieh2, Hsien-Li Kao2
National Taiwan University Hospital Hsin-Chu Branch, Taiwan1, National Taiwan University Hospital, Taiwan2,
Clinical Information
Patient initials or Identifier Number
Mr. Tseng, 85 year-old gentleman
Relevant Clinical History and Physical Exam
An 85-year-old gentleman was a case of coronary artery disease with 3 vessels disease who received off-pump coronary artery bypass (SVG1: Ao-LAD, SVG2: Ao-Dx-OM-PDA) in 2014. In 2021, he suffered from non-ST-elevation myocardial infarction and his diagnostic angiography showed partial graft failure. Then he received POBAS to SVG1. This time, acute chest pain happened to him at night.
PE: compression chest pain with diaphoresis
PE: compression chest pain with diaphoresis
Relevant Test Results Prior to Catheterization
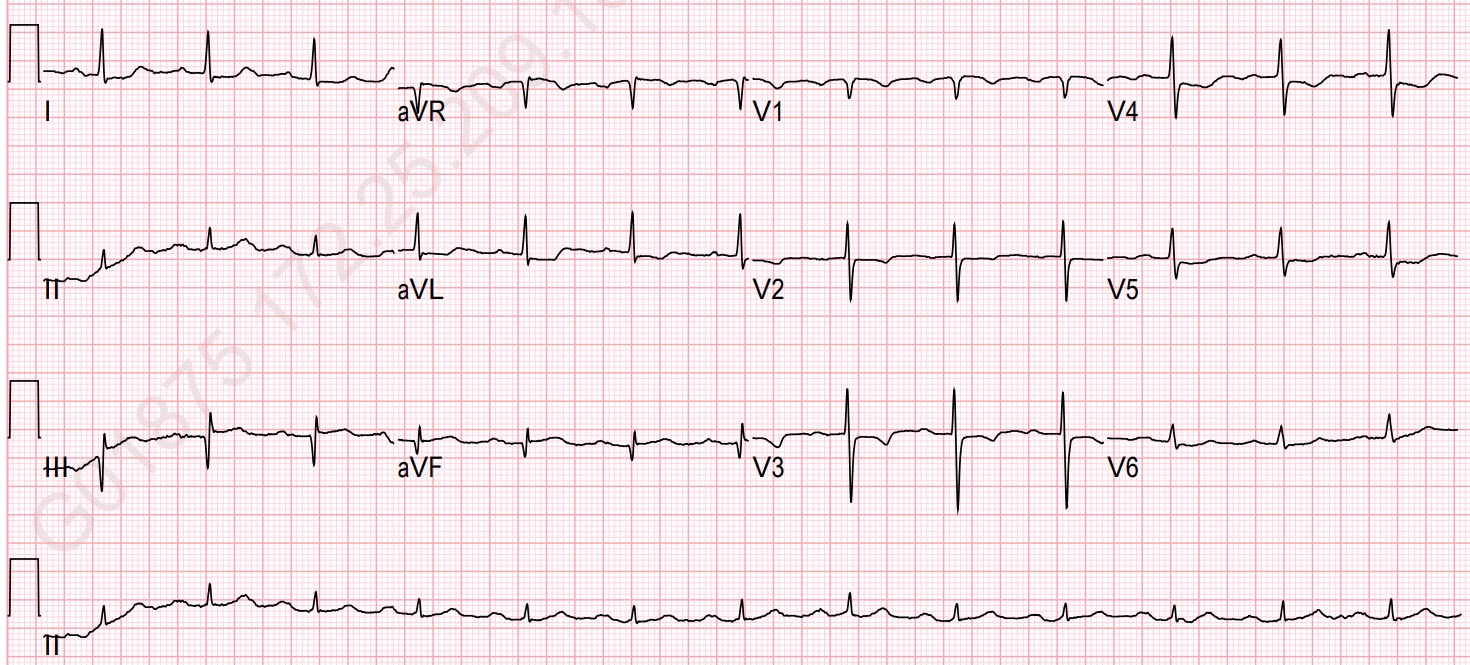
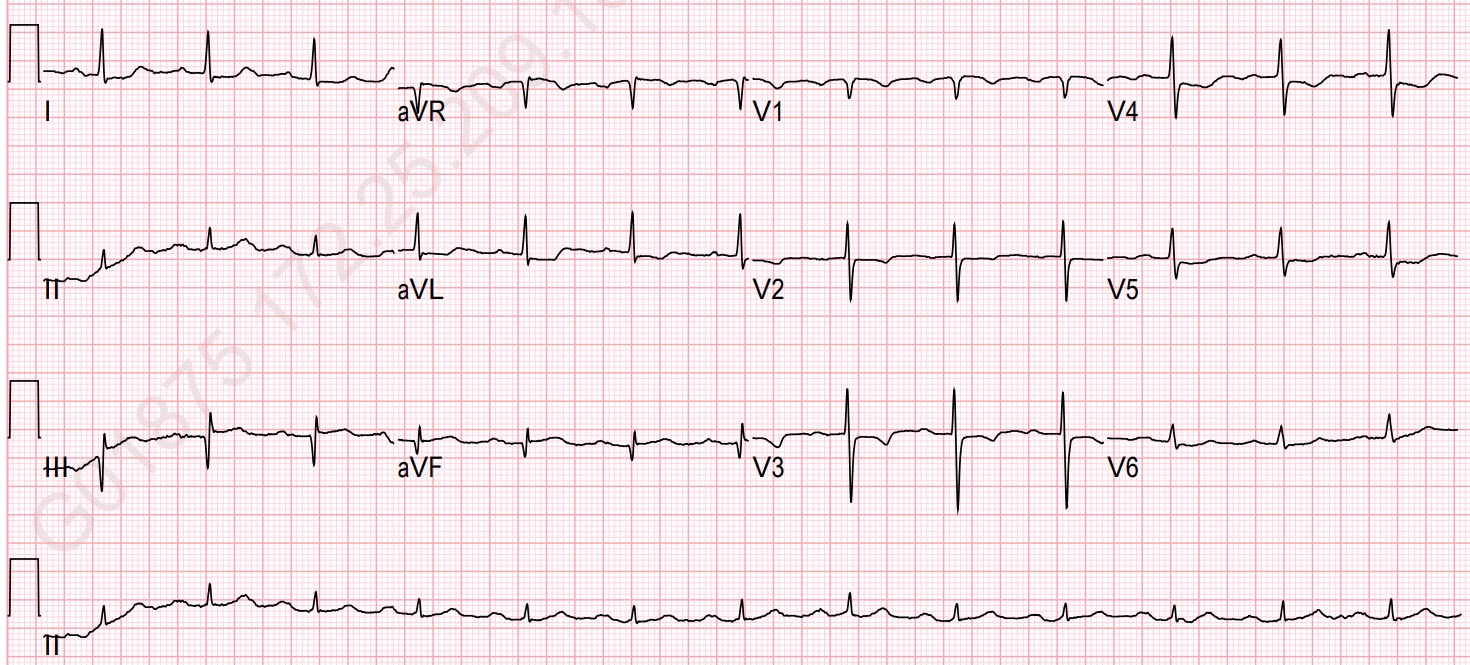
EKG at 01:52 in 8/30:ST depression and T wave inversion in V2~V5, I and aVLq wave in III and aVF
