Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-162
Acute Vascular Compromise at the Distal Stent Edge Portion After PCI: What and How to Look for?
By Dong Oh Kang
Presenter
Dong Oh Kang
Authors
Dong Oh Kang1
Affiliation
Korea University Guro Hospital, Korea (Republic of)1,
View Study Report
TCTAP C-162
IMAGING AND PHYSIOLOGIC LESION ASSESSMENT - Imaging: Intravascular
Acute Vascular Compromise at the Distal Stent Edge Portion After PCI: What and How to Look for?
Dong Oh Kang1
Korea University Guro Hospital, Korea (Republic of)1,
Clinical Information
Patient initials or Identifier Number
KOS and PJS
Relevant Clinical History and Physical Exam
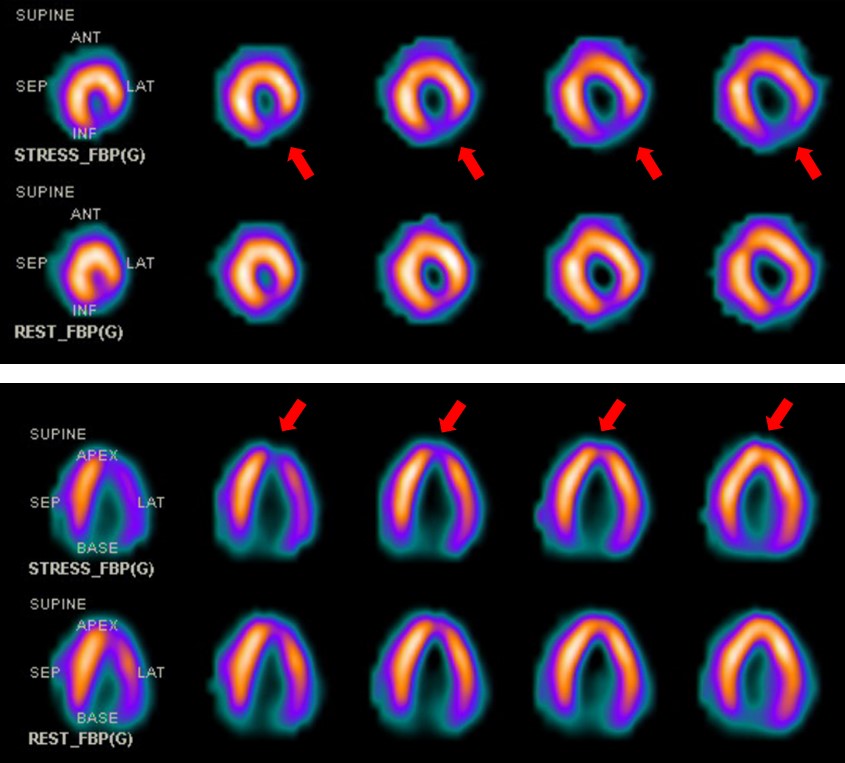
