Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-090
The Last Man Standing: Emergency High Risk PCI to LM-LCX
By Wei Liang Lee, Jayakhanthan Kolanthaivelu, Yee Sin Tey, Ting Yuen Beh
Presenter
Wei Liang Lee
Authors
Wei Liang Lee1, Jayakhanthan Kolanthaivelu2, Yee Sin Tey1, Ting Yuen Beh1
Affiliation
National Heart Institute, Malaysia1, Cardiovascular Sentral Kuala Lumpur, Malaysia2,
View Study Report
TCTAP C-090
CORONARY - Complex and Higher Risk Procedures for Indicated Patients (CHIP)
The Last Man Standing: Emergency High Risk PCI to LM-LCX
Wei Liang Lee1, Jayakhanthan Kolanthaivelu2, Yee Sin Tey1, Ting Yuen Beh1
National Heart Institute, Malaysia1, Cardiovascular Sentral Kuala Lumpur, Malaysia2,
Clinical Information
Patient initials or Identifier Number
RP
Relevant Clinical History and Physical Exam
Mr RP, a 61 year-old diabetic, was referred from a district hospital following a resuscitated ventricular fibrillation. His ECG showed ST elevation at aVR lead, suspicious of left main stem occlusion.His vital signs were stable, BP 130/65, Heart rate 78/minLungs and heart auscultation were unremarkable.
Relevant Test Results Prior to Catheterization
Echocardiography showed severely impaired LVEF 20%, dilated LV with global hypokinesia, and mild mitral regurgitation.
Creatinine 79 umol/lHemoglobin 15.2 x10^12/lHbA1c 7.3%
Creatinine 79 umol/lHemoglobin 15.2 x10^12/lHbA1c 7.3%
Relevant Catheterization Findings
LM: Tight distal stenosis LAD: Chronic total occlusion from ostium LCX: Tight ostial stenosisRCA: Chronic total occlusion from ostium
Intra-aortic balloon pump was inserted for hemodynamic support
He was referred to surgeon for consideration of coronary artery bypass grafting surgery. However, deemed ineligible for surgical revascularization.He has frequent angina and ventricular tachycardia in ward. Decision for high risk angioplasty was made after discussing with patient and family members.



Intra-aortic balloon pump was inserted for hemodynamic support
He was referred to surgeon for consideration of coronary artery bypass grafting surgery. However, deemed ineligible for surgical revascularization.He has frequent angina and ventricular tachycardia in ward. Decision for high risk angioplasty was made after discussing with patient and family members.