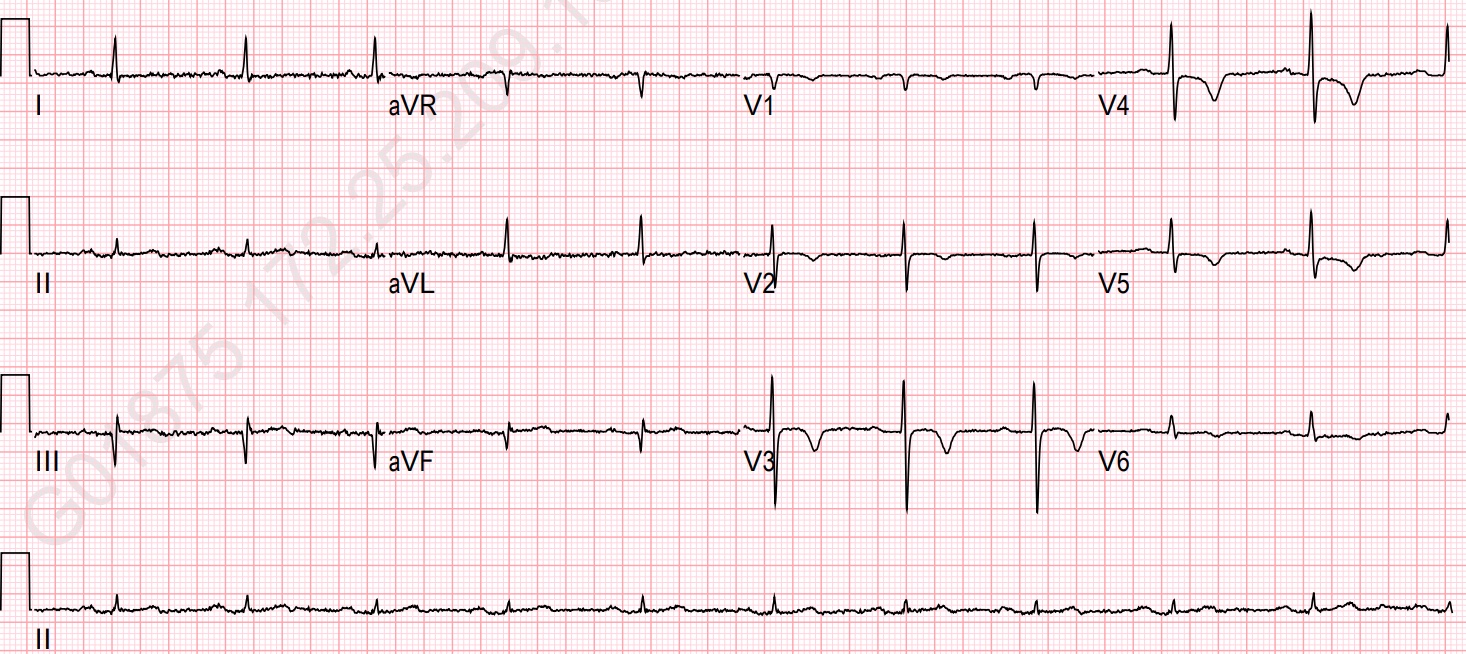
EKG at 06:03 in 8/30:Dynamic ST-T change in V2~V6, I and aVL
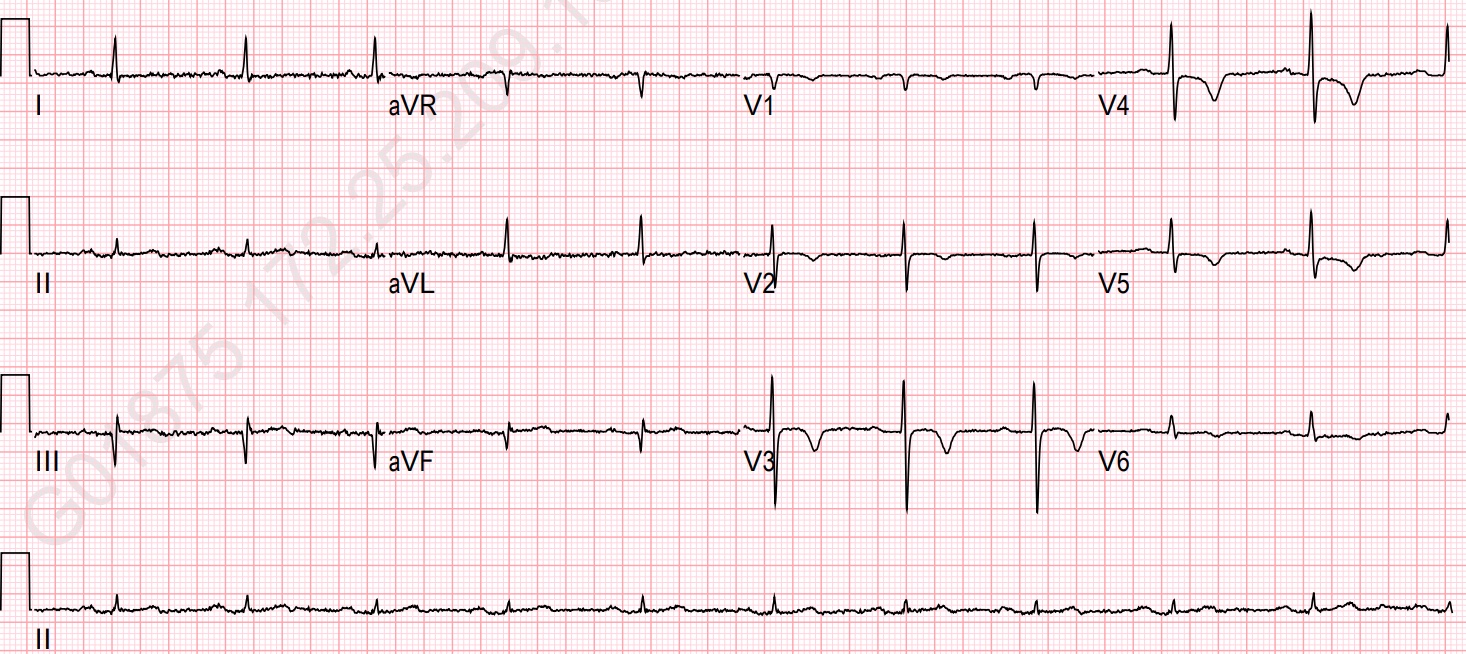
EKG at 06:03 in 8/30:Dynamic ST-T change in V2~V6, I and aVL
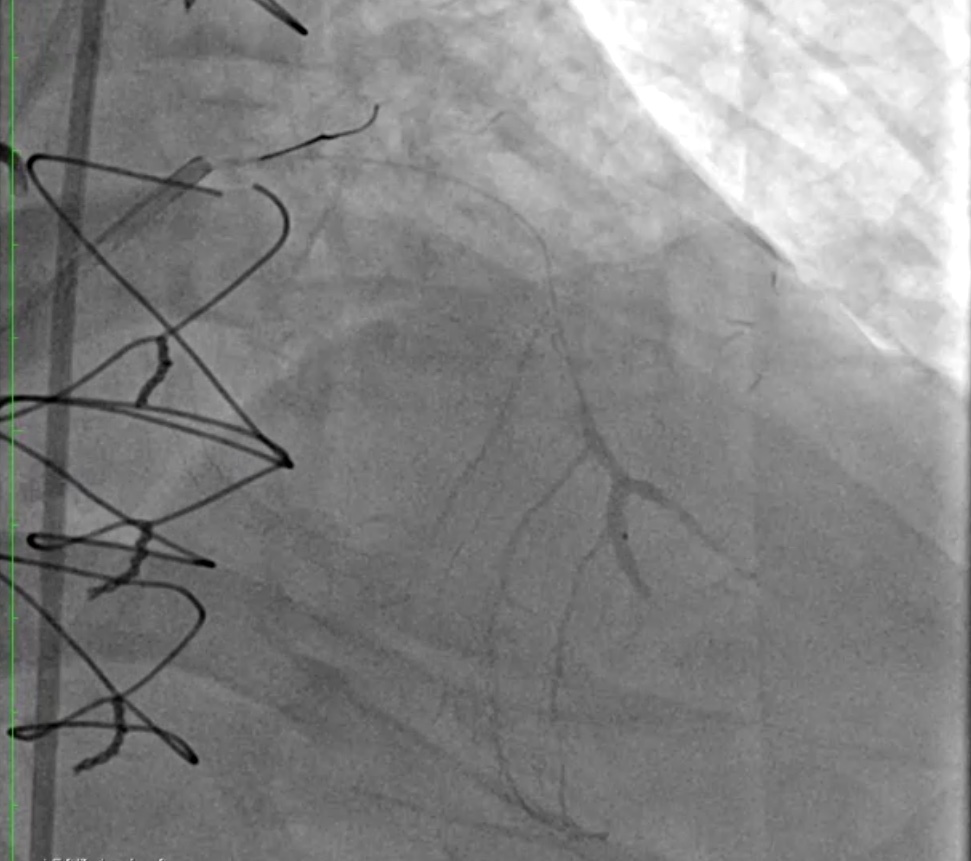
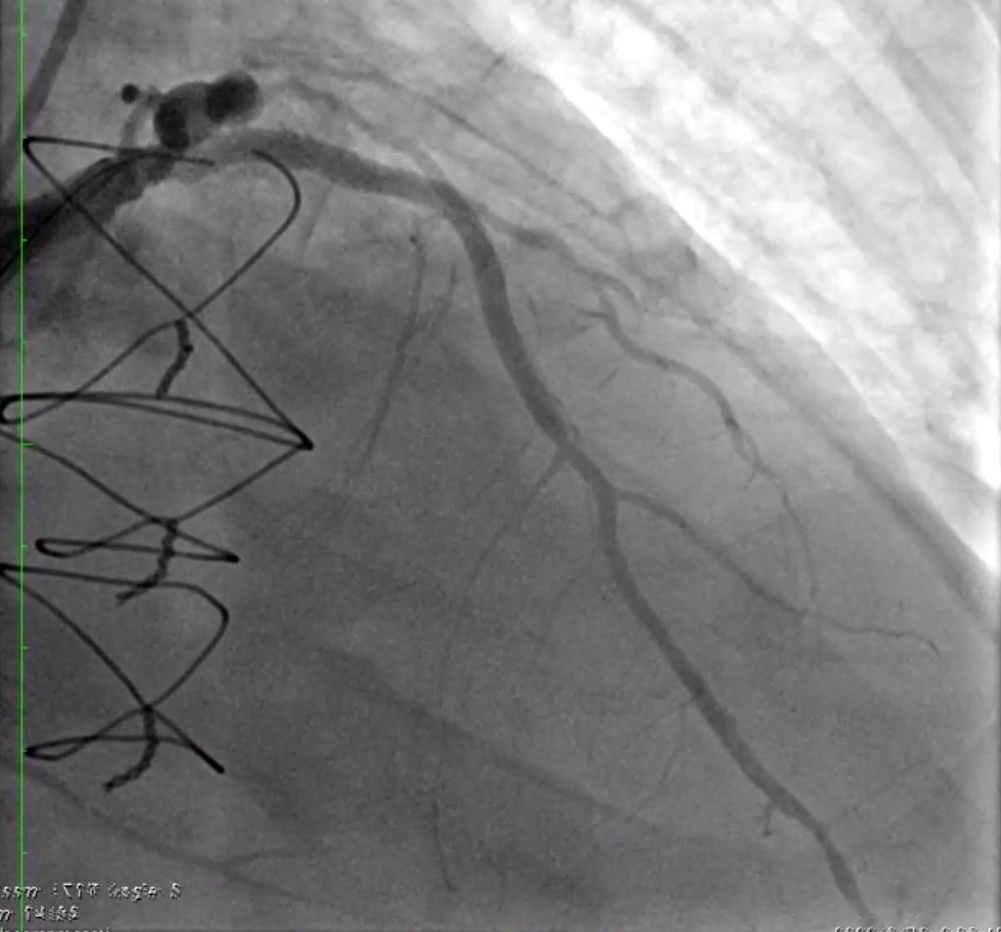
Relevant Catheterization Findings
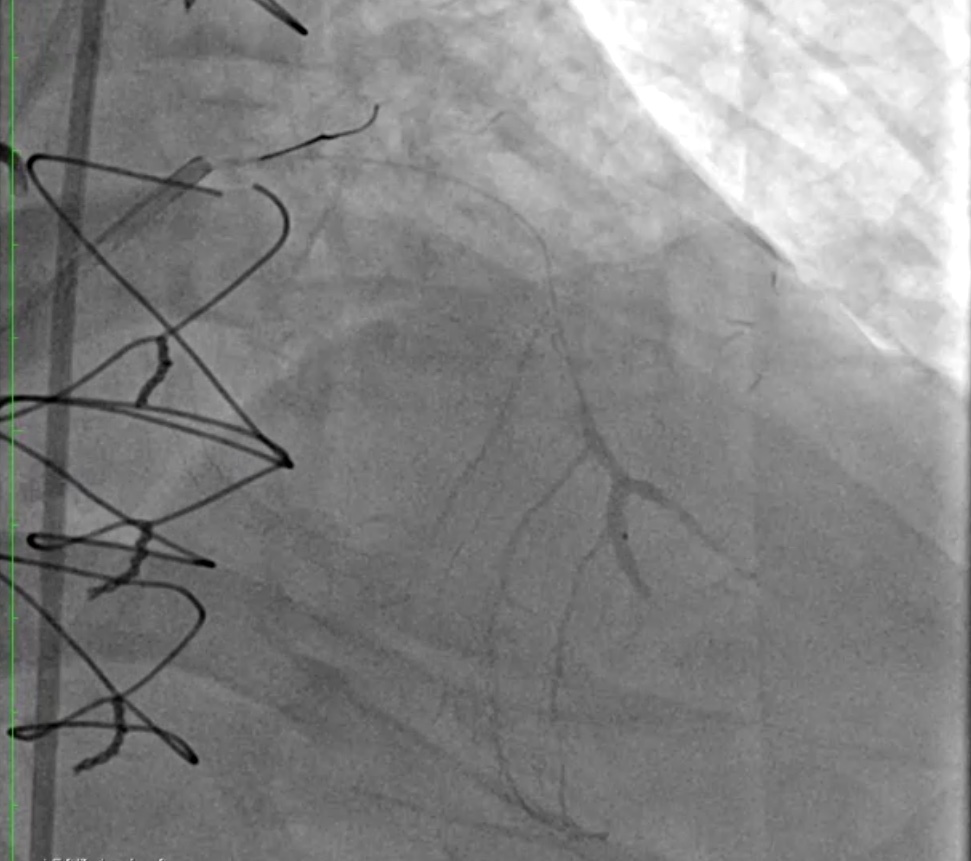
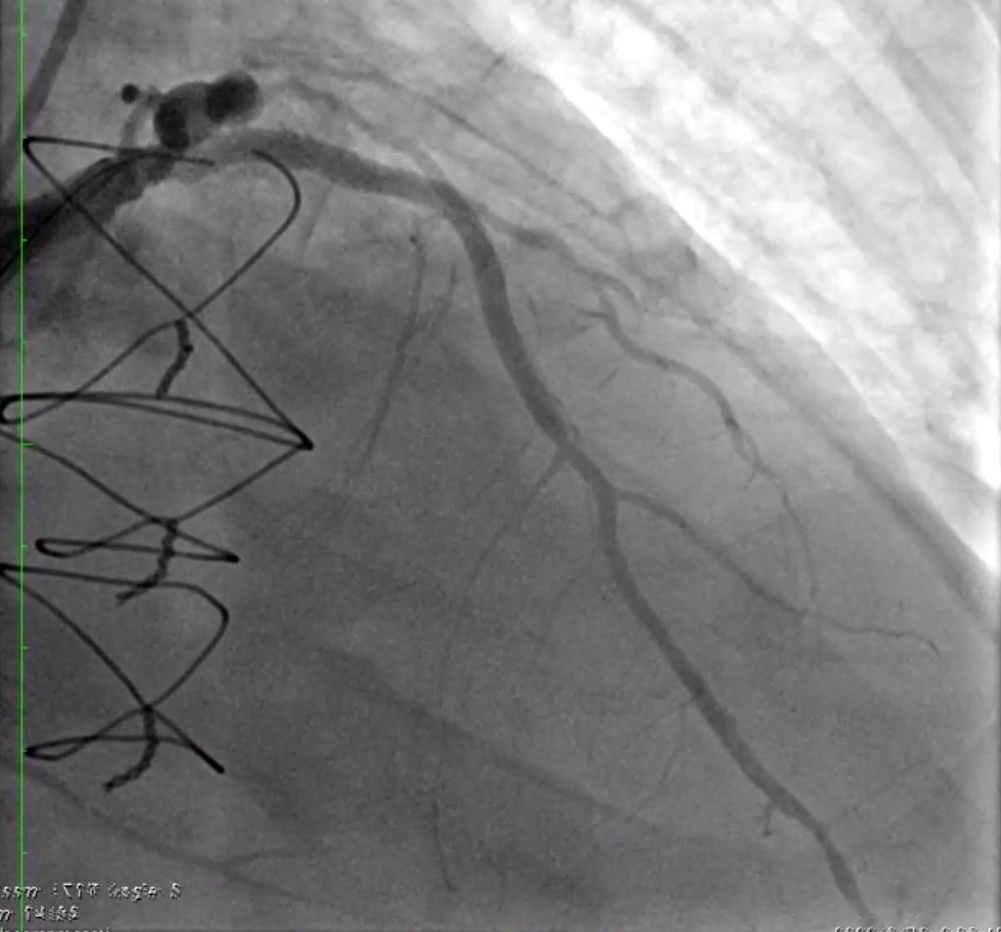
