Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-060
The Story of Calcified Bifurcation Lesion, Drug Coated Balloon and Rotational Atherectomy
By Heng Shee Kim, Shinji Imura, Motosu Ando, Miwako Tsukiji, Yasuhiro Tarutani, Yuuki Nakanishi, Fumitaka Hosaka
Presenter
Heng Shee Kim
Authors
Heng Shee Kim1, Shinji Imura2, Motosu Ando2, Miwako Tsukiji2, Yasuhiro Tarutani3, Yuuki Nakanishi2, Fumitaka Hosaka2
Affiliation
Sultanah Aminah Hospital, Malaysia1, Okamura Memorial Hospital, Japan2, Mishima Tarutani Clinic, Japan3,
View Study Report
TCTAP C-060
CORONARY - Bifurcation/Left Main Diseases and Intervention
The Story of Calcified Bifurcation Lesion, Drug Coated Balloon and Rotational Atherectomy
Heng Shee Kim1, Shinji Imura2, Motosu Ando2, Miwako Tsukiji2, Yasuhiro Tarutani3, Yuuki Nakanishi2, Fumitaka Hosaka2
Sultanah Aminah Hospital, Malaysia1, Okamura Memorial Hospital, Japan2, Mishima Tarutani Clinic, Japan3,
Clinical Information
Patient initials or Identifier Number
SYZN
Relevant Clinical History and Physical Exam
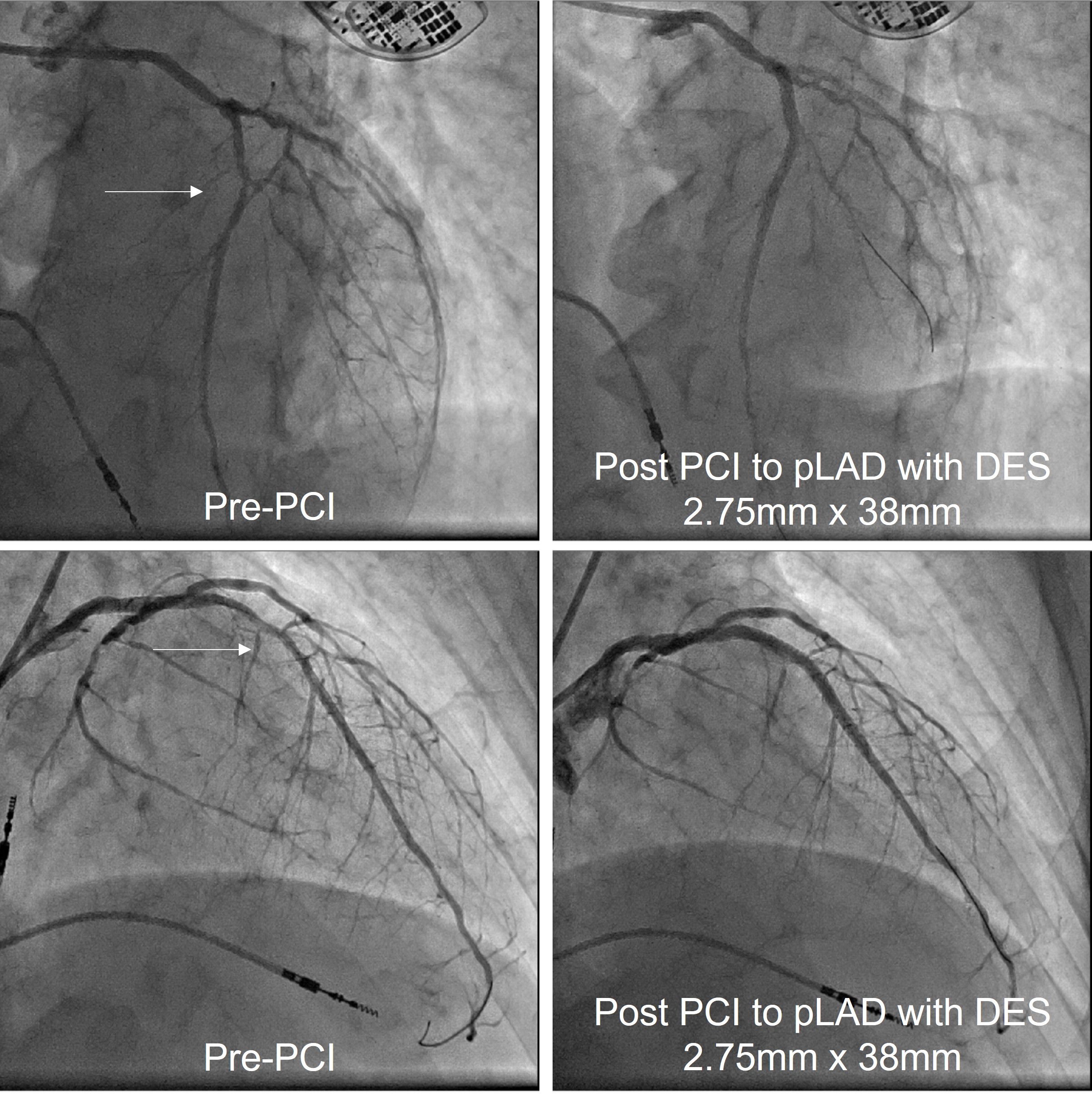
He is a 77-year-old smoker with type 2 diabetes, hypertension, dyslipidemia, and complete atrioventricular block on a dual chamber pacemaker. He first presented in 2016 with typical angina, and subsequent CAG revealed triple vessel disease with distal PDA disease. As the FFR of LCx and RCA was insignificant, he underwent PCI to LAD. A follow-up CAG in 2017 revealed no evidence of disease progression. He was well till 2022 when he had CCS II angina.
Physical examination was unremarkable.
Physical examination was unremarkable.
