Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-061
Challenges of Short Left Main With Ostial Left Anterior Descending Artery Lesion Intervention
By Aaron Hean Jin Ong, Imran Zainal Abidin
Presenter
Aaron Hean Jin Ong
Authors
Aaron Hean Jin Ong1, Imran Zainal Abidin2
Affiliation
Hospital Sultan Idris Shah, Malaysia1, University Malaya Medical Centre, Malaysia2,
View Study Report
TCTAP C-061
CORONARY - Bifurcation/Left Main Diseases and Intervention
Challenges of Short Left Main With Ostial Left Anterior Descending Artery Lesion Intervention
Aaron Hean Jin Ong1, Imran Zainal Abidin2
Hospital Sultan Idris Shah, Malaysia1, University Malaya Medical Centre, Malaysia2,
Clinical Information
Patient initials or Identifier Number
CLH
Relevant Clinical History and Physical Exam
A 68-year-old female with hypertension, non-valvular paroxysmal atrial fibrillation and breast cancer post mastectomy had presented with multiple episodes of resting angina and dyspnoea. She had no heart failure symptoms and was hemodynamically stable. Physical examination was unremarkable. She was promptly diagnosed with unstable angina and proceeded for inpatient coronary angiography.
Relevant Test Results Prior to Catheterization
Haemoglobin level was low at 10.6 g/dl
Relevant Catheterization Findings
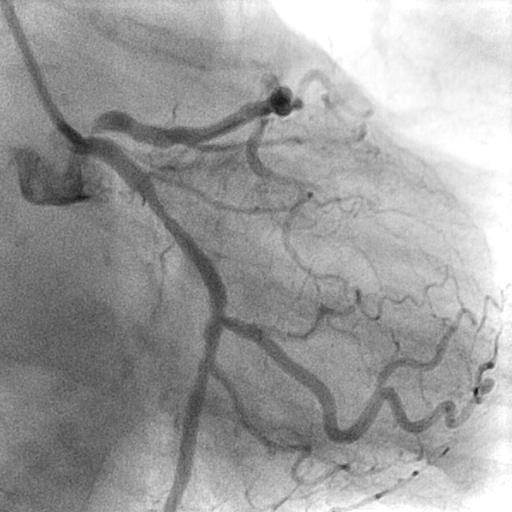
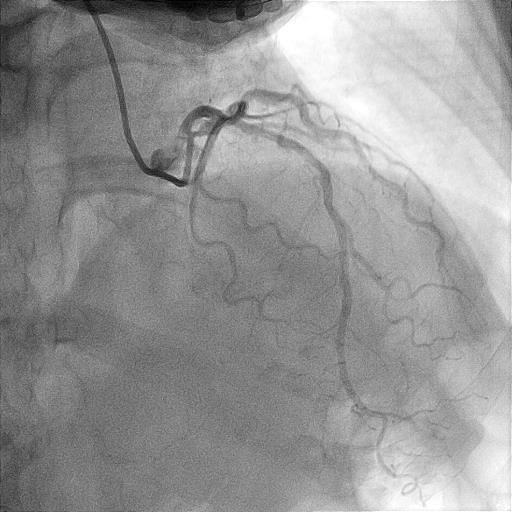
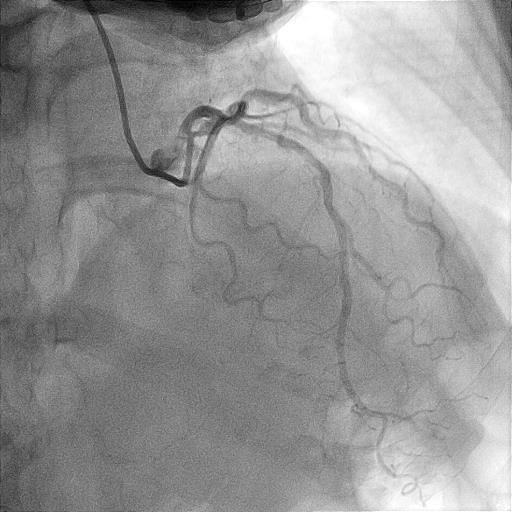
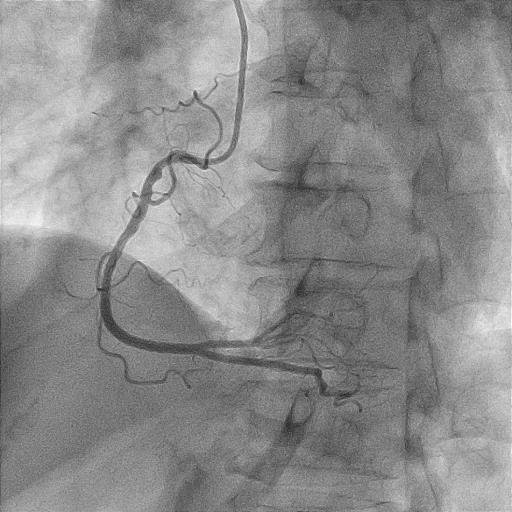
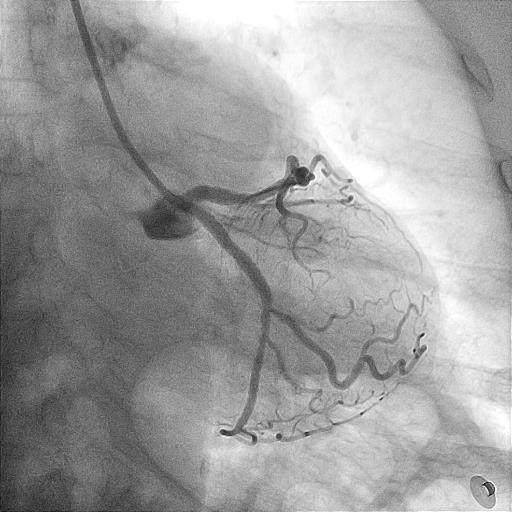
Angiography revealed very short left main (LM) with resultant selective engagement of diagnostic catheter. Left anterior descending artery (LAD) had 90 % stenosis at ostium with acute 90 degrees angulated take off from left main. There was minimal angiographic calcification. Proximal left circumflex artery (LCX) had 70 % stenosis while right coronary artery (RCA) was dominant with 50 % stenosis at proximal region.