LM: dLM: 30% stenosisLAD: pLAD: 90% stenosis mLAD: chronic total occlusionLCX: pLCX: ectasia, with collateral to RCA OM: 90% stenosis dLCX: chronic total occlusion, with intracoronary collateralsRCA: pRCA: chronic total occlusion dRCA / PLA / PDA: collateral from pLCXSVG1 (Ao-LAD): mid- no ISR anastomosis site- 90% stenosisSVG2 (Ao-DB-OM-PDA): Ao-DB: 90% stenosis DB-OM-PDA: graft occlusion






Interventional Management
Procedural Step
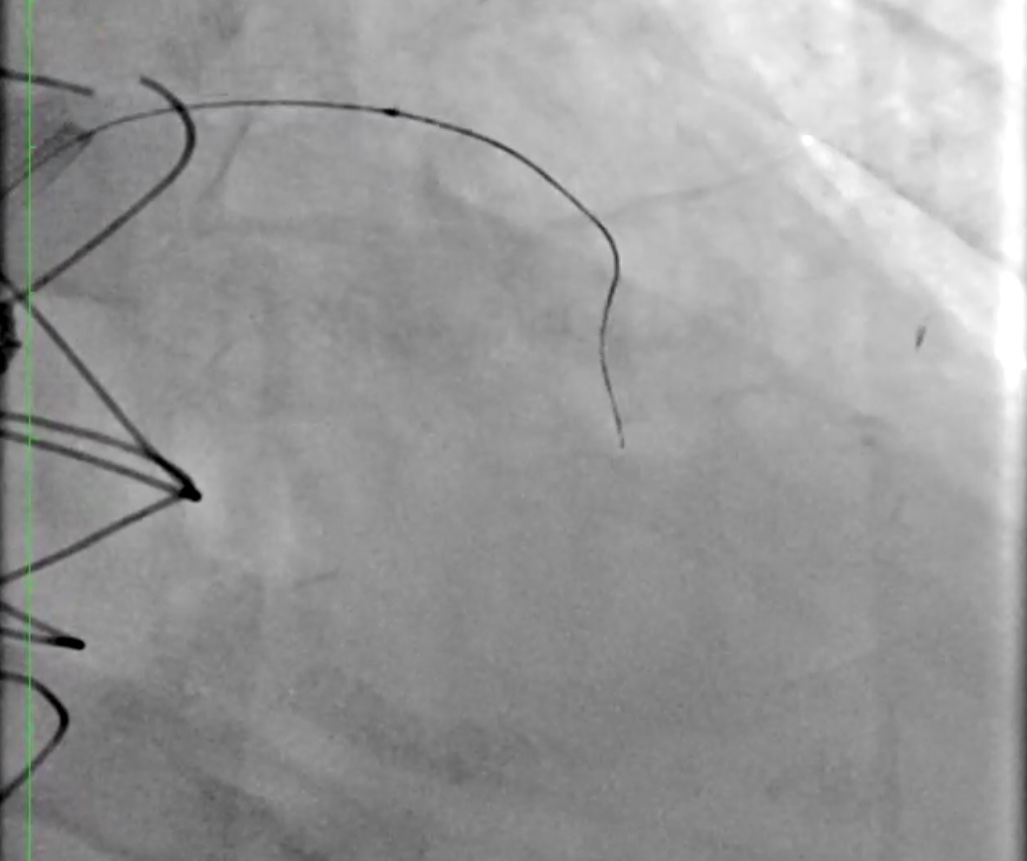