Relevant Test Results Prior to Catheterization
The ECG revealed no signs of ischemia. The echocardiographywas normal, with a left ventricular ejection fraction of 53% and no regionalwall motion abnormalities. His LDL was 48 mg/dl, and his eGFR was 61 ml/min,but he had poorly controlled diabetes mellitus, with a HbA1c of 7. 6. Because of his previous IHD history, he wasadvised to undergo repeat coronary angiography.
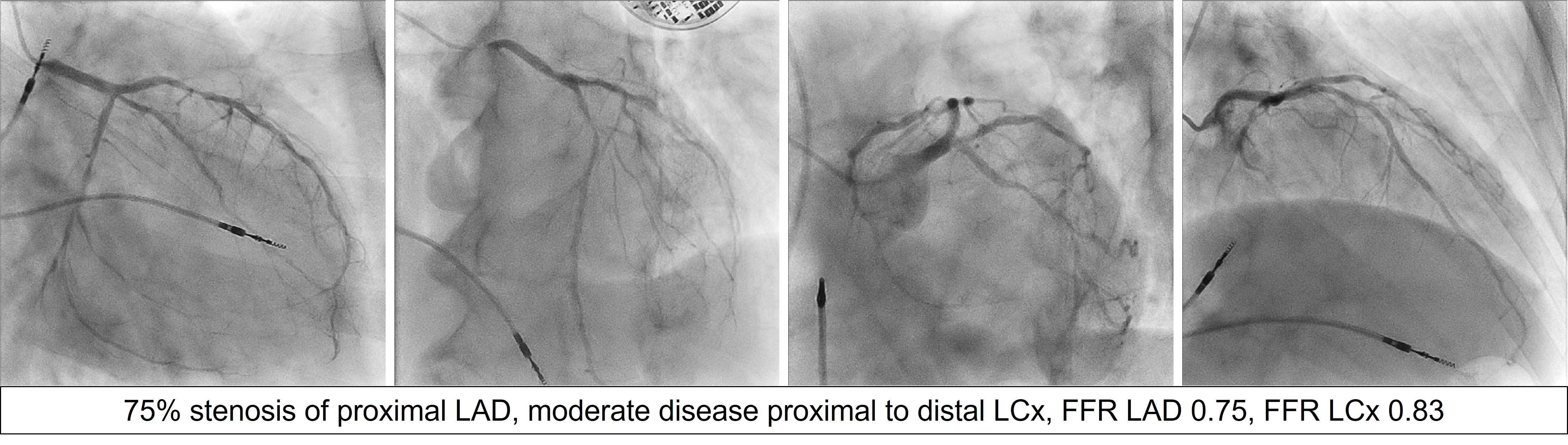
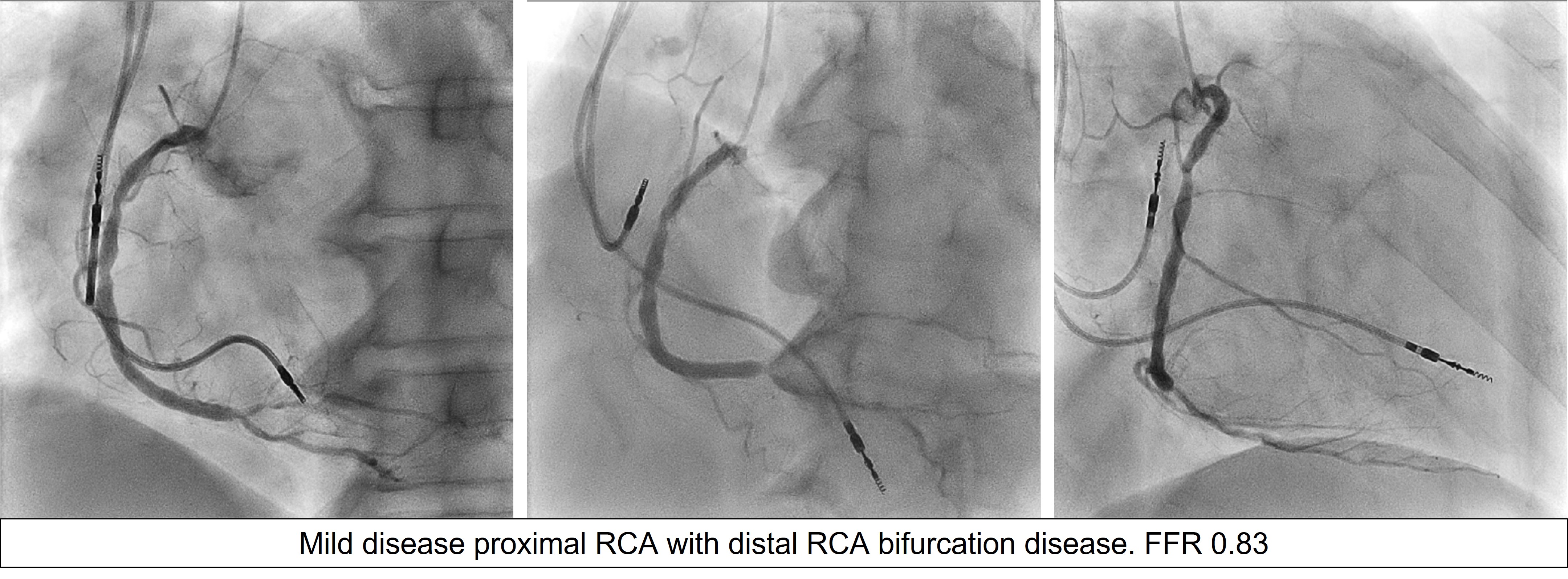
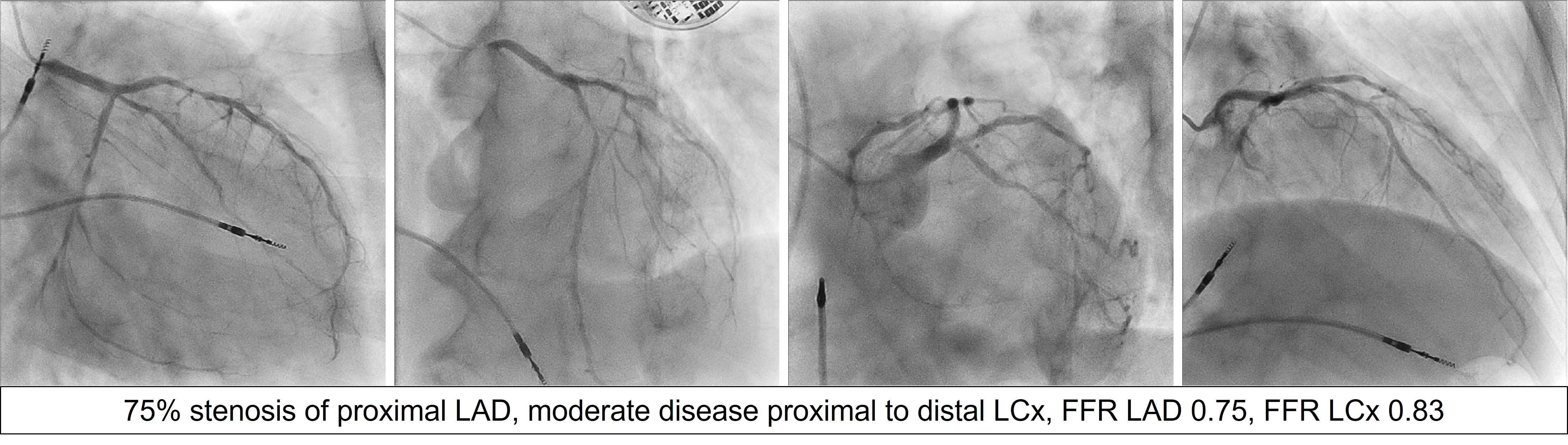
Relevant Catheterization Findings
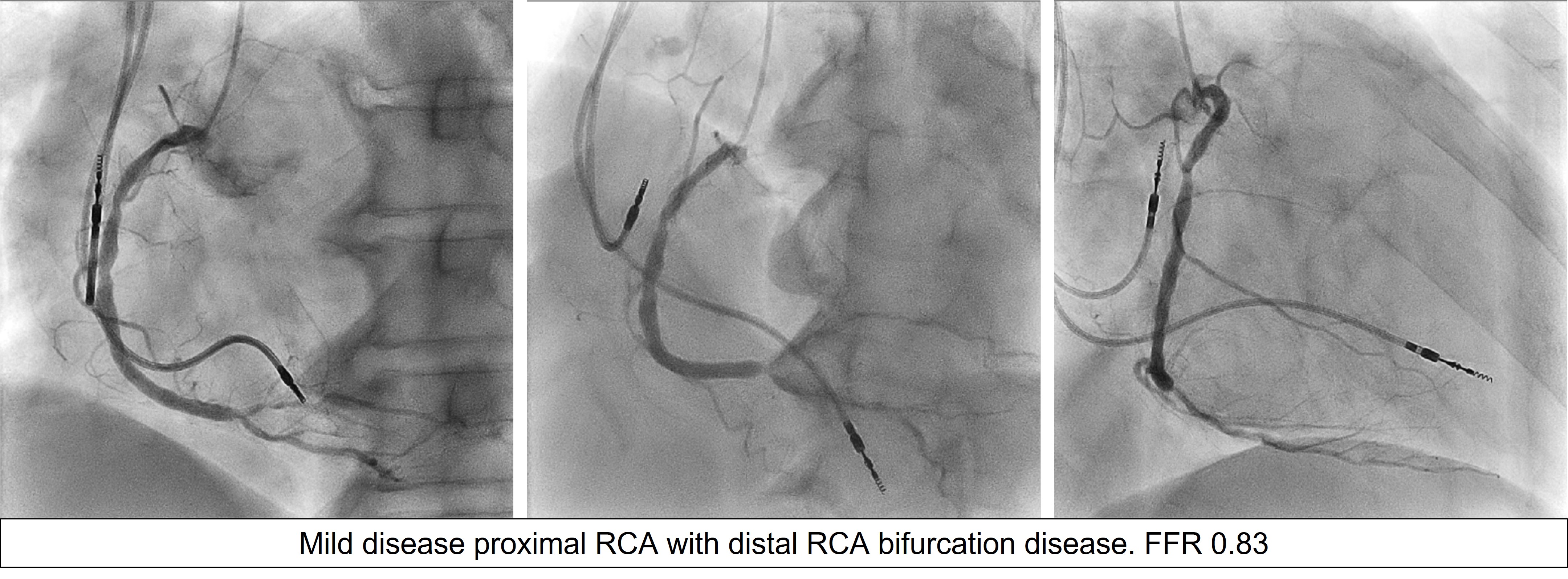
