TCTAP A-042
Complications (Coronary)
An Umbrella Review of the Meta Analyses About Risk and Protective Factors for Post-discharge Bleeding Events in Percutaneous Coronary Intervention Setting
Ricardo Adrian Nugraha1, Bagus Khrisna2, Tony Santoso Putra3, Primasitha Maharany Harsoyo4, Michael Jonatan2, Lalu Galih Pratama Rinjani3, I Gde Rurus Suryawan5, Yudi Her Oktaviono2
Universitas Airlangga - Dr Soetomo General Hospital, Indonesia1, Airlangga University, Indonesia2, Dr. Soetomo General Hospital, Indonesia3, General Regional Academic Hospital Dr. Soetomo, Universitas Airlangga, Indonesia4, Dr. Soetomo Academic General Hospital, Indonesia5
Background
Background: Major bleeding events (MBE) were uncommon in patients undergoing PCI. The presence of MBE are associated with increase in mortality rate; however, the timing of MBE is individually and poorly understood. Defining a standardized model for predicting post-discharge MBE risk following percutaneous coronary intervention (PCI) may help clinicians identify patients at high risk. This meta-analysis aimed to define prevalence and quantitatively analyse predictor model of MBE in patients undergoing PCI. MBE were defined according to the TIMI classification and their prevalnce was evaluated until 1 year post-discharge follow-up.
Methods: We searched Pubmed, Embase, Ovid, Web of Science, and Cochrane library from their inceptions until December 2019. Studies addressing risk factors for developing major bleeding events following PCI were eligible. We performed a random effects model using pool hazard ratios and weighted mean difference. Study quality was evaluated with Newcastle-Ottawa scale. Statistical analysis was performed using Review Manager ver 5.3.
