Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-046
PCI in a Calcified Vessel: Strategies and Importance of Intravascular Imaging
By Vicknesan Kulasingham, Mahadevan Gurudevan, Kumutha Gobal, Adelyn Nisha Henry, Tee Choon Keong, Kim Fong Ng, Azrina Abdul Kadir, Chu Zhen Quek, Heng Shee Kim
Presenter
Vicknesan Kulasingham
Authors
Vicknesan Kulasingham1, Mahadevan Gurudevan2, Kumutha Gobal3, Adelyn Nisha Henry3, Tee Choon Keong3, Kim Fong Ng3, Azrina Abdul Kadir4, Chu Zhen Quek3, Heng Shee Kim3
Affiliation
Ministry of Health Malaysia, Malaysia1, Sultanah Amina Hospital, Malaysia2, Sultanah Aminah Hospital, Malaysia3, KPJ Bandar Dato Onn Specialist Hospital, Malaysia4,
View Study Report
TCTAP C-046
CORONARY - Adjunctive Procedures (Thrombectomy, Atherectomy, Special Balloons)
PCI in a Calcified Vessel: Strategies and Importance of Intravascular Imaging
Vicknesan Kulasingham1, Mahadevan Gurudevan2, Kumutha Gobal3, Adelyn Nisha Henry3, Tee Choon Keong3, Kim Fong Ng3, Azrina Abdul Kadir4, Chu Zhen Quek3, Heng Shee Kim3
Ministry of Health Malaysia, Malaysia1, Sultanah Amina Hospital, Malaysia2, Sultanah Aminah Hospital, Malaysia3, KPJ Bandar Dato Onn Specialist Hospital, Malaysia4,
Clinical Information
Patient initials or Identifier Number
YSM
Relevant Clinical History and Physical Exam