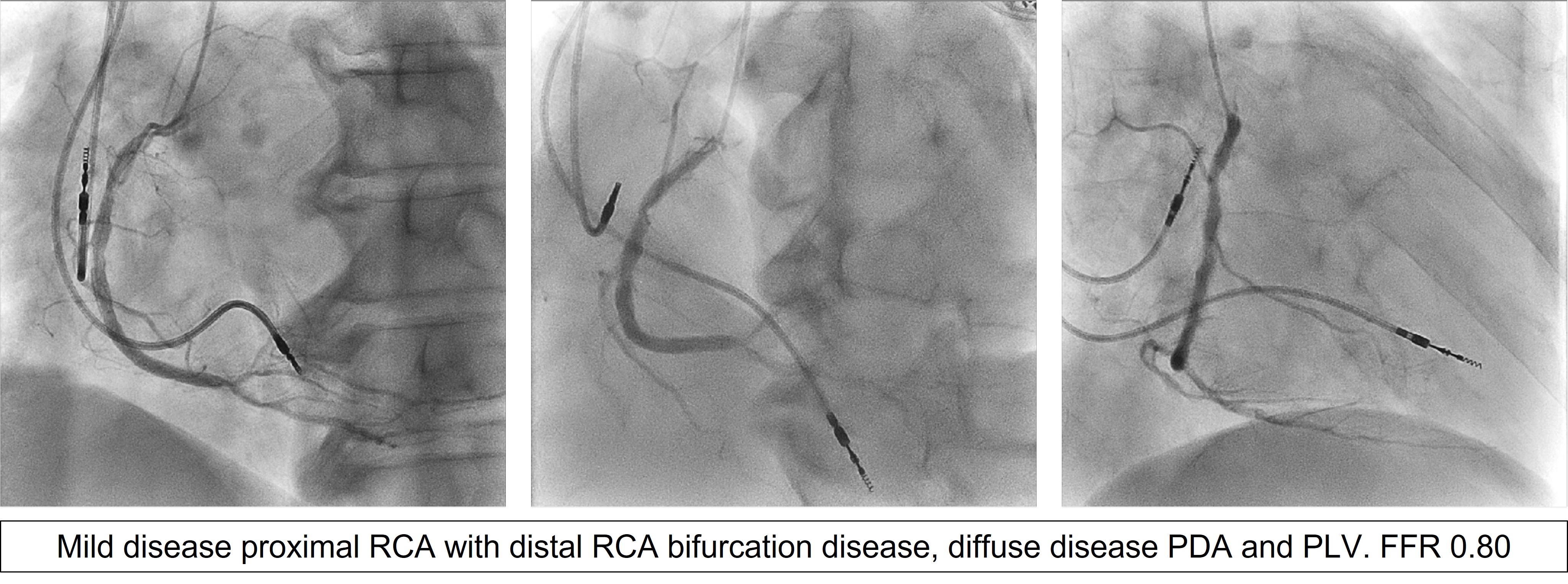
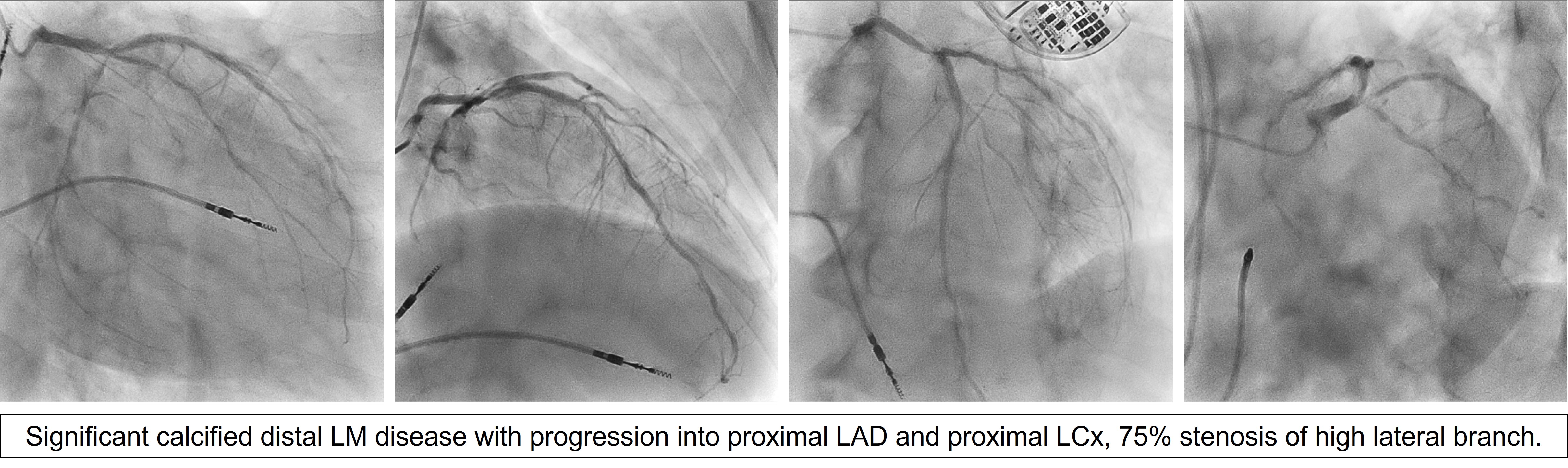
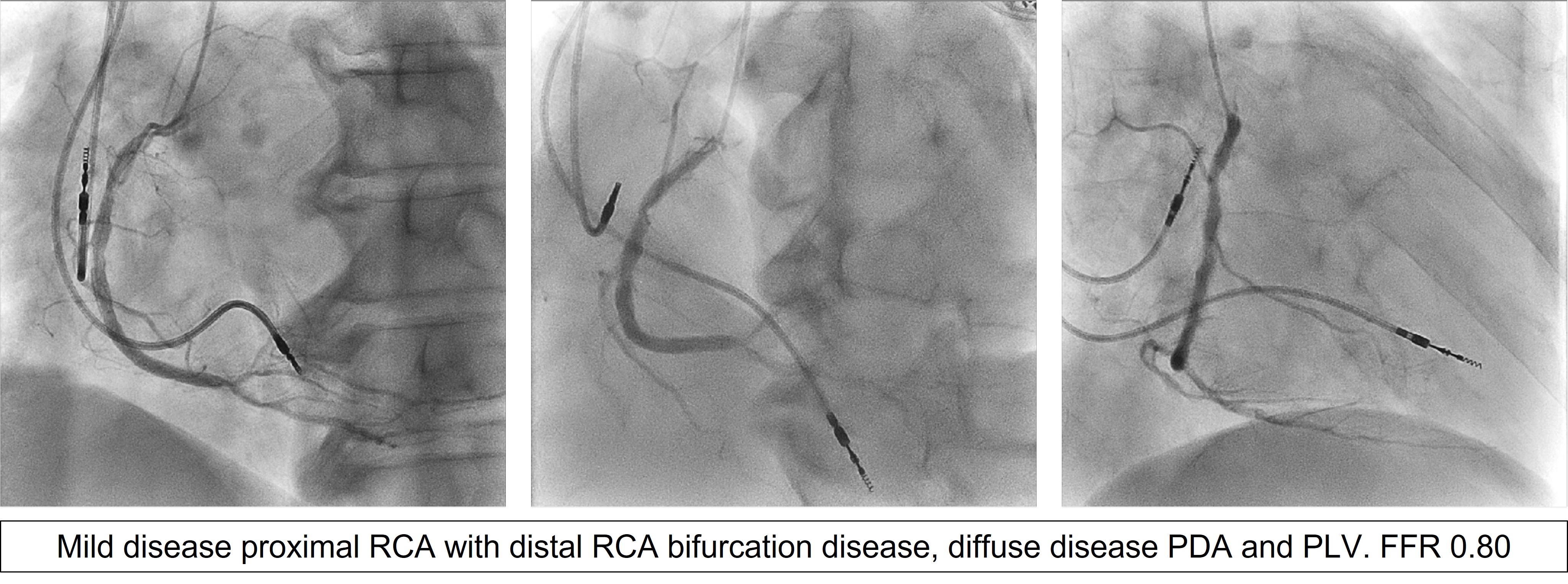
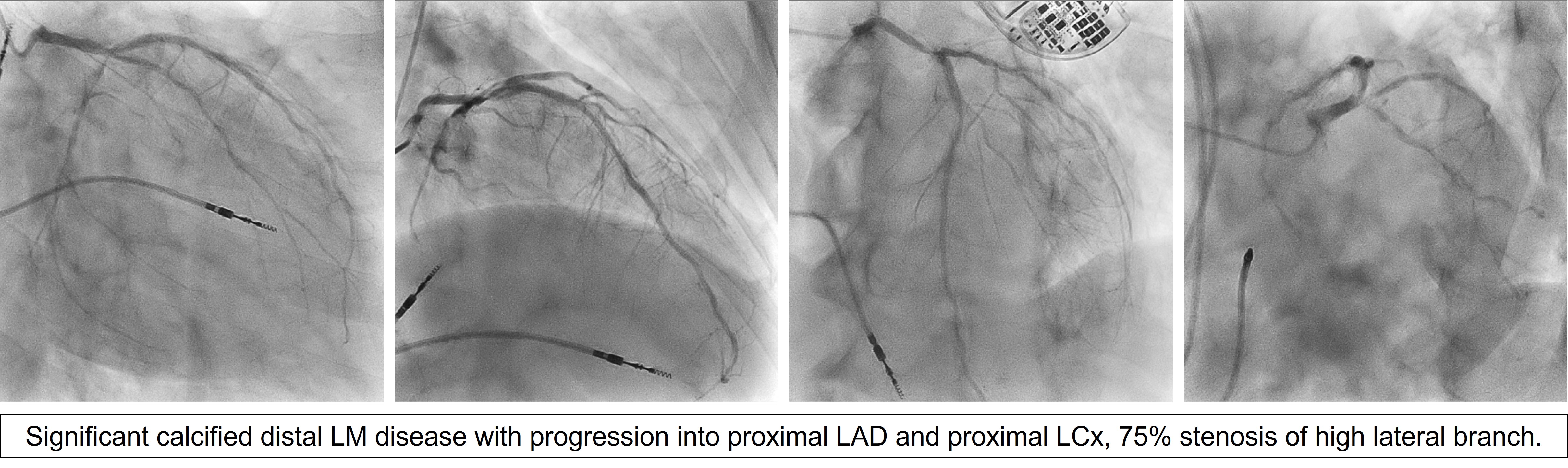
CAG revealed 75% dLM, 75% pLAD, 50% mLAD ISR; 75% pLCx, 75% mLCx, and 75% stenosis in the high lateral branch. The FFR to LAD was 0.7, and 0.8 for RCA. It is a Medina 1,1,1 true bifurcation lesion with LM involvement. The Syntax I score was 46, Syntax II score suggests either PCI/ CABG. After discussion with the patient and family members, he opted for PCI. Because RCA was FFR insignificant with stable disease, we decided to perform PCI to the left main, LAD, LCx, and high lateral branch.