Results: We collected 220 relevant studies including 8.563.898
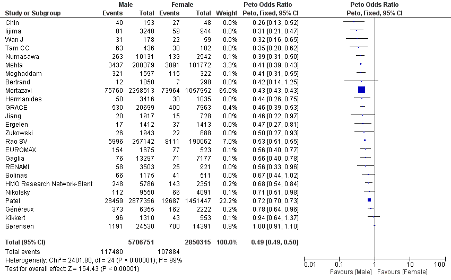
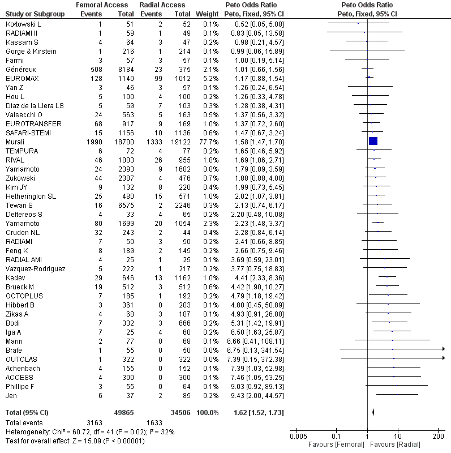
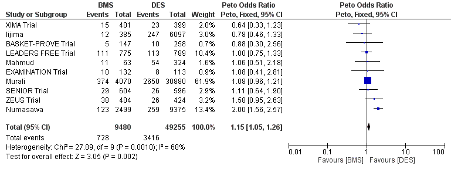
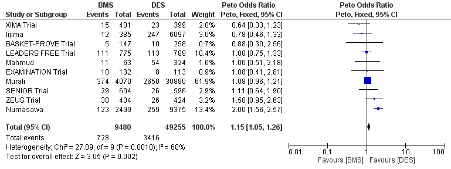
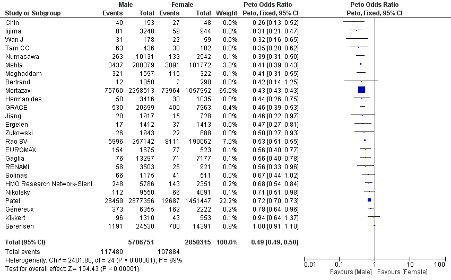
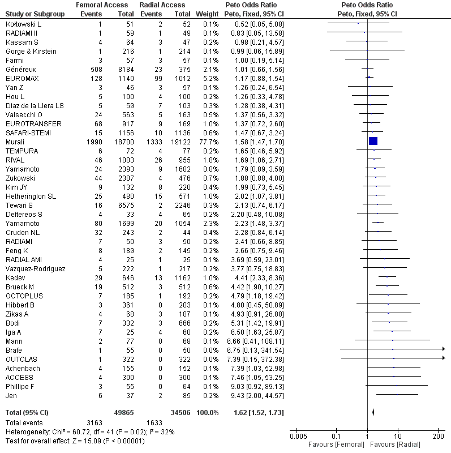
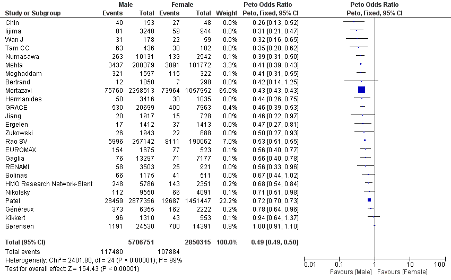
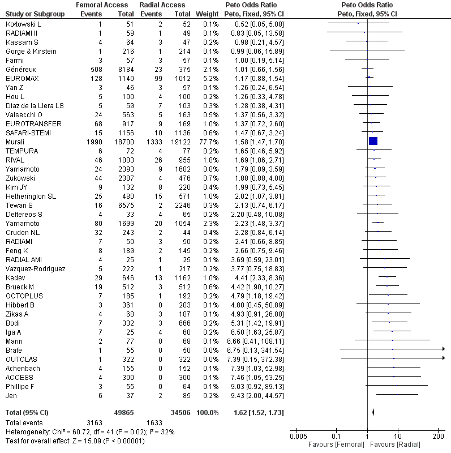
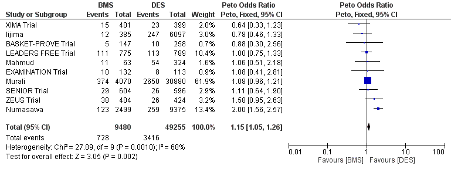
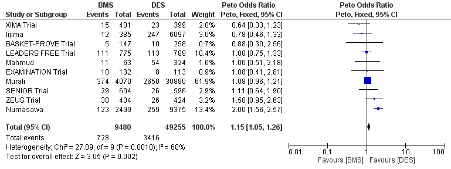
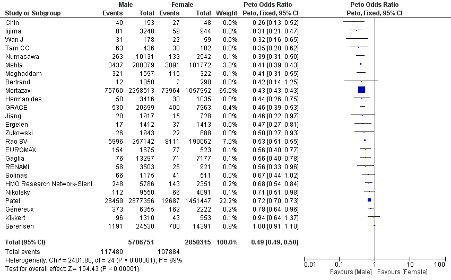
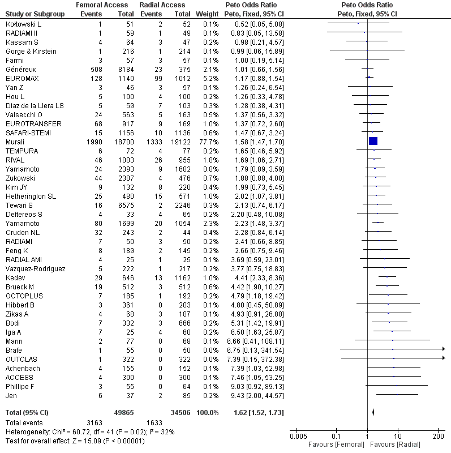
consecutive patients who underwent PCI. During in-hospital admission, major and minor bleeding events occurred in 0.95% and 2.6% of patients, respectively. It was found that age >70 years, age (per 10‐year increase), female gender, lower BMI, baseline anemia and thrombocytopenia, history of hypertension, history of diabetes, baseline creatinin clearance <60 mL/min, positive cardiac troponin, congestive heart failure, shock or prior use of inotropic medications, prior stroke, prior acute coronary syndrome, previous PCI, prior use of GPIIB/IIIA inhibitor, femoral access route, larger sheath size, longer procedural duration, multiple stents implanted, left main and chronic total occlusion are significant risk factor to develop MBE following PCI.