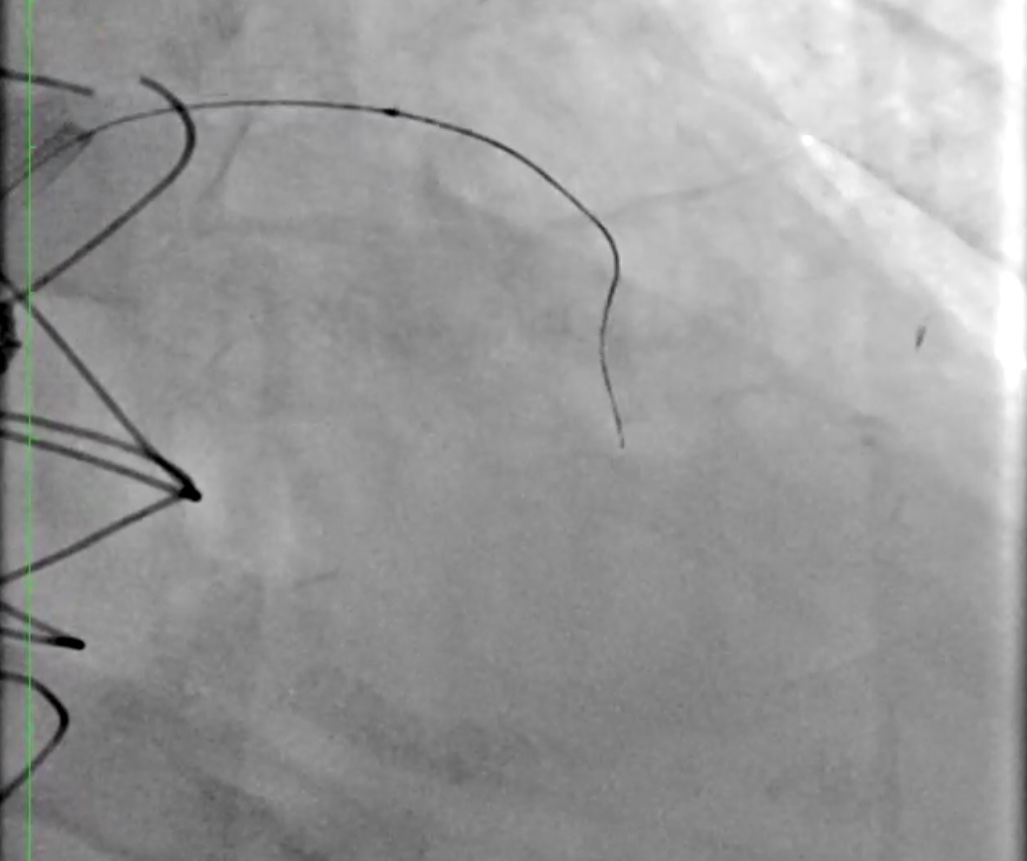
1. engage to LCA with GC 7Fr BL3.5 and to SVG with 6F AL1 2. do bilateral injection 3. try antegrade wiring with Gaiya 2 + Finecross, with success 4. do distal injection via finecross to confirm distal true lumen 5. switch workhorse wire to Sion 6. POBA to mLAD with BC 1.5x15, BC 2.5x15 7. check IVUS to LAD 8. POBA to mLAD with NC 3.0x20, c/w dissection 9. POBAS to mLAD with DES1 "Combo 2.75x33mm" 10. post dilatation with