Interventional Management
Procedural Step
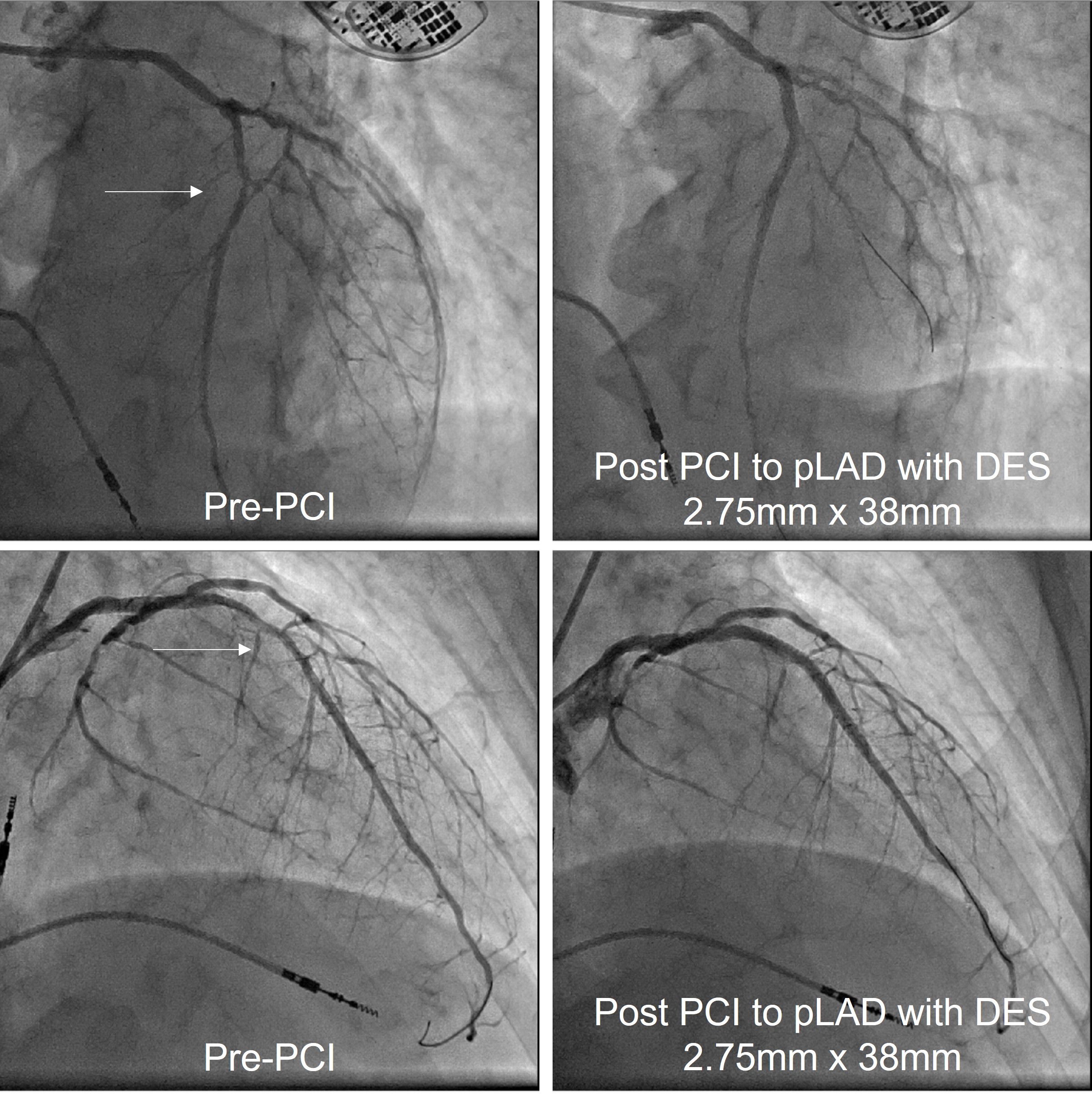
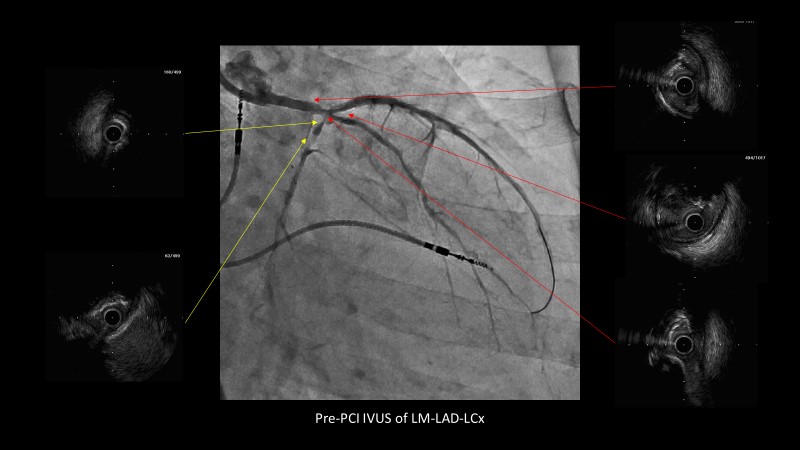
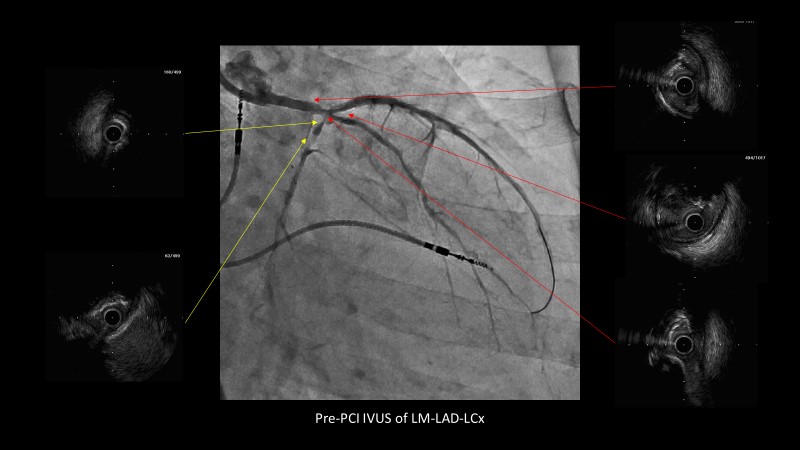
The case started with an 8F RFA approach and engaged with a Roadmaster 8Fr, CLS40 SH. LAD and LCx wired with 2 ASAHI SION Blue wires. IVUS showed 270° calcified plaque of dLM to ostial LAD and circumferential calcified plaque of pLCx. We considered bifurcation DCB only strategy after calcium debulking due to his high-risk profile. Rotablation was performed with ROTAPRO 2.0mm burr at maximum speed for 4 cycles from dLM to pLAD followed by Rotablation from dLM to pLCx with ROTAPRO 1.5 mm burr at maximum speed for 9 rounds. Post-Rotablation showed good debulking results but with Type A non-flow limiting dissection of the LCx.