Conclusion: This study found several risk and protective factors which can help clinician predicting MBE and preparing an effective prevention strategy before PCI. These findings should be interpreted cautiously, since study populations might differs to real-world settings.
PROSPERO ID: CRD42020184611
Methods
This meta analysis study has been registered on PROSPERO international prospective register of systematic review, registration number (CRD 42020184611). Search strategyWe searched many databases, including PubMed, Embase, Cochrane Library, Sciencedirect, China National Knowledge Infrastructure (CNKI), and Chinese BioMedical (CBM). Queries were limited to articles published between January 2009 and December 2019 and reporting data on bleeding risk factor in acute coronary syndrome patients underwent PCI, using the following search terms: (“TIMI bleeding” OR “major bleeding event” OR “hemorraghic complication” AND (“acute coronary syndrome” OR “myocardial infarction” OR “STEMI” OR “NSTEMI”) AND (“percutaneous coronary intervention”) in either the title or the abstract.Inclusion and exclusion criteriaThe inclusion criteria were as follows: (1) written in English, (2) patients with ACS underwent PCI, (3) a prospective follow-up study, and (4) major bleeding events, and risk factors were clearly presented. The exclusion criteria were as follows: (1) duplicate publication (most recent paper was included for analysis), (2) patients with pharmaco-invasive strategies included, and their data could not be separately identified; (3) animal experiments, case reports, case series, reviews, and studies on prevention. Three reviewers) independently searched databases, included and excluded papers, and assessed the data on methodological assessment. Study selectionThe searches yielded a total of 6810 titles and abstracts that were screened for potential relevance, from which 550 articles were selected for further consideration after the removal of duplicate publications and met inclusion criteria. The abstracts of these 550 papers were reviewed, leaving 300 potentially relevant studies that were examined in more detail. Of these, 250 of studies included in qualitative synthesis , 220 of studies included in quantitative synthesis (meta-analysis).
Results
We collected
220 relevant studies including
8.563.898 consecutive patients who underwent PCI. During in-hospital admission, major and minor bleeding events occurred in 0.95% and 2.6% of patients, respectively. It was found that age >70 years, age (per 10‐year increase), female gender, lower BMI, baseline anemia and thrombocytopenia, history of hypertension, history of diabetes, baseline creatinin clearance <60 mL/min, positive cardiac troponin, congestive heart failure, shock or prior use of inotropic medications, prior stroke, prior acute coronary syndrome, previous PCI, prior use of GPIIB/IIIA inhibitor, femoral access route, larger sheath size, longer procedural duration, multiple stents implanted, left main and chronic total occlusion are significant risk factor to develop MBE following PCI.
Conclusion
This study is the first systematic review and meta‐analysis to evaluate risk and protective factors for periprocedural major bleeding after PCI using prospective cohort and retrospective studies. The results of this study can contribute significantly to clinical practice. Firstly, it can help clinicians to pay close attention to high‐risk groups where major bleeding may be more likely after PCI. Secondly, for some baseline parameters that cause major bleeding, effective intervention can be conducted, for example, to limit the heparin dosage. Thirdly, findings can assist nurses to provide more targeted care and interventions. Overall, study findings can assist in the management of this potentially fatal complication. Bleeding complications are an inevitable consequence of PCI. Awareness of the predictors and importance of major peri-procedural bleeding as well as the judicious use of efficacious bleeding avoidance strategies will optimize outcomes of PCI procedures undertaken.