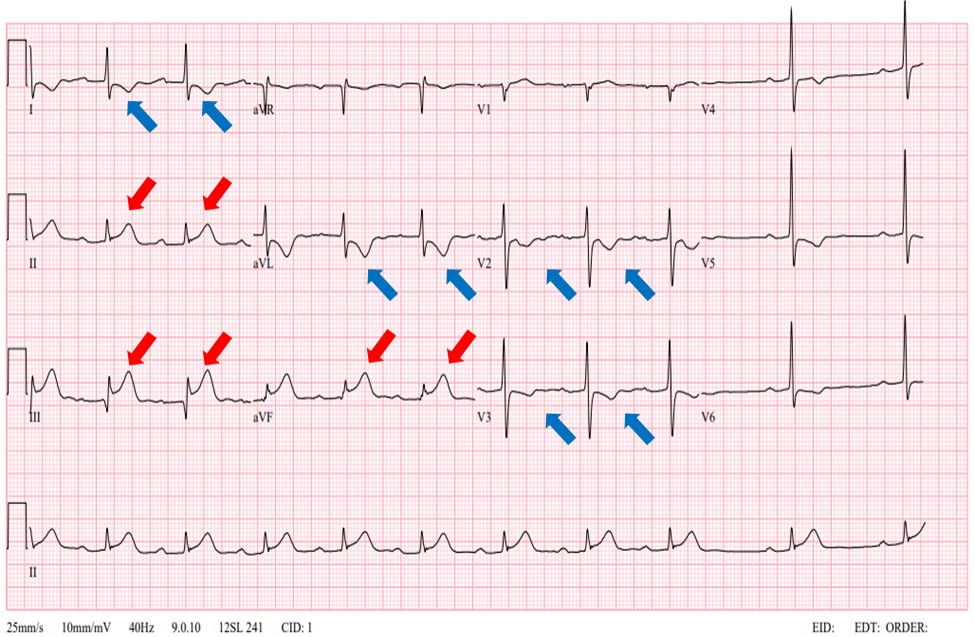
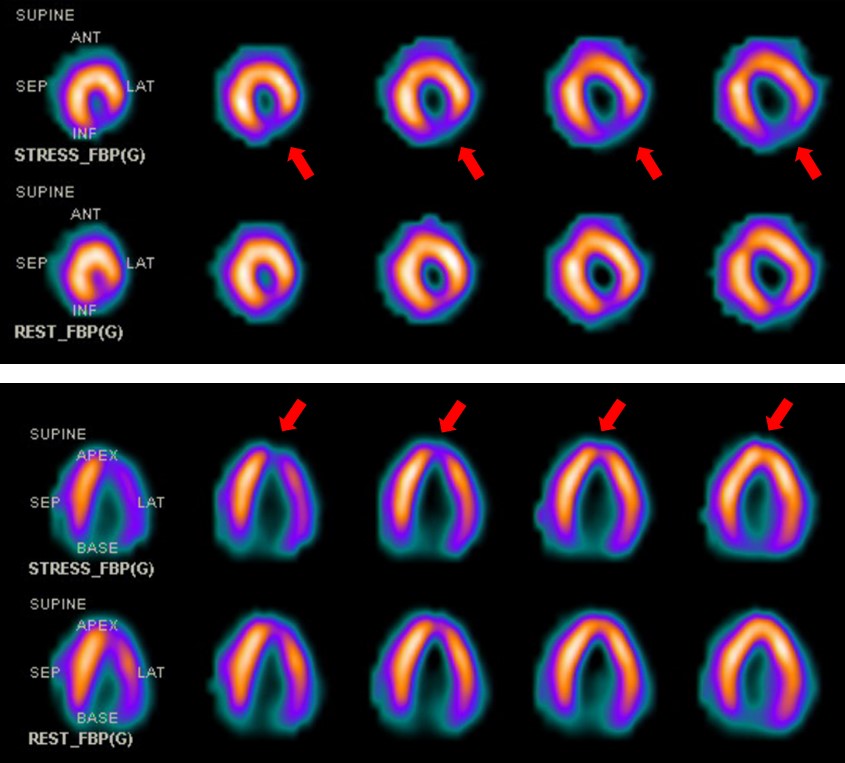
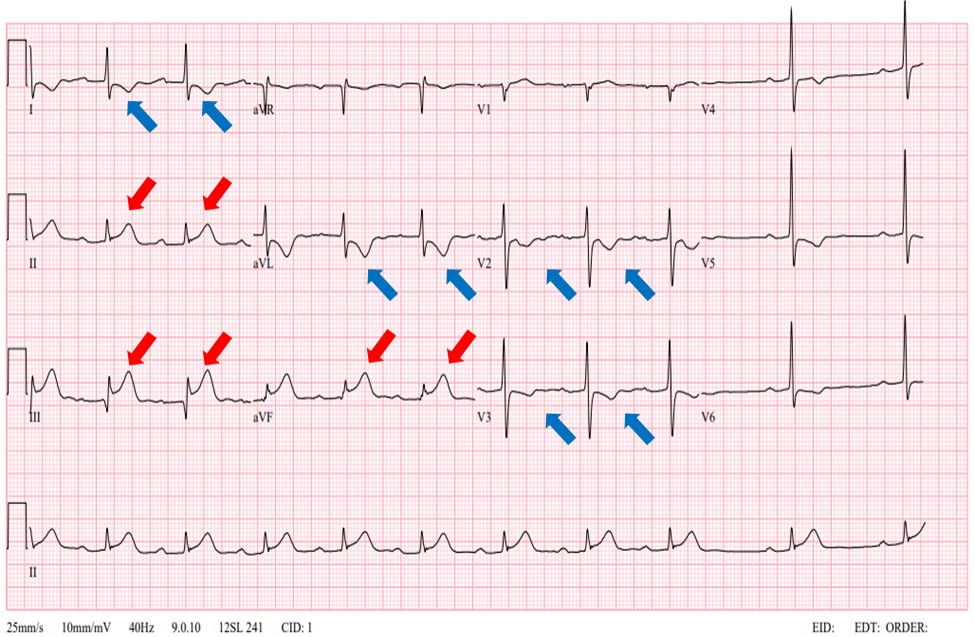
Case 1: A 79-year-old female with a history of hypertension was presented for effort chest discomfort since 3 months ago. The patient was recommended to undergo invasive coronary angiography based on typical angina symptom and positive stress test results (Figure 1).Case 2: A 64-year-old female patient with a history of dyslipidemia was presented for sudden chest pain since 1 hour ago. Initial electrocardiogram showed prominent ST-segment elevation at the inferior leads (Figure 2).
Relevant Test Results Prior to Catheterization
Relevant Catheterization Findings
