Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-059
A Hard Decision and the Only Option : Provisional LM Stenting in Very Calcified Vessel
By Faten Aqilah Aris, Tjen Jhung Lee, Mohd Tawfeq Mohd Noor, Aizai Azan Rahim
Presenter
Faten Aqilah Aris
Authors
Faten Aqilah Aris1, Tjen Jhung Lee1, Mohd Tawfeq Mohd Noor1, Aizai Azan Rahim1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-059
CORONARY - Bifurcation/Left Main Diseases and Intervention
A Hard Decision and the Only Option : Provisional LM Stenting in Very Calcified Vessel
Faten Aqilah Aris1, Tjen Jhung Lee1, Mohd Tawfeq Mohd Noor1, Aizai Azan Rahim1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Mr LCS
Relevant Clinical History and Physical Exam
44 years old gentleman was referred from other cardiac center for multivessel high risk PCI. He had multiple risk factor including DM, Hypertension, Hyperlipidemia, and morbid obesity (BMI: 40) He has history of recurrent acute myocardial infarction. Coronary angiogram showed severe two vessel disease (calcified) with chronic total occlusion of RCA. Echocardiogram showed poor LV function with EF 38%. He was seen by multiple surgeon but was deemed very high risk in view of his comorbidities.
Relevant Test Results Prior to Catheterization
ECG: SR, IVCD
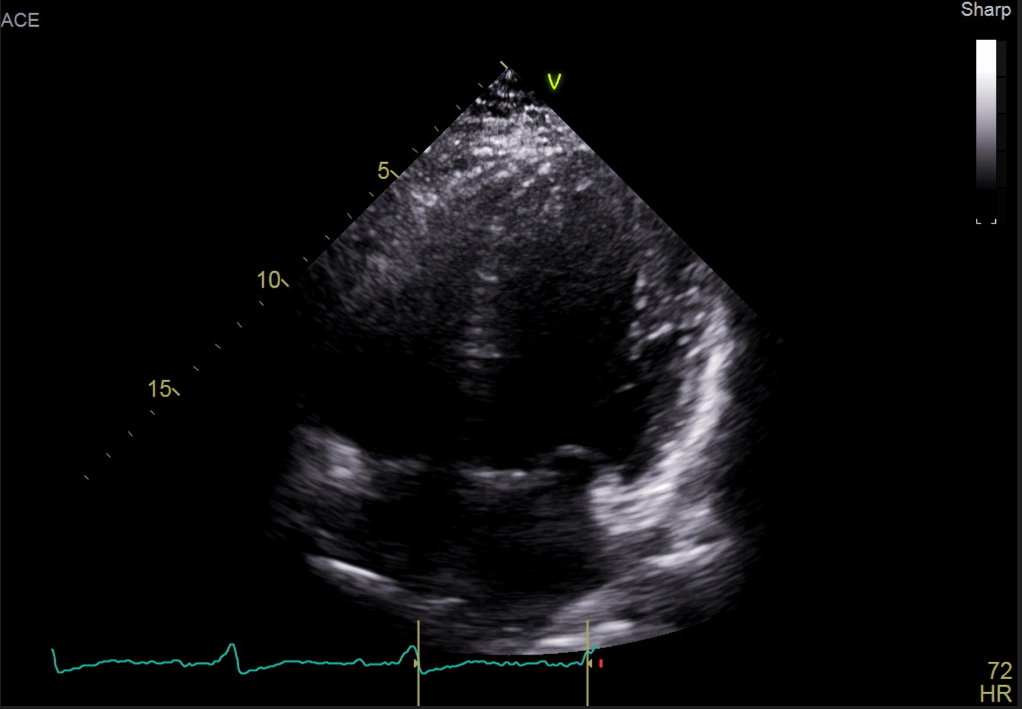
ECHO: EF 38%, global hypokinesia, TAPSE 2.6cm
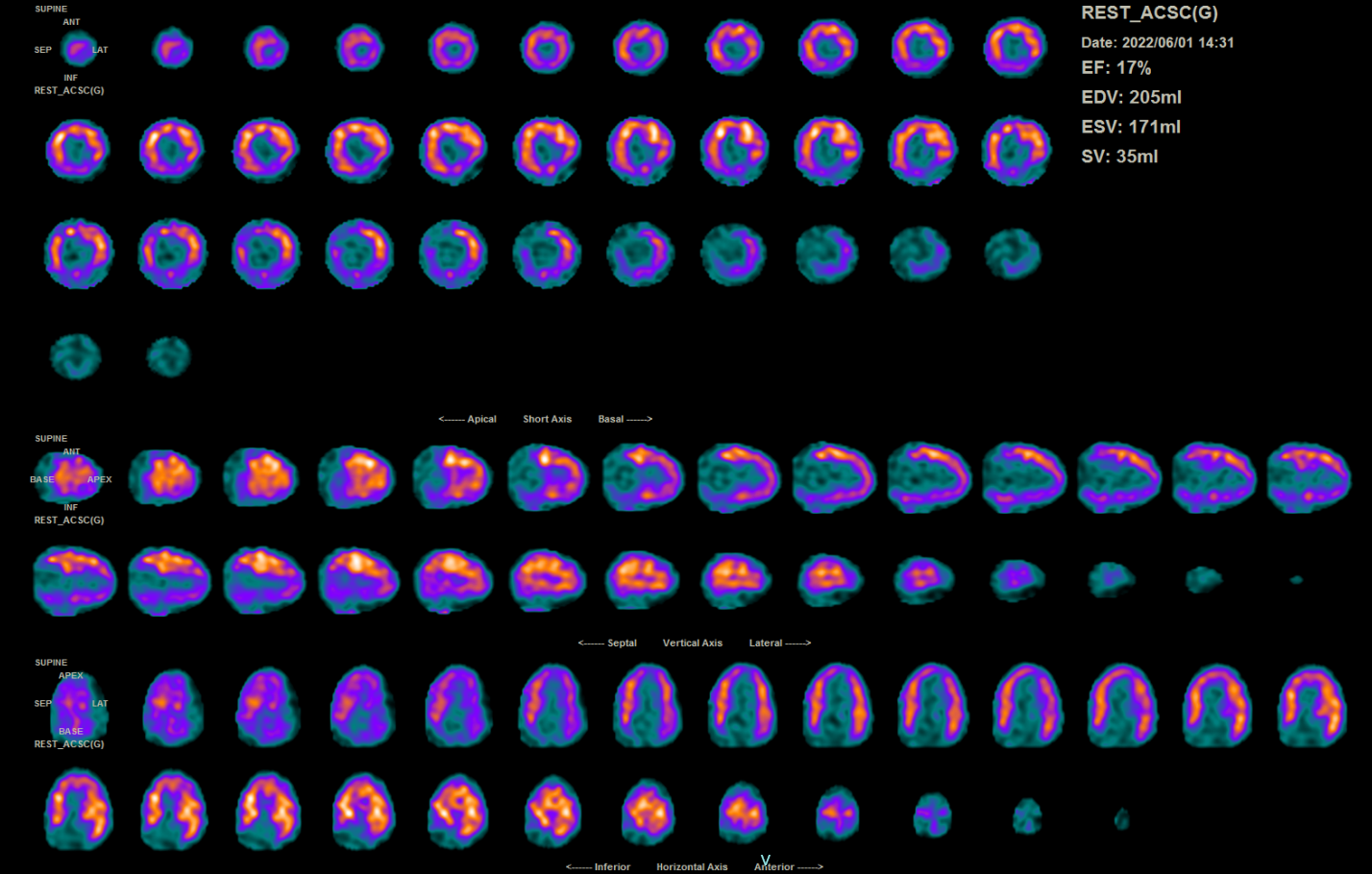
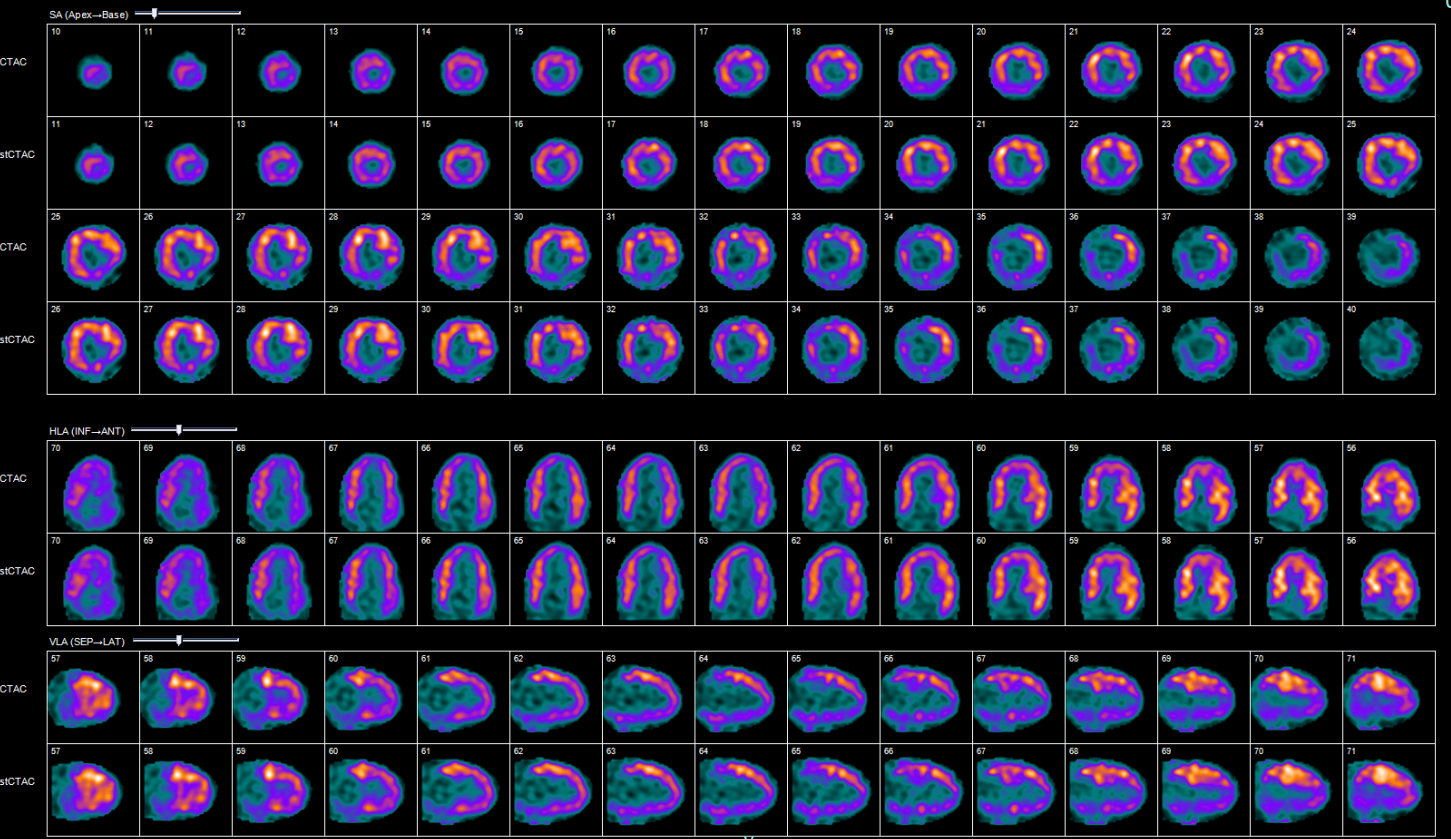
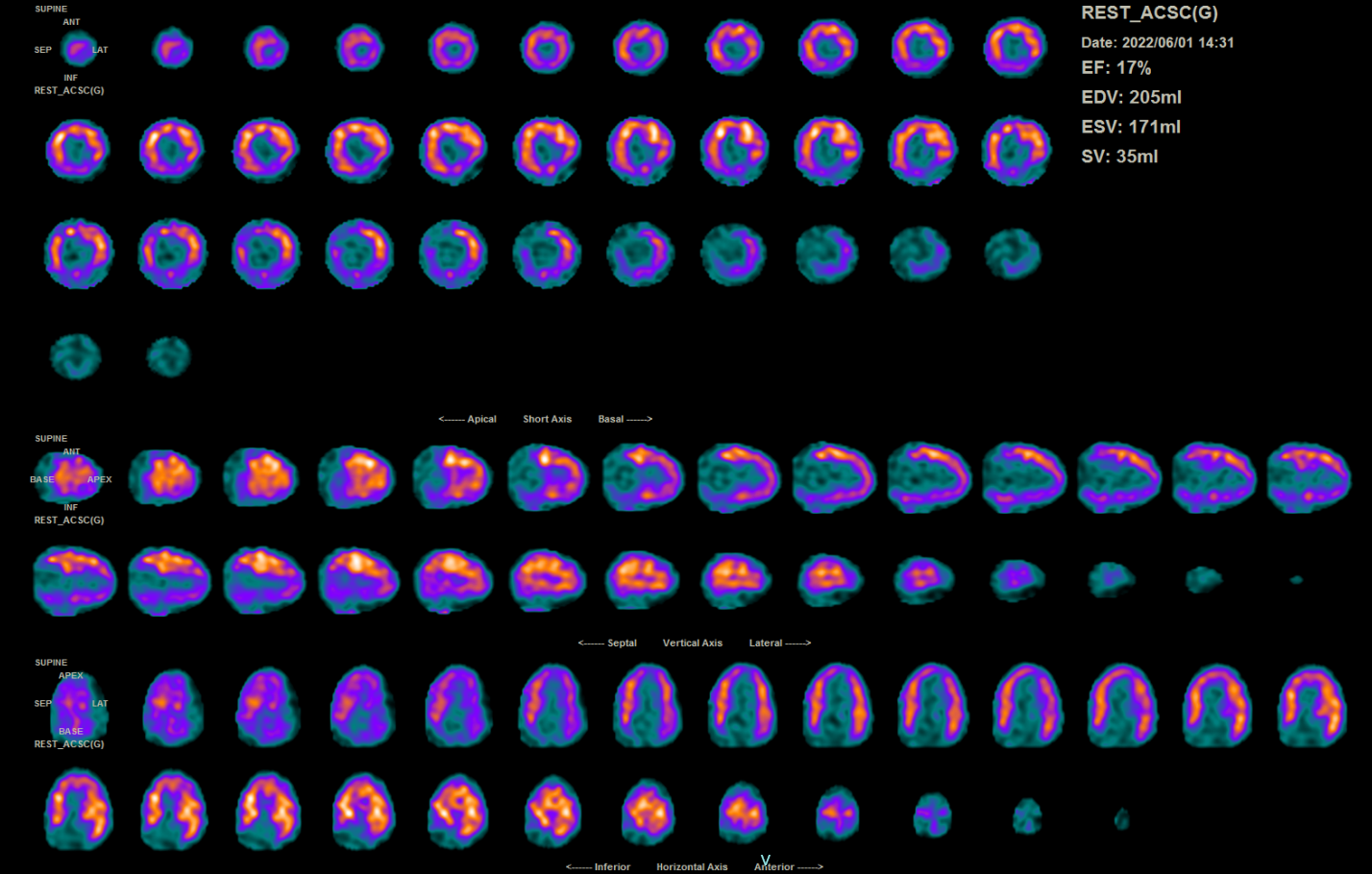
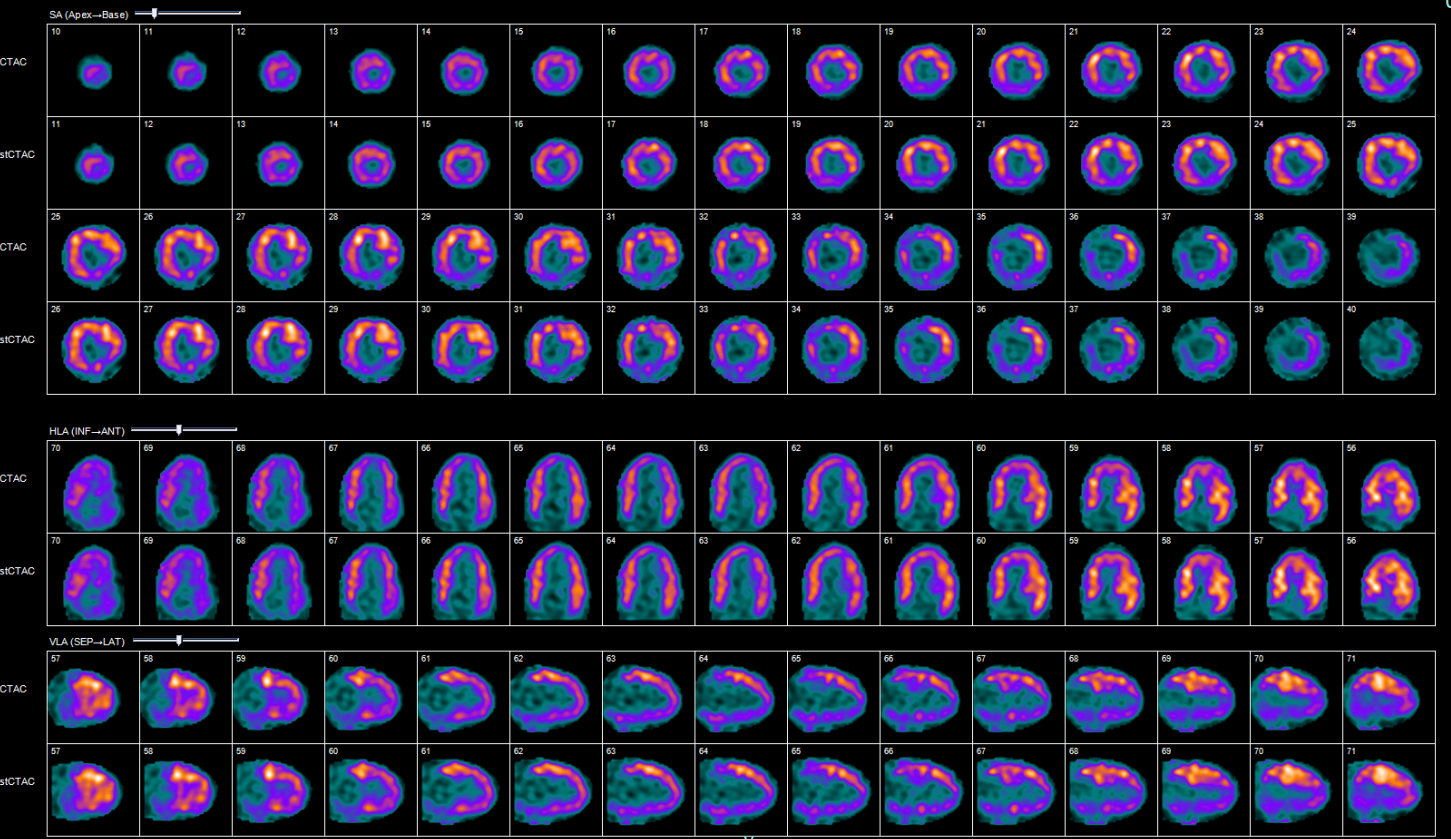
PET CT (for viability study) : large area of non transmural infarcted myocardium in the RCA territory. The rest of myocardium show normal viable myocardium
Blood investigations:-Hemoglobin : 14.3- Renal profile: Normal-HBA1c: 6.1%- LDL: 1.6