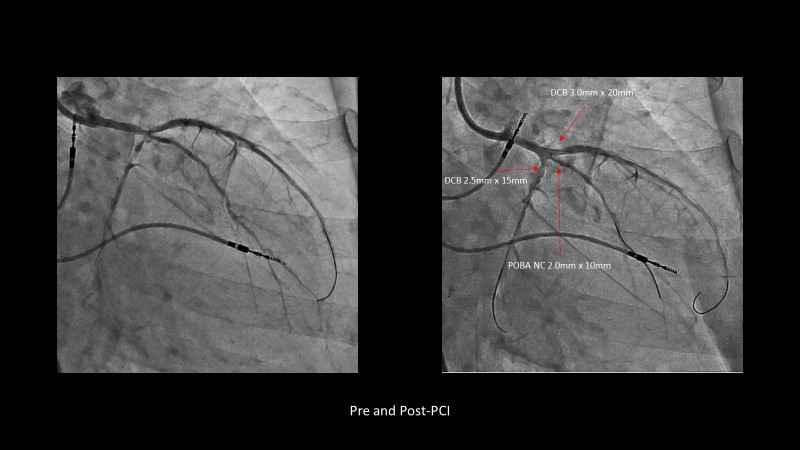
We then further prepared the bifurcation lesion with balloon dilatation As Wolverine 2.5 x 10 balloon failed to cross LCx despite anchoring balloon, LCx POBA with SC 2.0 x 10 mm, followed by Wolverine 2.5 x 10 mm balloon. Thereafter predilatation of pLAD to dLM with Wolverine 3.0 x 15 mm balloon. Next was KBT to LM-LAD-LCx with the Wolverine 3.0 x 15 mm and 2.5 x 10mm balloons. HL branch POBA with NC 2.0 x 10 mm balloon. After lesion preparation, as the residual stenosis < 30% with non-flow limiting dissection, we decided to perform bifurcation DCB.
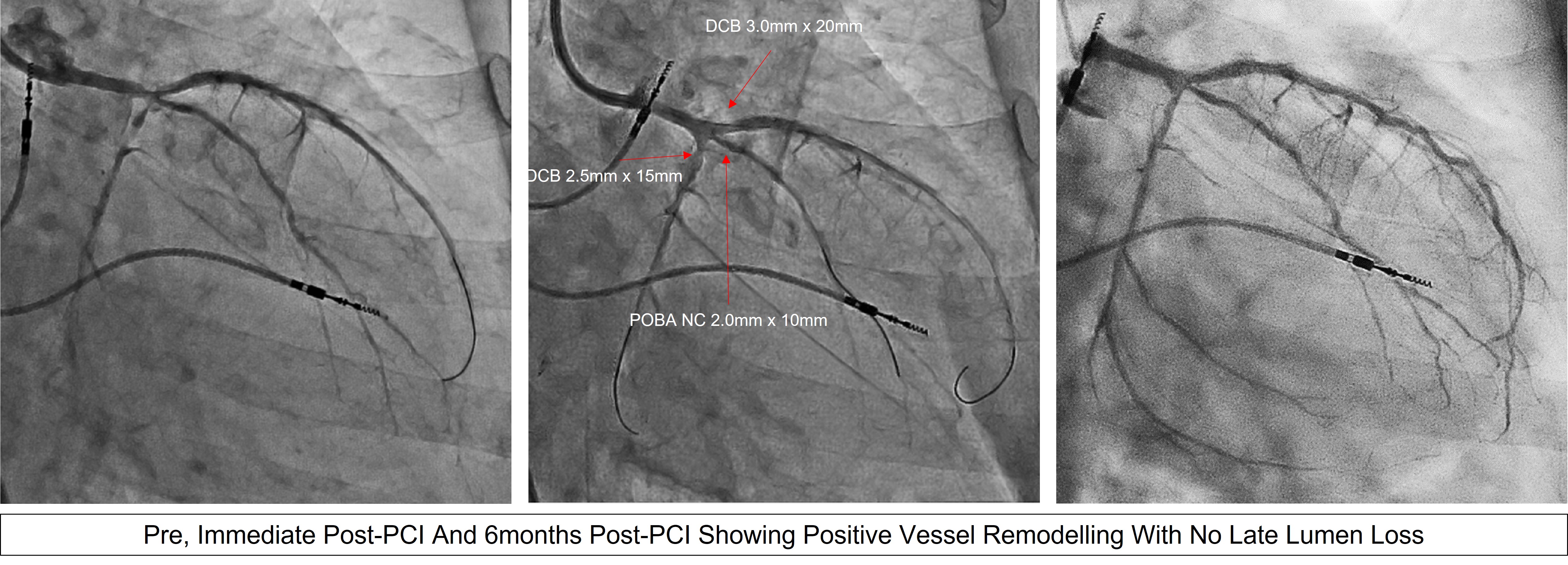
LM-LCx treated with DCB Sequent Please Neo 2.5 x 15mm and LM-LADwith DCB Sequent Please Neo 3.0 x 20mm. This was followed by KBT of the bifurcation with the DCB balloon. Total procedure time: 170min, total contrast:80ml. Repeated CAG 6 months later showed positive remodeling with no late lumen loss.