82years old gentleman with background history of T2DM and Hypertension. He had previous history of admission for NSTEMI and
Unstable angina. Currently CCSII-III and NYHA 1. ADL independent. Non smoker. Decided for angiogram in view of recurrent chest pain.
Clinically there are no signs of heart failure and vital signs were stable.
Relevant Test Results Prior to Catheterization
Hemoglobin 12.2 g/dL, WBC 5.2x10^3/L, Platelets 333x10^3/Lurea 3.6mmol/L, Creatinine 71 micromol/LSodium 140mmol/L, Potassium 4.0 mmol/L
Chest radiograph: clear lung fields, cardiomegalyECG sinus rhythm, no ST changes
Echocardiography: Good LV function, EF 60%, no regional wall abnormalities, dilated LA, normal RV function, mild MR and TR
Chest radiograph: clear lung fields, cardiomegalyECG sinus rhythm, no ST changes
Echocardiography: Good LV function, EF 60%, no regional wall abnormalities, dilated LA, normal RV function, mild MR and TR
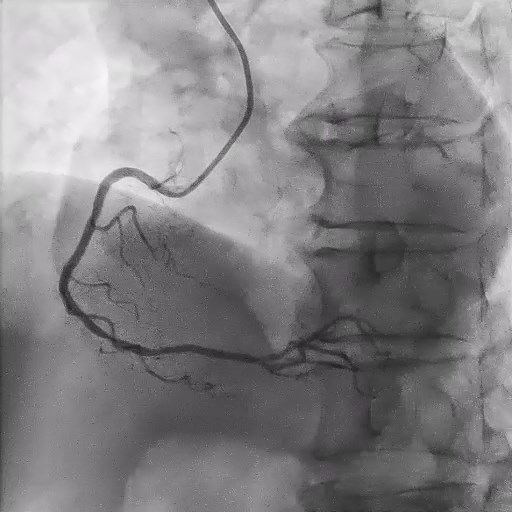
Relevant Catheterization Findings
Left main is normal
Ostial to mid left anterior descending artery 70-80% stenosis and heavily calcifiedOM1 80% stenosis
RCA fairly normal


Interventional Management
Procedural Step
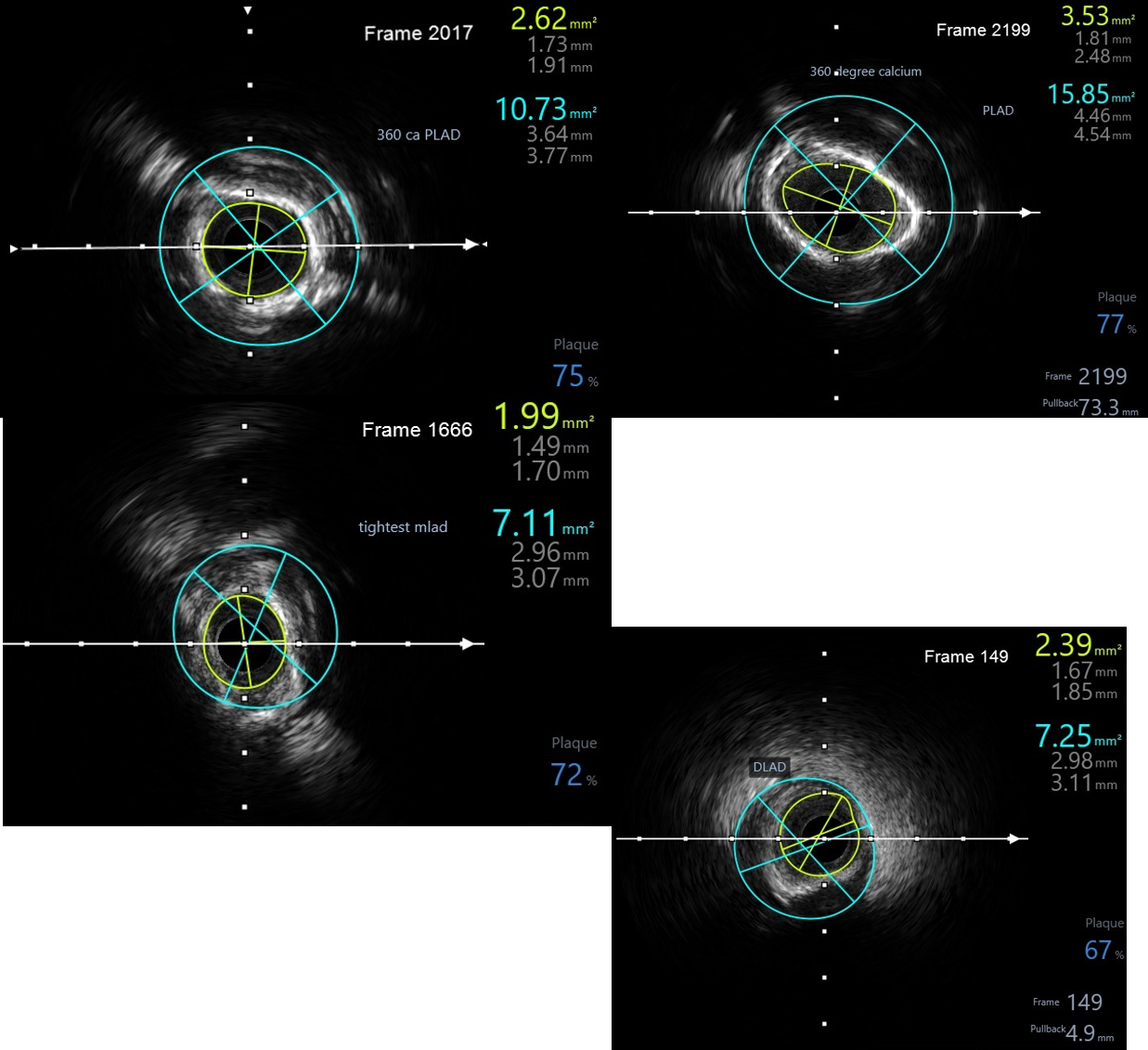
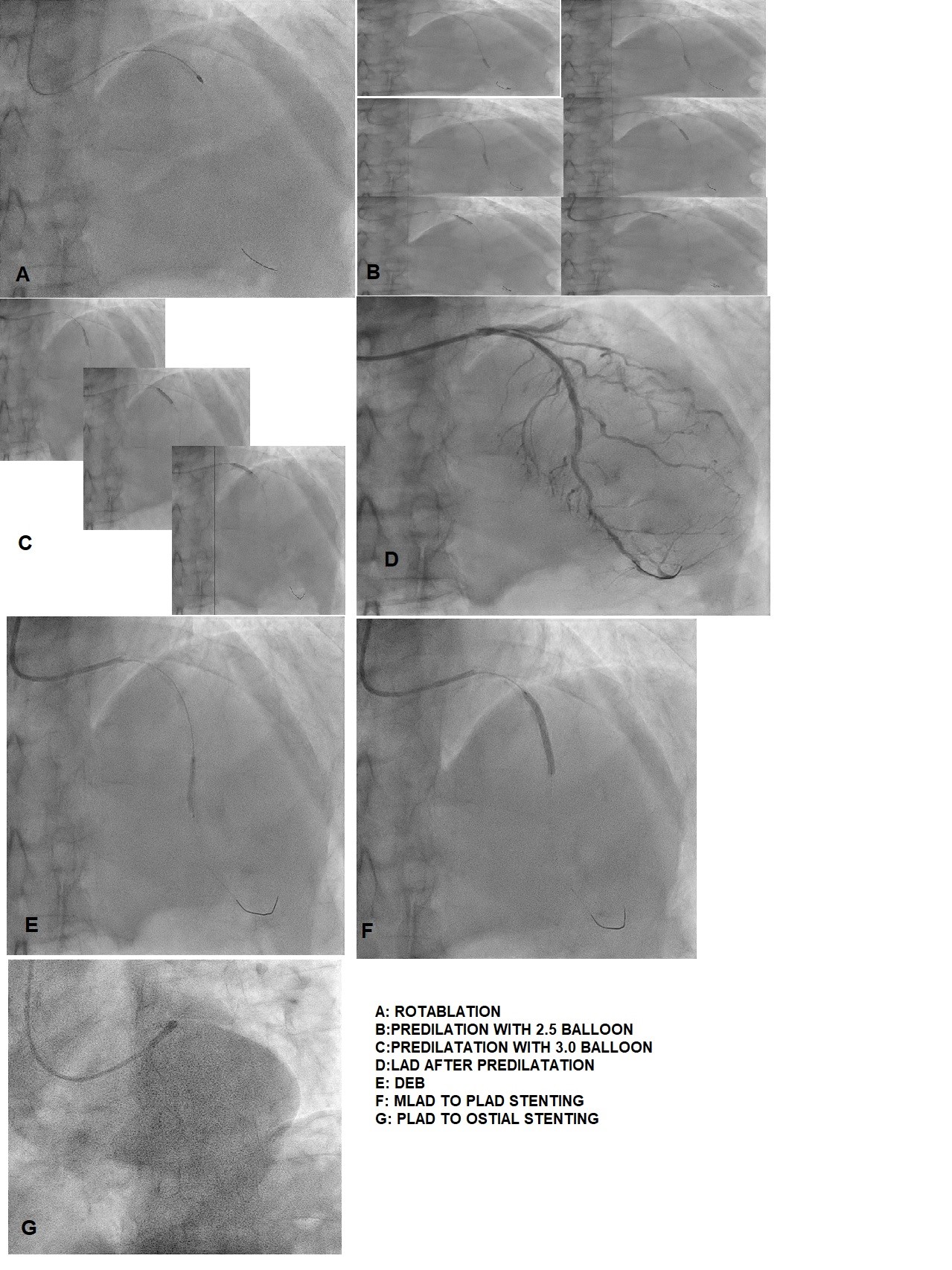
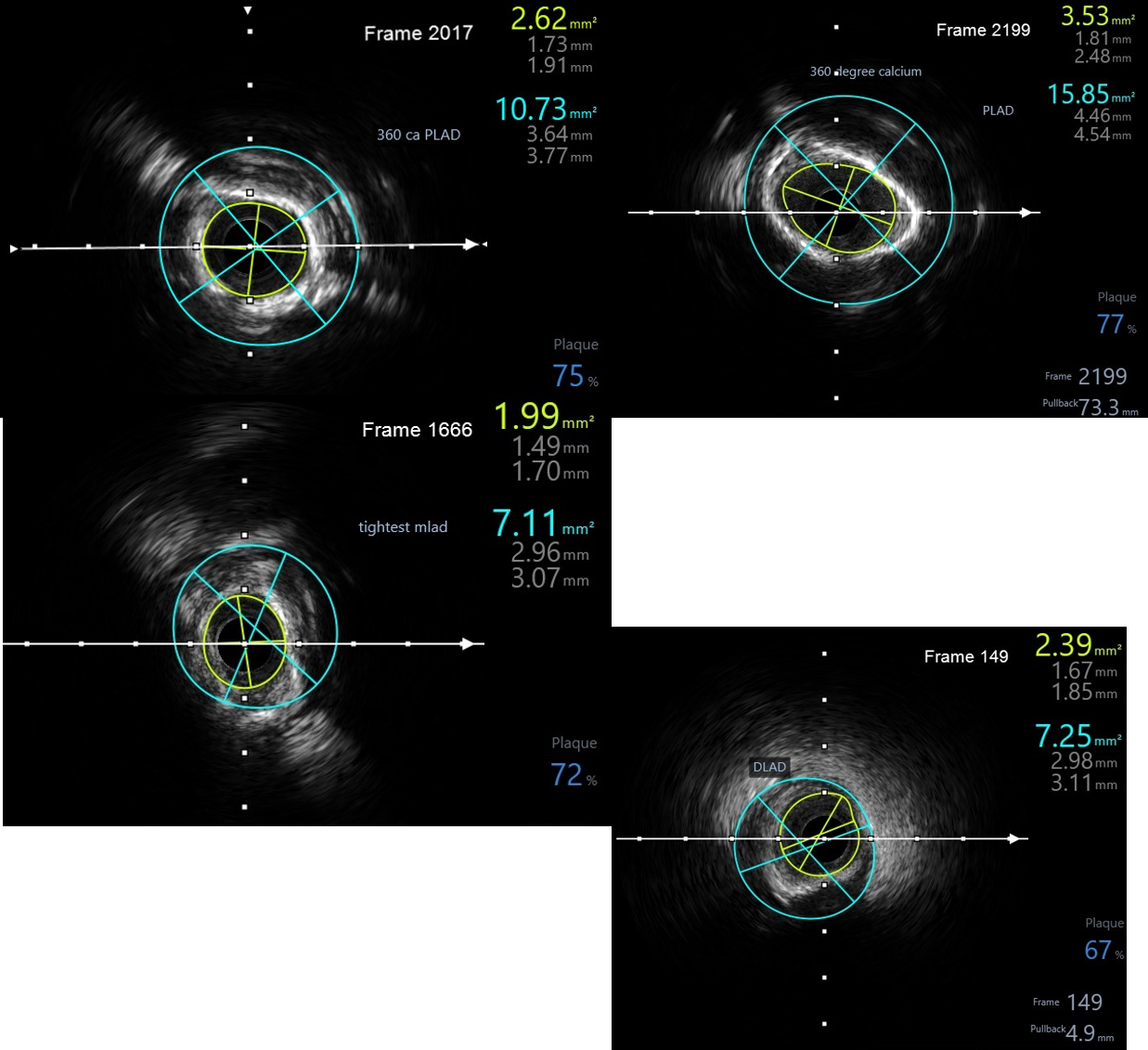