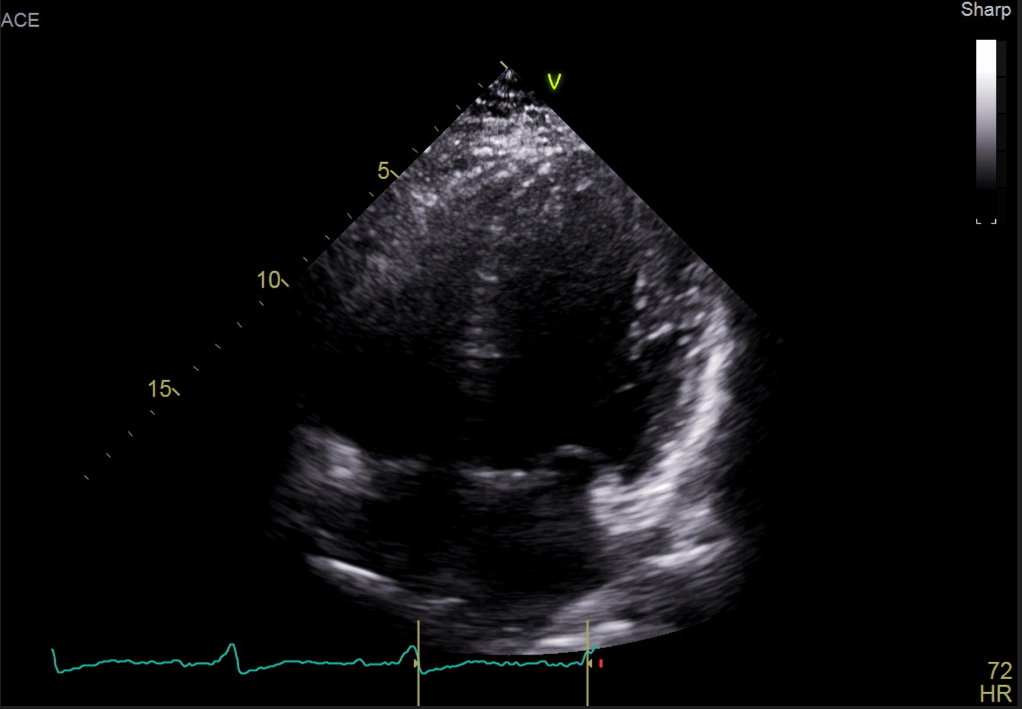
ECHO: EF 38%, global hypokinesia, TAPSE 2.6cm
PET CT (for viability study) : large area of non transmural infarcted myocardium in the RCA territory. The rest of myocardium show normal viable myocardium
Blood investigations:-Hemoglobin : 14.3- Renal profile: Normal-HBA1c: 6.1%- LDL: 1.6
Relevant Catheterization Findings
LMS: Normal
LAD: 80% ostial lesion, 90% mid LAD lesion, heavily calcified mid LAD
LCx: mild disease, ectatic vessel
RCA: severe proximal lesion 90%, CTO from after RV branch up till distal RPL/RPDA, collaterals via LCx/LAD seen
LAD: 80% ostial lesion, 90% mid LAD lesion, heavily calcified mid LAD
LCx: mild disease, ectatic vessel
RCA: severe proximal lesion 90%, CTO from after RV branch up till distal RPL/RPDA, collaterals via LCx/LAD seen
Interventional Management
Procedural Step