Interventional Management
Procedural Step
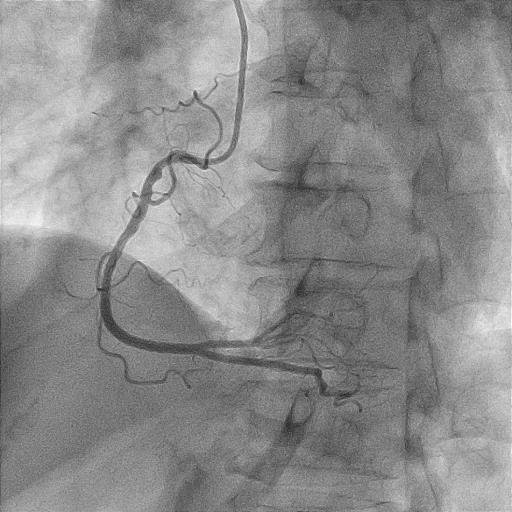
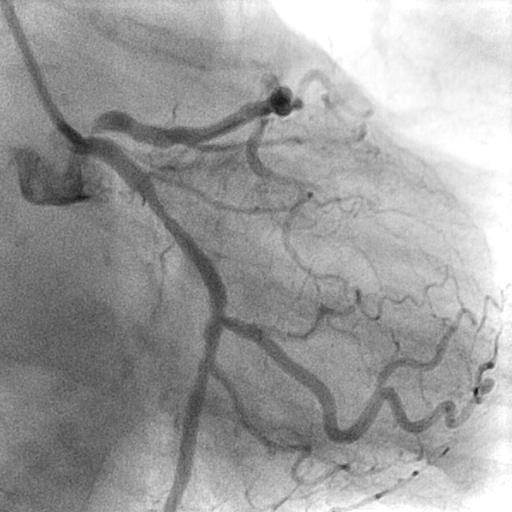
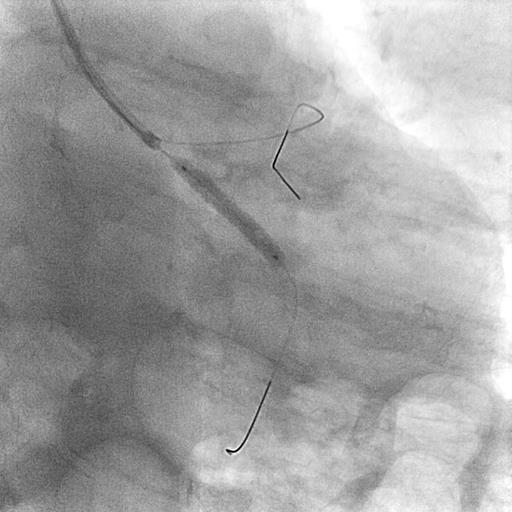
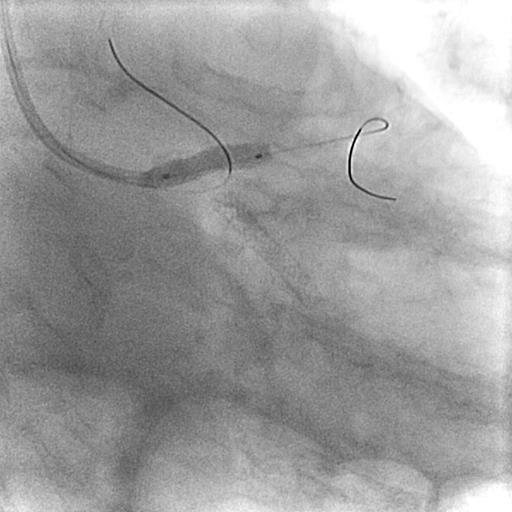
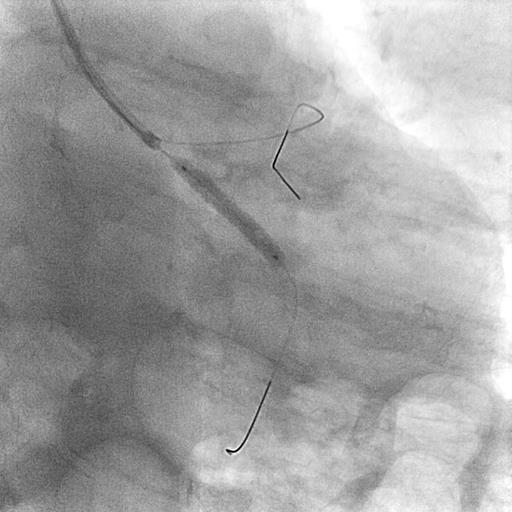
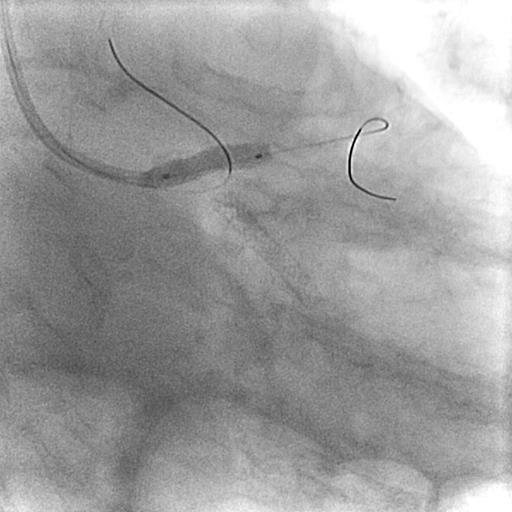
IVUS guided intervention involving LM was planned. Vascular access obtained via right radial. XB 3.0 6 French (Cordis, U.S) catheter carefully manipulated to engage LM as selective intubation into ostial LAD plaque may risk dissection. Guider position stabilised by foremost wiring LCX with Runthrough Floppy (Terumo, Japan), followed by wiring LAD with second Runthrough Floppy. Upfront IVUS run of LCX and LAD done. Proximal LCX had 70 % plaque with vessel size 3.2 mm while ostial LAD had 90 % plaque with vessel size 4.4 mm and superficial calcification < 180 degrees. Provisional approach of LM to LAD stenting was planned. Due to inevitable jailing of LCX, proximal LCX lesion was intervened first. LCX was predilated with Emerge 2.5 x 15 mm (Boston, U.S) at 16 atm and stented with Promus Elite 3.0 x 20 mm (Boston, U.S) followed by postdilatation with NC Emerge 3.0 x 12 mm (Boston,U.S) at 