Case 1: Baseline angiography showed severe diffuse stenosis (90%) with heavy calcification at mid LAD. Based on recurrent chest pain under medical therapy, we decided to undergo therapeutic intervention.Case 2: Emergency coronary angiography showed thrombotic subtotal occlusion (TIMI-1) at mid RCA, therefore, we decided to undergo primary PCI.
Interventional Management
Procedural Step
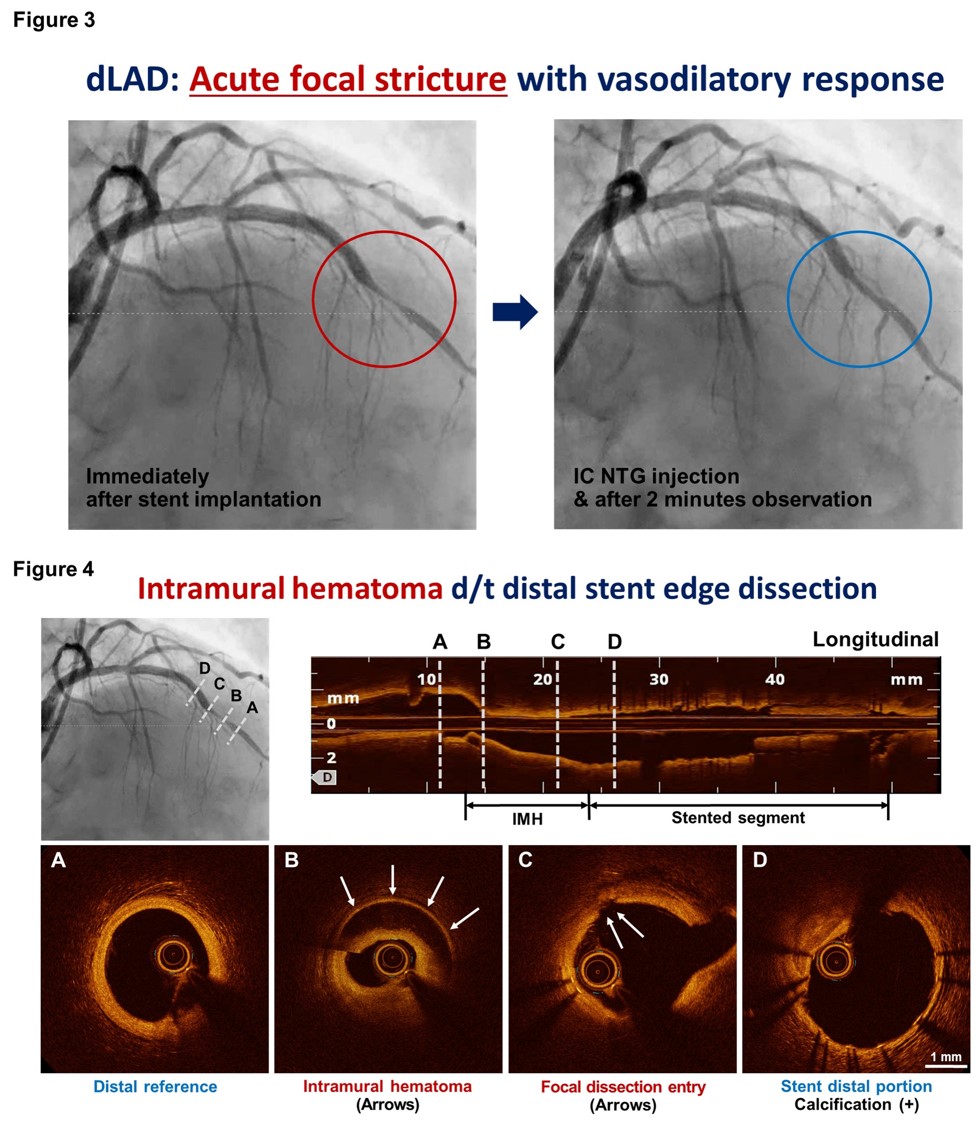
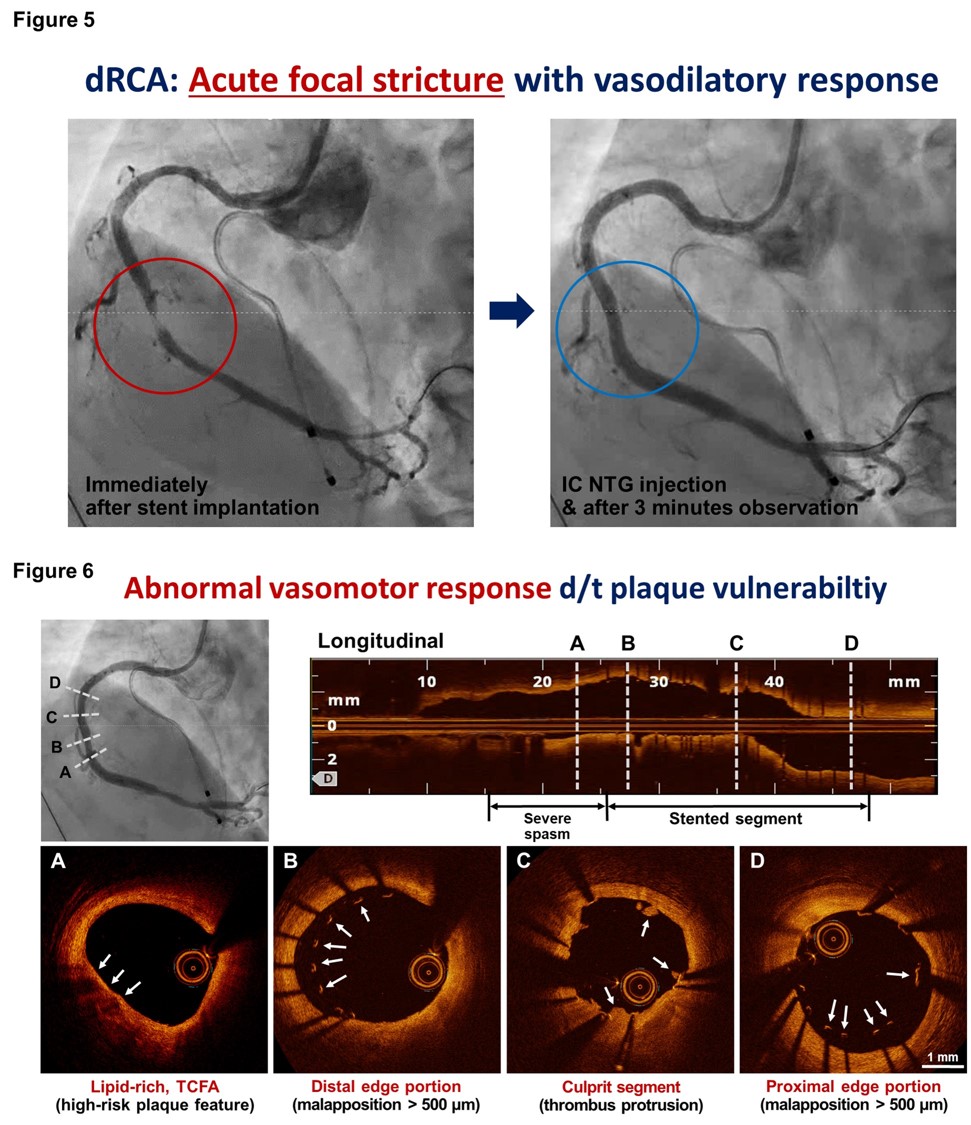
Case 1: 7Fr EBU3.5 catheter was engaged via right femoral access. Pre-dilation was performed using semi-compliant (2.0x15mm) and scoring (2.5x13mm) balloons. Sirolimus-eluting stent (SES) 3.0x30mm was