Patient was declined for CABG by surgeon as deemed very high risk. Attempted CTO RCA (J-CTO Score 4) Guiding SAL 1.0 6Fr but poor support thus change to AL 6fr Attempted to cross proximal cap : successful with GAIA 3rd, failed with Fielder XT and Gaia 2ndPOBA proximal RCA with scoreflex 3.0mm x15mm @ 12ATM Noted another calcified CTO mid RCA. Noted poor support despite adding Guide Plus II extension catheter Escalated to Conquest Pro 8gm but wire failed to cross the lesion despite support from AL 1.0, Guideplus II and finecross
Stage PCI to LMS-LAD with IVUS Right radial artery acessGuiding EBU 3.5 6Frwired LCx with Runthrough floppy and LAD with Sion BluePredilated mid LAD with Wedge NC 3.0mm x 15mm, balloon opened at 18ATMIVUS done: mid LAD vessel 3.5-4.0mm, calcified 270 degreeproximal LAD aneurysmal but not diseaseostial LAD severe disease with fibrofatty plaque, MLA 3.3mm2plaque burden at ostial LAD 93%
Further predilatation mid to ostial LAD 3.5mm x 15mm NC Balloon at 12-10ATMStented mid LAD (distal to aneurysmal) Onyx 3.5mm x 26mm Postdilated with 4.0x12mm NC Balloon at 16ATMStented proximal-ostial LAD to mid body LM with Megatron 4.0mmx 20mmPOT LM with 5.5mm x 8mm NC balloon @12-20ATMIVUS done: underexpanded ostial LAD stent and malopposed stent at body LMSFurther postdilatation done for LAD stent with NC baloon 3.5mm and 4.0mmRePOT LMS with 6mm x 8mm @ 20ATMRewired LCX and Kissing balloon inflation done at 12ATMFinal POT done with 6.0mm x 8mmFinal IVUS: good MSA, no dissection
Stage PCI to LMS-LAD with IVUS Right radial artery acessGuiding EBU 3.5 6Frwired LCx with Runthrough floppy and LAD with Sion BluePredilated mid LAD with Wedge NC 3.0mm x 15mm, balloon opened at 18ATMIVUS done: mid LAD vessel 3.5-4.0mm, calcified 