Interventional Management
Procedural Step
PCI to Right Coronary Artery (RCA):Guiding catheter: SAL 0.75/6FrAttempted to cross lesion with coronary wire Fielder XT & Gaia II with Caravel Microcatheter Support. Unsuccessful, and abandoned.
PCI to Left Anterior Descending Artery (LAD):Guiding catheter EBU 3.5/7Fr, Coronary wire Runthrough to LCXAttempted to cross lesion with coronary wire Fielder XT & Fielder XT-A with Supercross Microcatheter Support. Unsuccessful and abandoned.
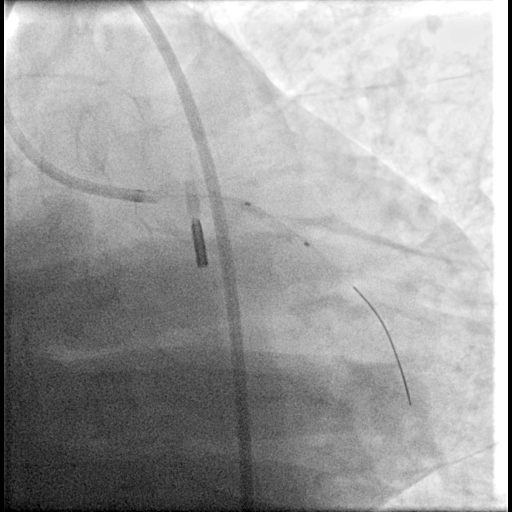
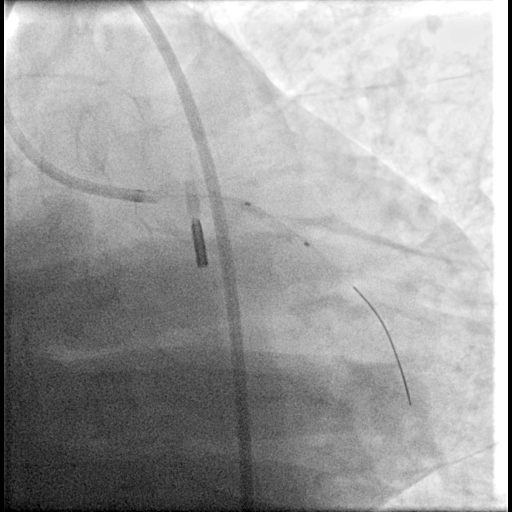
PCI to Left Circumflex Artery (LCX):Patient developed ventricular tachycardia/ventricular fibrillation while advancing balloon pass the left main coronary artery. Cardiopulmonary resuscitation performed and patient was mechanically ventilated. Transvenous temporary pacing catheter was inserted.
Pre-dilated ostial LCX-distal Left Main (LM) with non-compliance balloon 2.5x15mm and 3.0x15mm.Stented Left Main - LCX with Drug Eluting Stent 3.0x20mm Intravascular Ultrasound assessment done.Post-dilated stent with non-compliance balloon 3.5x15mmExtended stent to ostial LM with Drug Eluting Stent 4.0x8mmPost-dilated LCX stent with non-compliance balloon 3.0x15mm
Post angioplasty assessment with intravascular ultrasound showed well apposed stent with no stent edge dissections.


PCI to Left Anterior Descending Artery (LAD):Guiding catheter EBU 3.5/7Fr, Coronary wire Runthrough to LCXAttempted to cross lesion with coronary wire Fielder XT & Fielder XT-A with Supercross Microcatheter Support. Unsuccessful and abandoned.
PCI to Left Circumflex Artery (LCX):Patient developed ventricular tachycardia/ventricular fibrillation while advancing balloon pass the left main coronary artery. Cardiopulmonary resuscitation performed and patient was mechanically ventilated. Transvenous temporary pacing catheter was inserted.
Pre-dilated ostial LCX-distal Left Main (LM) with non-compliance balloon 2.5x15mm and 3.0x15mm.Stented Left Main - LCX with Drug Eluting Stent 3.0x20mm Intravascular Ultrasound assessment done.Post-dilated stent with non-compliance balloon 3.5x15mmExtended stent to ostial LM with Drug Eluting Stent 4.0x8mmPost-dilated LCX stent with non-compliance balloon 3.0x15mm
Post angioplasty assessment with intravascular ultrasound showed well apposed stent with no stent edge dissections.


Case Summary
Coronary angioplasty in patient with advanced heart failure should be attempted with mechanical circulatory support device in the setting of ongoing ischemia. Intra-aortic balloon pump was chosen as it was the only option available in our center.
It was technically challenging to perform an upfront 2 stent LM bifurcation stenting in this patient due to unsuccessful wiring across the occluded LAD. Our bailout was to perform a LM-LCX provisional stenting in view of cardiac arrest.
On a hemodynamically stable patient, re-attempt angioplasty to both RCA and LAD CTO should be reconsidered. However, in this situation, PCI to LM-LCX was a life saving decision.
It was technically challenging to perform an upfront 2 stent LM bifurcation stenting in this patient due to unsuccessful wiring across the occluded LAD. Our bailout was to perform a LM-LCX provisional stenting in view of cardiac arrest.
On a hemodynamically stable patient, re-attempt angioplasty to both RCA and LAD CTO should be reconsidered. However, in this situation, PCI to LM-LCX was a life saving decision.