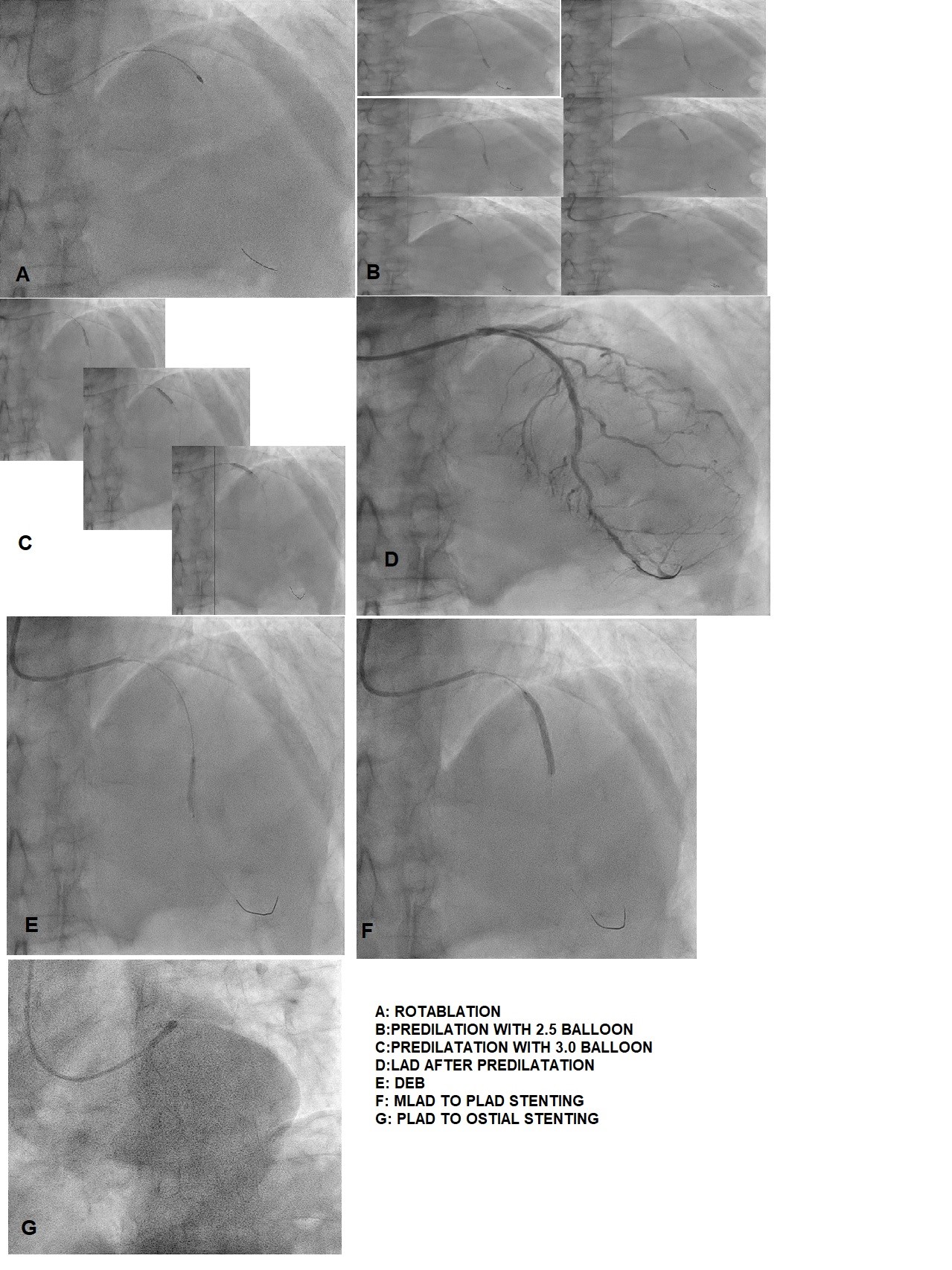
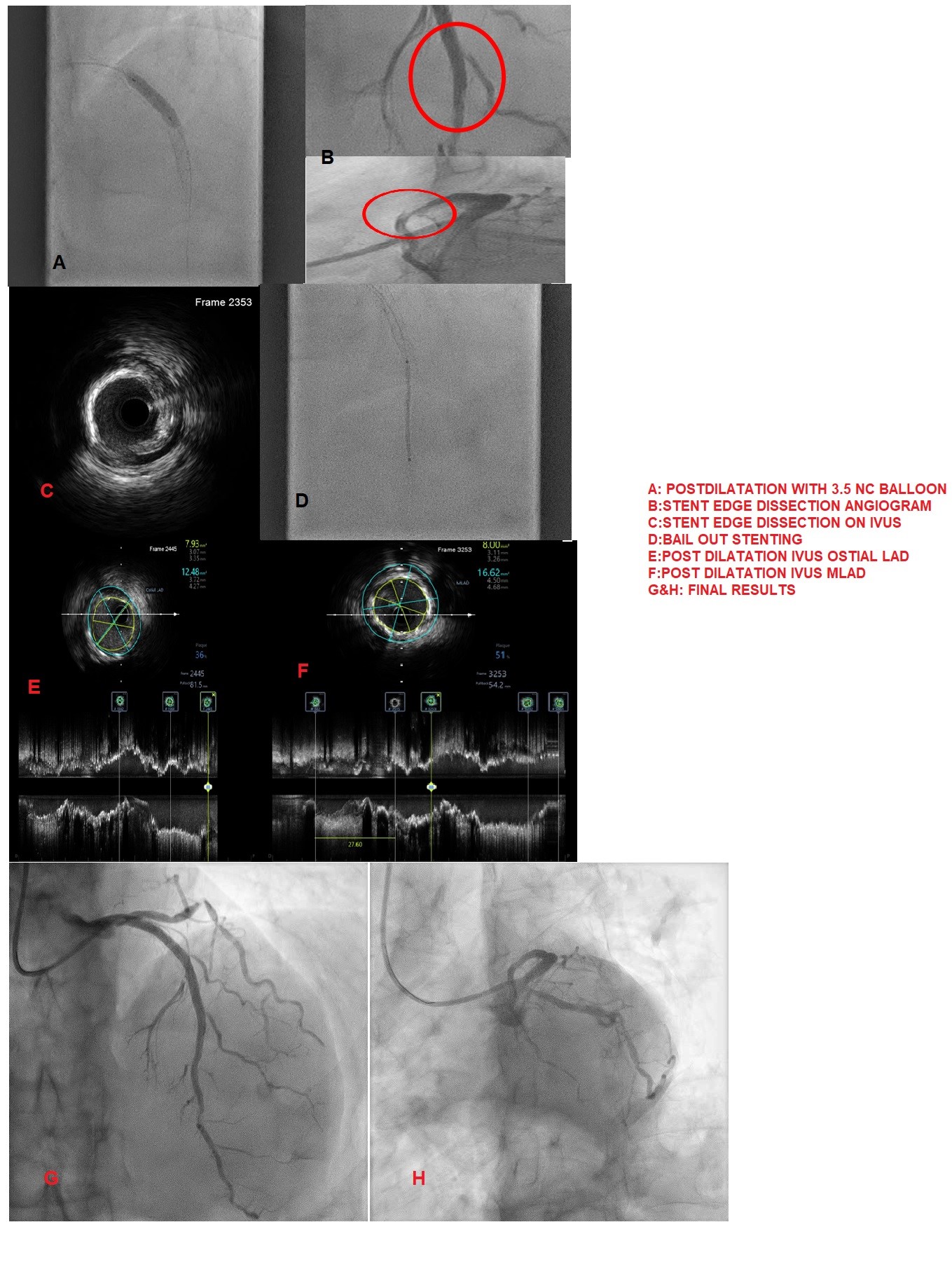
PCI to LAD and strategy was IVUS guided PCI and KIV for athrectomy. Right radial approach. Engaged with 6Fr XB3.0 guiding catheter and wired to DLAD with runthrough floppy wire.First IVUS run showed heavily calcified vessel with areas of 360 degree calcium ring with tightest MLA of 1.99mm2 at MLAD and average plaque burden of 77%. Decided for rotablation and wire is exchanged with rota wire with a MC. Total 4 runs at 180k RPM was done with a 1.5mm burr.Predilated with 2.5x15mm cutting balloon from DLAD to Ostium at 6-24atm.Cutting balloon 3.0x15mm from MLAD to ostium at 12-18atm.DCB 2.25mmx20mm to DLAD at 6atm for 60sec.Stented MLAD to PLAD with 3.0x32mm and PLAD to Ostium with 3.5x24mm stent.2nd IVUS showed some area of underexpansion and malapposed stent.Post dilated with NC 3.5x15mm at 12-22atm.MLAD distal stent edge dissection seen and confirmed by IVUS.IVUS also showed well apposed and expanded MLAD and PLAD stent but little under expanded at the ostium.Decided for bail out stenting for the DLAD with 2.5x28mm stent.Post dilated PLAD stent with NC 4.0x15mm at 16atm.Post dilated distal stent with NC 2.5x15mm at 14atm. Final IVUS showed adequate stent MSA, well apposed and expanded stent with no edge dissection.