270 degreeproximal LAD aneurysmal but not diseaseostial LAD severe disease with fibrofatty plaque, MLA 3.3mm2plaque burden at ostial LAD 93%
Further predilatation mid to ostial LAD 3.5mm x 15mm NC Balloon at 12-10ATMStented mid LAD (distal to aneurysmal) Onyx 3.5mm x 26mm Postdilated with 4.0x12mm NC Balloon at 16ATMStented proximal-ostial LAD to mid body LM with Megatron 4.0mmx 20mmPOT LM with 5.5mm x 8mm NC balloon @12-20ATMIVUS done: underexpanded ostial LAD stent and malopposed stent at body LMSFurther postdilatation done for LAD stent with NC baloon 3.5mm and 4.0mmRePOT LMS with 6mm x 8mm @ 20ATMRewired LCX and Kissing balloon inflation done at 12ATMFinal POT done with 6.0mm x 8mmFinal IVUS: good MSA, no dissection
Case Summary
This case illustrated a young gentleman with multiple comorbid and poor LV function, which suffered recurrent acute myocardial infarction but was not suitable for coronary artery bypass graft. Full revascularization were also unsuccessful and attempt to PCI to CTO RCA was failed. In view of that PCI to LM-LAD was done as that was his only option left.
His coronary artery were very calcified but plaque modification were successful with cutting balloon and not needing atherectomy. There is huge discrepancy in his vessel size between left main and left anterior descending but special stent (megatron) was used to overcome it.
Sometimes settling for less is the best option.
His coronary artery were very calcified but plaque modification were successful with cutting balloon and not needing atherectomy. There is huge discrepancy in his vessel size between left main and left anterior descending but special stent (megatron) was used to overcome it.
Sometimes settling for less is the best option.