stent balloon 11. POBAS to LM-pLAD with DES2 "Synergy 3.5x32mm" 12. post dilatation to stent junction with stent balloon 13. do antegrade and retrograde angio to confirm flow compromised at SVG-LAD anastomosis sitebecause the patient presents chest pain14. POBA to SVG-LAD anastomosis site with BC 2.0x20 with antergrade flow recovery 15. give Morphine IV for pain control 16. POBA to SVG-LAD anastomosis site with CB "Wolverine 2.0x10mm", c/w no flow 17. POBAS to SVG-LAD anastomosis site with DES3 "Xience Sierra 2.0x15mm" 18. post dilatation with stent balloon 19. post dilatation to dLAD stent, with NC 2.0x8mm, up to 20A10" 20. post dilatation to mLAD stent, with NC 2.75x15mm, up to 22A5" 21. post dilatation to pLAD / mLAD stent junction, with NC 3.0x15mm, up to 20A7" 22. check IVUS to LAD 23. post dilatation to pLAD and LM-pLAD stent with NC 3.5x15mm, up to 20A6" 24. perform POT to LM stent with NC 5.0x8mm, up to 20A4" 25. check IVUS 26. final result is good, up to TIMI 3 flow
Case Summary
Interventional cardiologists should evaluate patients comprehensively. Culprit lesion evaluation is crucial during complicated percutaneous coronary intervention. Although the culprit lesion is anastomosis site, percutaneous coronary intervention to native chronic total occlusion is more effective and safer than to graft anastomosis sites in CABG patients with acute coronary syndrome.