implanted and post-dilation was performed using non-compliant balloon (3.5x8mm). Follow-up angiogram showed acute focal stricture at the distal stent edge and luminal narrowing was modestly resolved after intracoronary NTG injection (Figure 3). We performed OCT intravascular imaging to explore the underlying mechanism of this abnormal vasomotor response. Intracoronary imaging revealed prominent intramural hematoma originating from the distal stent edge portion (Figure 4).
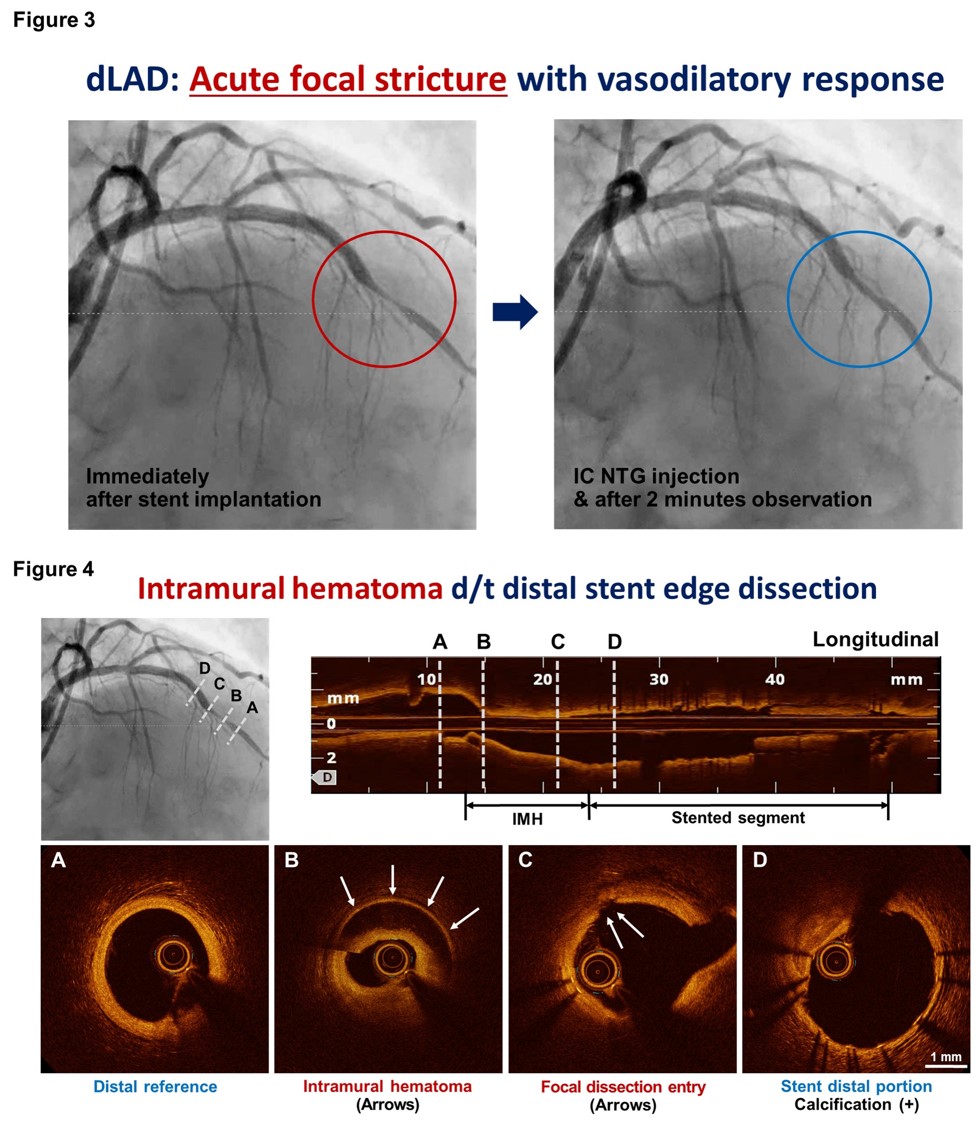
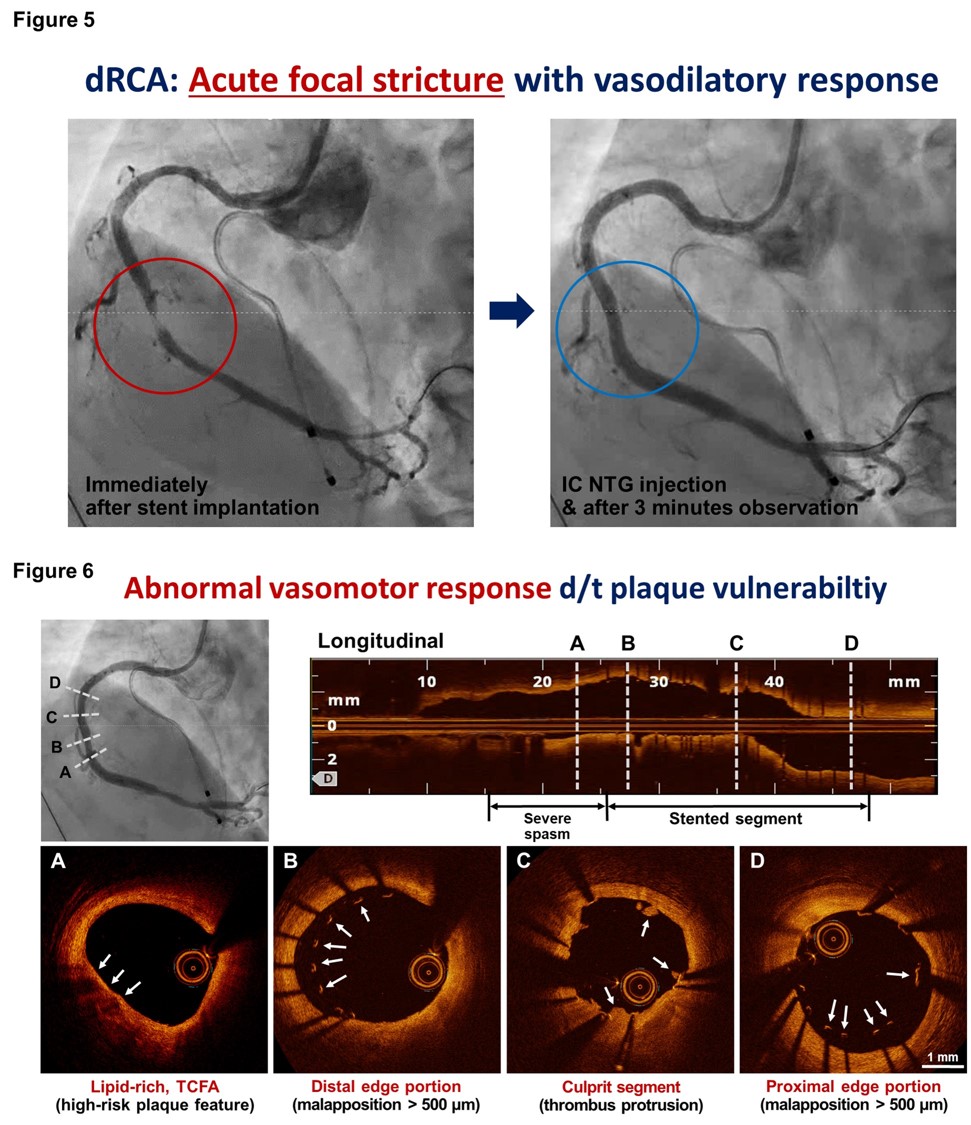
Case 2: 6Fr JR4 catheter was engaged via right radial access. Distal flow was restored (TIMI-3) after pre-dilation with semi-compliant