16 atm. Ostial LAD incrementally predilated due to watermelon seeding with Emerge 2.5 x 15 mm up to 22 atm. Due to short LM and difficulty identifying aorto-ostial junction angiographically, a sepal wire technique using Runthrough Floppy was used to guide ostial LM stent placement and prevent guider engagement. Ostial LM to LAD stented with Promus Elite 4.0 x 12 mm and flared with NC Emerge 4.0 x 8 mm up to 22 atm. Final IVUS run showed no edge dissection with good stent apposition and expansion. LM minimum luminal area was 13.4 mm2, while LAD minimum luminal area was 11.5 mm2.
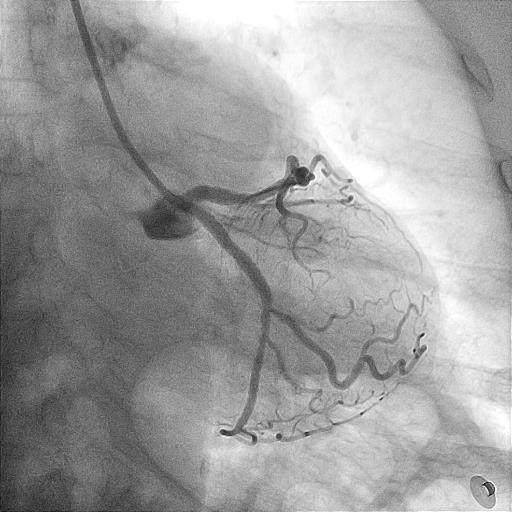
Case Summary
Very short LM with ostial LAD stenosis intervention posed some unique challenges. Selective guider engagement bias into ostial LAD plaque may potentially risk dissection. In provisional LM to LAD stenting, side branch lesion should be treated first to avoid jailing LCX for future access. In short LM with ambiguous aorto-ostial junction angiographically, sepal wire may guide accurate stent placement while preventing guider engagement. LM intervention should be imaging guided, preferentially IVUS, for stent size selection and optimisation.


