Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-100
Characteristics of Non-Invasive Hemodynamic Monitoring in Left and Right-Sided Heart Failure Patients
By Jiun Yu Guo, Shih-Hsien Sung
Presenter
Jiun Yu Guo
Authors
Jiun Yu Guo1, Shih-Hsien Sung2
Affiliation
Taipei Veterans General Hospital, Taiwan1, National Yang Ming Chiao Tung University, Taiwan2
View Study Report
TCTAP A-100
Others (Structural Heart Disease)
Characteristics of Non-Invasive Hemodynamic Monitoring in Left and Right-Sided Heart Failure Patients
Jiun Yu Guo1, Shih-Hsien Sung2
Taipei Veterans General Hospital, Taiwan1, National Yang Ming Chiao Tung University, Taiwan2
Background
Ambulatory blood-pressure monitoring (ABPM) and arterial stiffness have established their role in the evaluation of hypertension. The application of both parameters among heart failure (HF) patients was less mentioned and investigations were mainly focused on advanced congestive heart failure patients. In addition, the physiological and pathological differences between left and right-sided HF are significant. The information regarding circadian blood pressure variation and arterial stiffness was limited. Our study aimed to investigate the characteristics of hemodynamic alteration between left and right-sided HF with the use of non-invasive hemodynamic measurements.
Methods
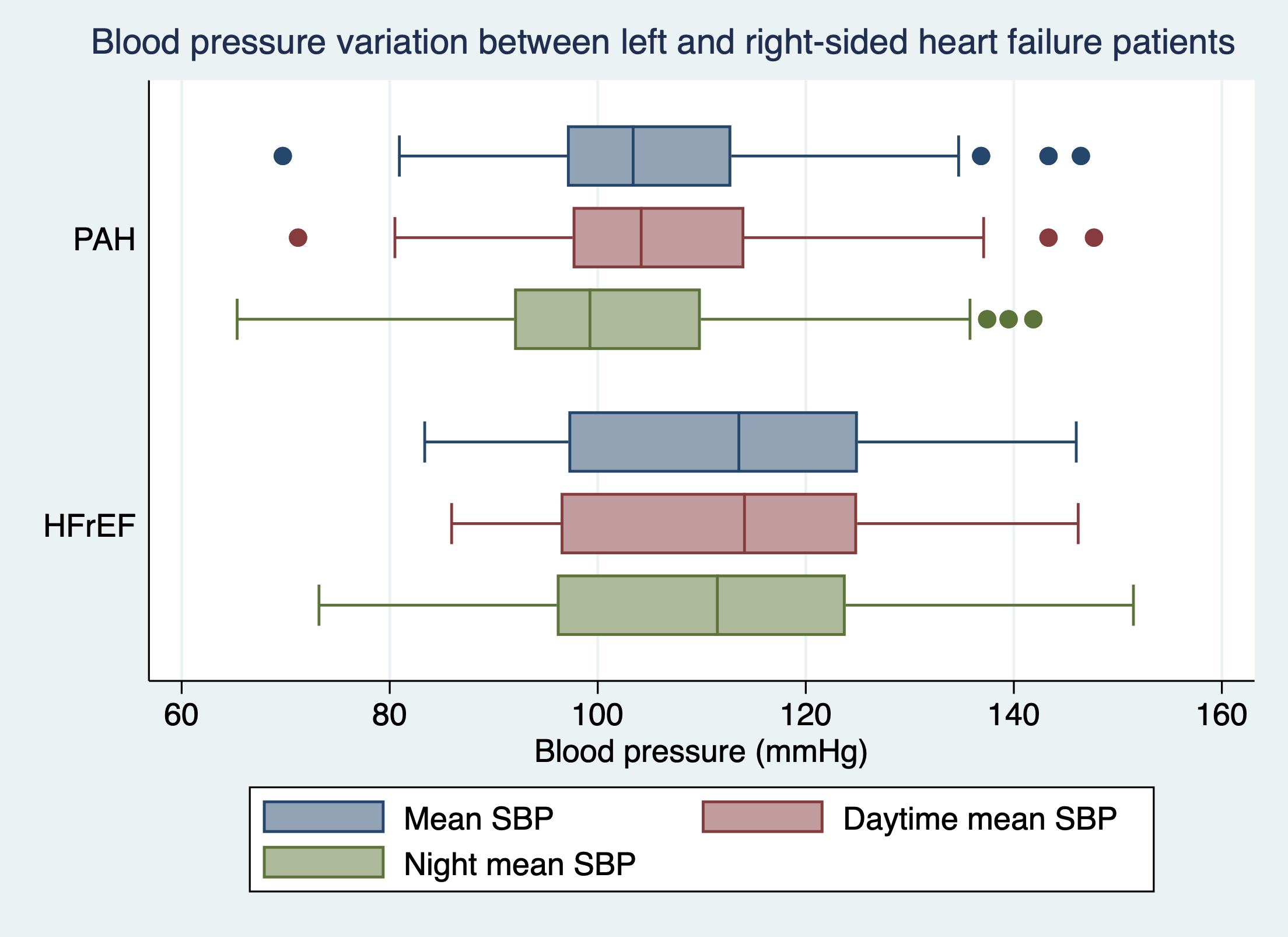
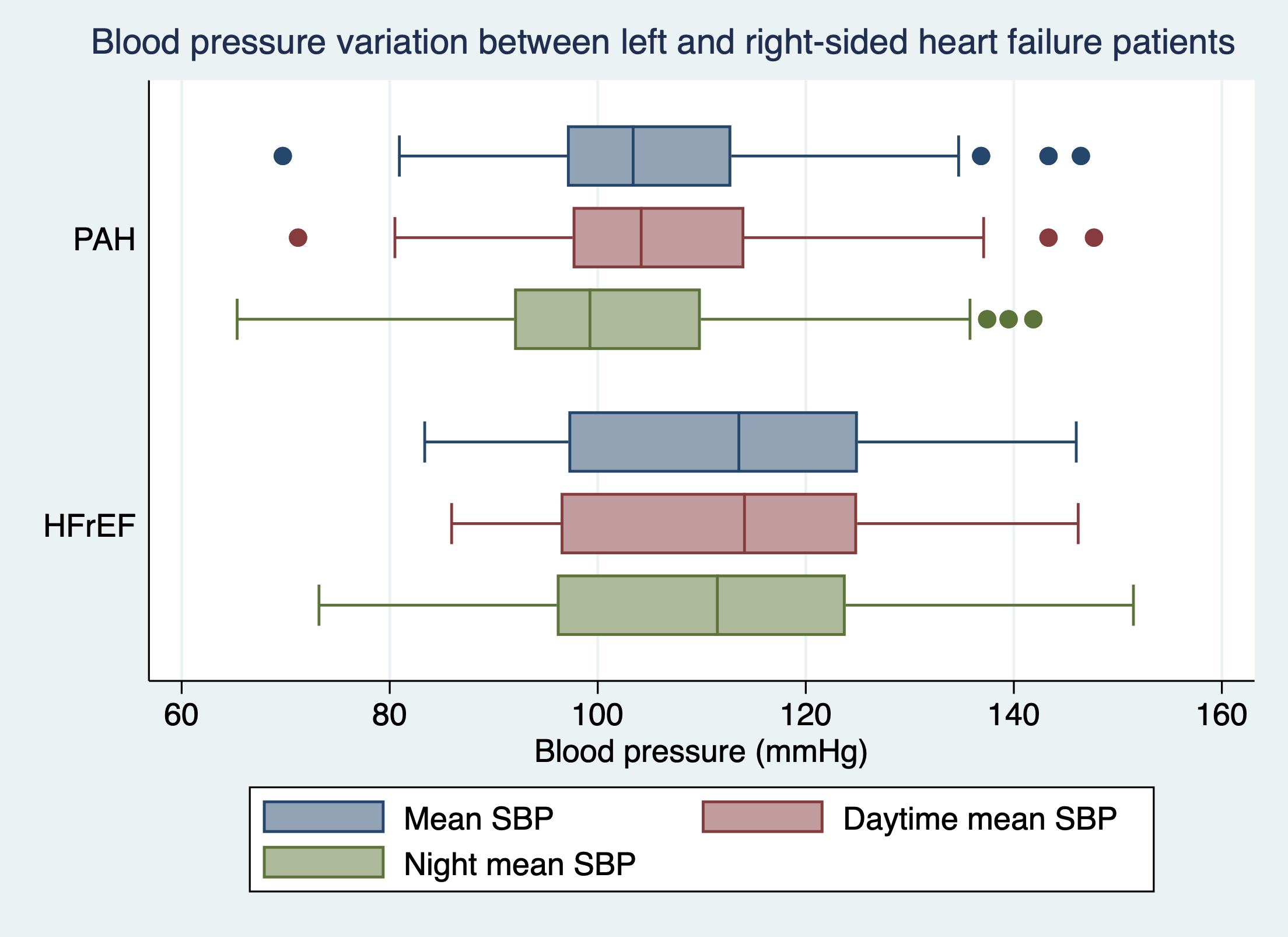
Adult patients who presented with heart failure symptoms (NYHA class II or more) were enrolled in this study. Subjects were classified as pulmonary arterial hypertension (PAH) and HF with reduced ejection fraction (HFrEF) to represent right and left-sided HF based on definition, respectively. A detailed chart review was conducted to collect information on demographic characteristics, comorbidities, comedications, and laboratory parameters. The 24-hour ABPM was performed for the measurement of circadian hemodynamic patterns. Pulsatile hemodynamics, including carotid-femoral pulse wave velocity (cf-PWV), carotid augmentation index (cAI), and backward pressure amplitude (Pb) were measured. Echocardiography was performed concordantly as confirmation of HF characteristics. The data were compared using non-parametric methods.
Results
Among a total of 135 patients who were enrolled in this study (median age 53 years old, 50% male), there were 81 patients were classified as PAH and 54 patients as HFrEF. The PAH group was younger [median age 47 years old vs. 60 years old, p<0.001] and had more female patients (78% vs. 22.6%, p<0.001).
Conclusion
Our study demonstrated the distinctive characteristics between left and right-sided HF from 24-hour ABPM and pulsatile hemodynamics measurements. The loss of normal pressure dipping and increased arterial stiffness were more prominent among left-sided heart failure patients.