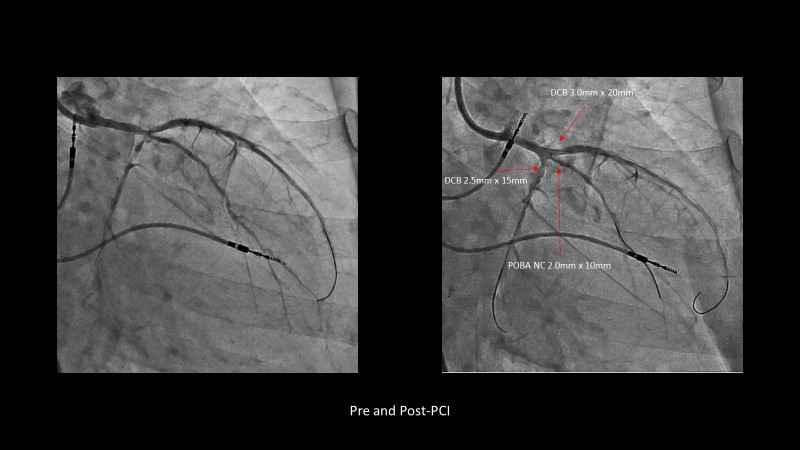
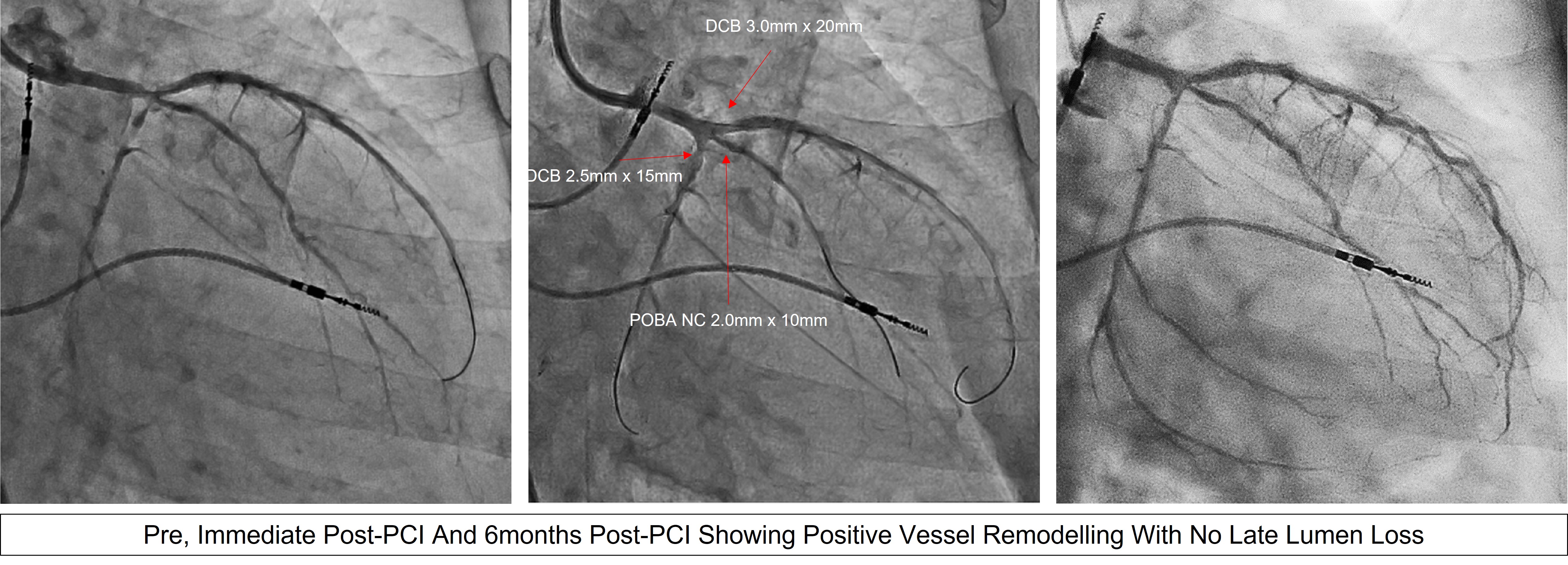
We then further prepared the bifurcation lesion with balloon dilatation As Wolverine 2.5 x 10 balloon failed to cross LCx despite anchoring balloon, LCx POBA with SC 2.0 x 10 mm, followed by Wolverine 2.5 x 10 mm balloon. Thereafter predilatation of pLAD to dLM with Wolverine 3.0 x 15 mm balloon. Next was KBT to LM-LAD-LCx with the Wolverine 3.0 x 15 mm and 2.5 x 10mm balloons. HL branch POBA with NC 2.0 x 10 mm balloon. After lesion preparation, as the residual stenosis < 30% with non-flow limiting dissection, we decided to perform bifurcation DCB.
LM-LCx treated with DCB Sequent Please Neo 2.5 x 15mm and LM-LADwith DCB Sequent Please Neo 3.0 x 20mm. This was followed by KBT of the bifurcation with the DCB balloon. Total procedure time: 170min, total contrast:80ml. Repeated CAG 6 months later showed positive remodeling with no late lumen loss.
Case Summary
Despite advances in technique and equipment, calcified bifurcation lesions have always been an Achilles tendon in complex PCI.
As the concept of leaving nothing behind, DCB has gained popularity in bifurcation PCI. However, since it primarily relies on drug transfer and tissue retention of the anti-proliferative drug, calcified lesions can dilute and impede the above processes, hence the benefit of DCB.
Our case demonstrated the proper procedures for calcium modification with RA and cutting balloons. This rationalizes the adoption of the RA/DCB approach. Thus, it promotes positive vessel remodeling without late lumen loss.
In conclusion, RA/DCB may be an appealing option for the right patient.
As the concept of leaving nothing behind, DCB has gained popularity in bifurcation PCI. However, since it primarily relies on drug transfer and tissue retention of the anti-proliferative drug, calcified lesions can dilute and impede the above processes, hence the benefit of DCB.
Our case demonstrated the proper procedures for calcium modification with RA and cutting balloons. This rationalizes the adoption of the RA/DCB approach. Thus, it promotes positive vessel remodeling without late lumen loss.
In conclusion, RA/DCB may be an appealing option for the right patient.