balloon (2.0x15mm) and SES 3.0x25mm was successfully implanted. Follow-up angiogram showed acute focal stricture at the distal stent edge and this was gradually resolved after intracoronary NTG injection (Figure 5). OCT intravascular imaging was performed to explore the underlying mechanism of this abnormal vasomotor response. Intracoronary imaging showed no significant evidence of adverse findings. Despite baseline angiogram showed normal-looking appearance of the distal stent landing zone, intravascular imaging revealed widely distributed lipid-rich thin-cap fibroatheroma at this portion (Figure 6).
Case 2: 6Fr JR4 catheter was engaged via right radial access. Distal flow was restored (TIMI-3) after pre-dilation with semi-compliant balloon (2.0x15mm) and SES 3.0x25mm was successfully implanted. Follow-up angiogram showed acute focal stricture at the distal stent edge and this was gradually resolved after intracoronary NTG injection (Figure 5). OCT intravascular imaging was performed to explore the underlying mechanism of this abnormal vasomotor response. Intracoronary imaging showed no significant evidence of adverse findings. Despite baseline angiogram showed normal-looking appearance of the distal stent landing zone, intravascular imaging revealed widely distributed lipid-rich thin-cap fibroatheroma at this portion (Figure 6).
Case Summary
Case 1: Despite focal intimal entry point, distal stent edge dissection was suspected to be the main mechanism of intramural hematoma formation. Additional SES 2.75x22mm was implanted to manage the adverse findings and follow-up OCT imaging confirmed stent optimization with well covered distal edge dissection and intramural hematoma. Final angiogram also corroborated the intravascular imaging results.Case 2: Acute endothelial dysfunction occurring at the site of plaque vulnerability was suggested as the main mechanism of acute vascular compromise. Based on intravascular imaging, the patient underwent conservative medical management with vasodilators and high-intensity statins.