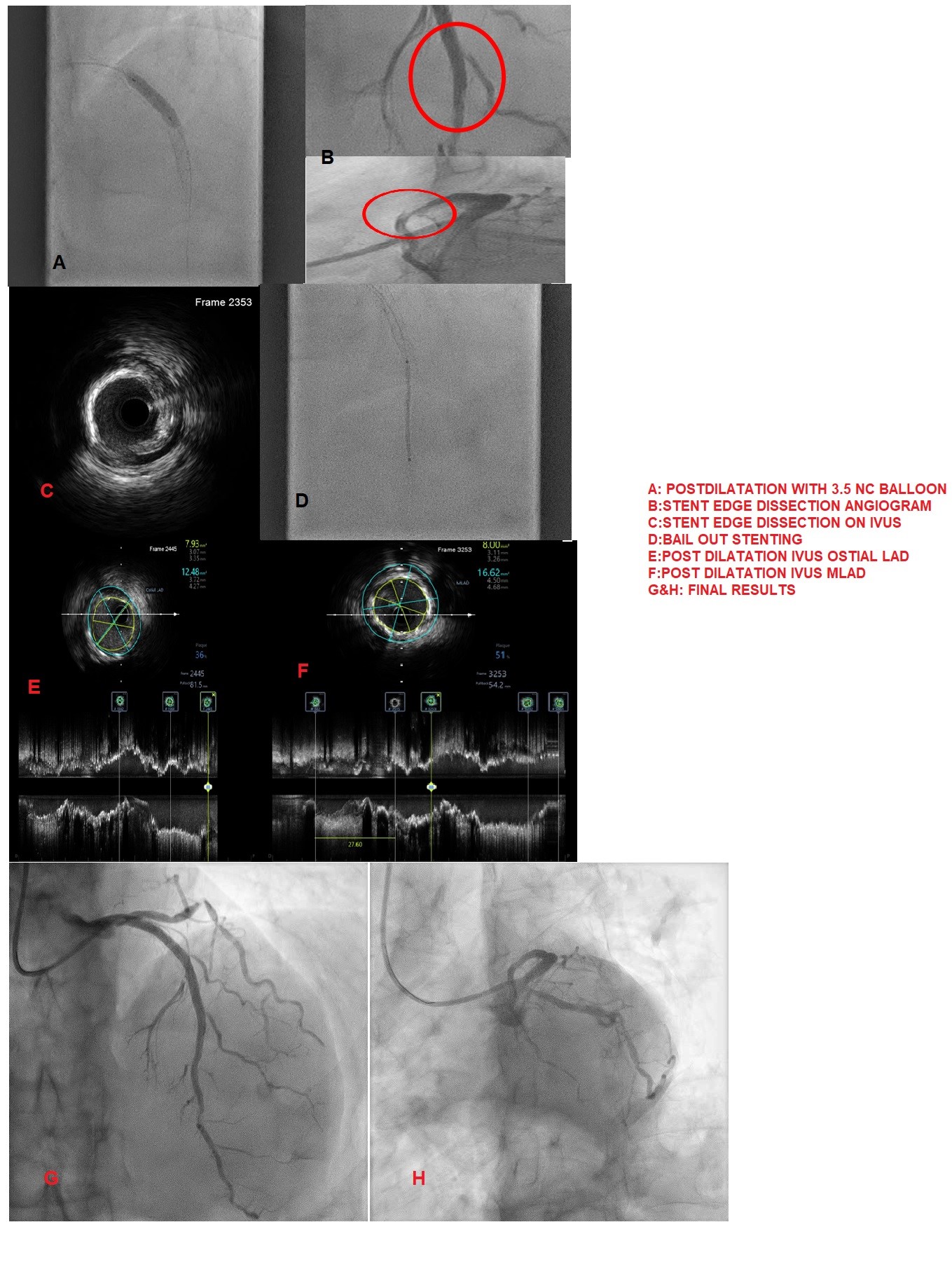
Case Summary
Patient with severely calcified coronaries have overall higher mortality hence accurate characterization of calcium distribution and morphology is key to successful treatment. Coronary angiography grossly underestimates the presence, extent, severity, and depth of coronary calcification. Intravascular imaging provides comprehensive assessment of the calcified lesion there by facilitating a tailored strategy for lesion preparation and appropriate atherectomy device selection. Intravascular imaging also provides us information with regards to vessel size, diameter, landing zones and also in making sure that post PCI optimization targets achieved along with identifying complications post stenting.


