Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-058
Incidence and Characteristics of Intravascular Ultrasound Detected Myocardial Bridgings of Left Anterior Descending Arteries Culprit of Acute Coronary Syndromes
By Mohamed Saad-Eddine Bouzghaia, Chakib Lamraoui, Khalil Lebcira
Presenter
Mohamed Saad-Eddine Bouzghaia
Authors
Mohamed Saad-Eddine Bouzghaia1, Chakib Lamraoui2, Khalil Lebcira2
Affiliation
El Besma Private Hospital, Algeria1, Universitary Hospital of Bejaia, Algeria2
View Study Report
TCTAP A-058
Imaging: Intravascular
Incidence and Characteristics of Intravascular Ultrasound Detected Myocardial Bridgings of Left Anterior Descending Arteries Culprit of Acute Coronary Syndromes
Mohamed Saad-Eddine Bouzghaia1, Chakib Lamraoui2, Khalil Lebcira2
El Besma Private Hospital, Algeria1, Universitary Hospital of Bejaia, Algeria2
Background
Myocardial bridging (MB) is the most common congenital coronary variation, and is the most commonly located in the left anterior descending artery (LAD) middle segment. A 27% incidence of LAD MB has been reported in unselected necropsy series. In vivo, intravascular ultrasound (IVUS) and coronary computed tomography angiography (CCTA) are accurate imaging modalities to detect and characterize MB, whereas coronary angiography alone detects only a small proportion of MB.
Methods
We retrospectively analyzed IVUS studies of consecutive patients admitted to the cardiology department of the Universitary Hospital of Bejaia (Algeria) for acute coronary syndrome and a presumed culprit lesion located in the LAD, from January to August 2022.
We estimated maximum plaque burden (PB) in the tunneled segment. A PB of more than 50% defined significant tunneled segment disease.
Measurements are expressed as means ± standard deviation.
We estimated maximum plaque burden (PB) in the tunneled segment. A PB of more than 50% defined significant tunneled segment disease.
Measurements are expressed as means ± standard deviation.
Results
Seventy-four patients were included in the study (78% males, 22% females). Mean age was 62 ± 13 years (60 ± 14 years for males, and 70 ± 7 years for females).
MB length was 14.6 ± 8.97 mm (minimum: 1.5 mm ; maximum: 33 mm; 95% confidence interval of mean: [11.15; 18.04] mm).
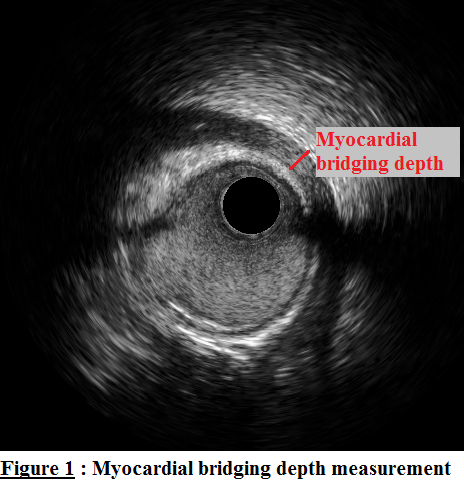
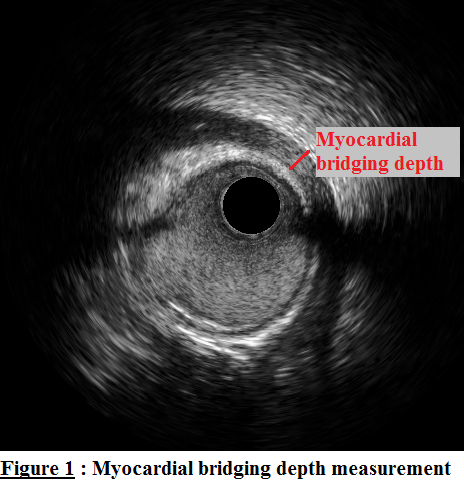
MB depth was 0.83 ± 0.54 mm (minimum: 0.25 mm ; maximum: 2.6 mm; 95% confidence interval of mean: [0.62; 1.04]mm).
Significant tunneled segment disease was found in 21% of MB (6 of 28), but extended beyond the first 3 mm of tunneled segment extremities in only 2 patients (7 % of MB).
A Point-biserial correlation did not show a significant correlation between MB depth, length or systolic compression index and significant tunneled segment disease (respectively rpb = -0.1, p = 0.622; rpb = 0.01, p= 0.964; rpb = 0.09, p = .666).
MB length was 14.6 ± 8.97 mm (minimum: 1.5 mm ; maximum: 33 mm; 95% confidence interval of mean: [11.15; 18.04] mm).
MB depth was 0.83 ± 0.54 mm (minimum: 0.25 mm ; maximum: 2.6 mm; 95% confidence interval of mean: [0.62; 1.04]mm).
Significant tunneled segment disease was found in 21% of MB (6 of 28), but extended beyond the first 3 mm of tunneled segment extremities in only 2 patients (7 % of MB).
A Point-biserial correlation did not show a significant correlation between MB depth, length or systolic compression index and significant tunneled segment disease (respectively rpb = -0.1, p = 0.622; rpb = 0.01, p= 0.964; rpb = 0.09, p = .666).
Conclusion
Incidence of LAD MB in our study population was 37.8%, which is higher than the reported incidence in unselected population and chronic coronary syndrome population, suggesting a causal relationship of MB in the occurrence of acute coronary syndromes. However MB varied widely in length and depth and larger longitudinal studies are necessary to define "pathologic" MB.
Presence of significant atherosclerosis in the tunneled segment was not rare (21% of MB). Thus, if a percutaneous coronary intervention (PCI) with stent implantation was planned, landing the stent in the MB had to be considered.
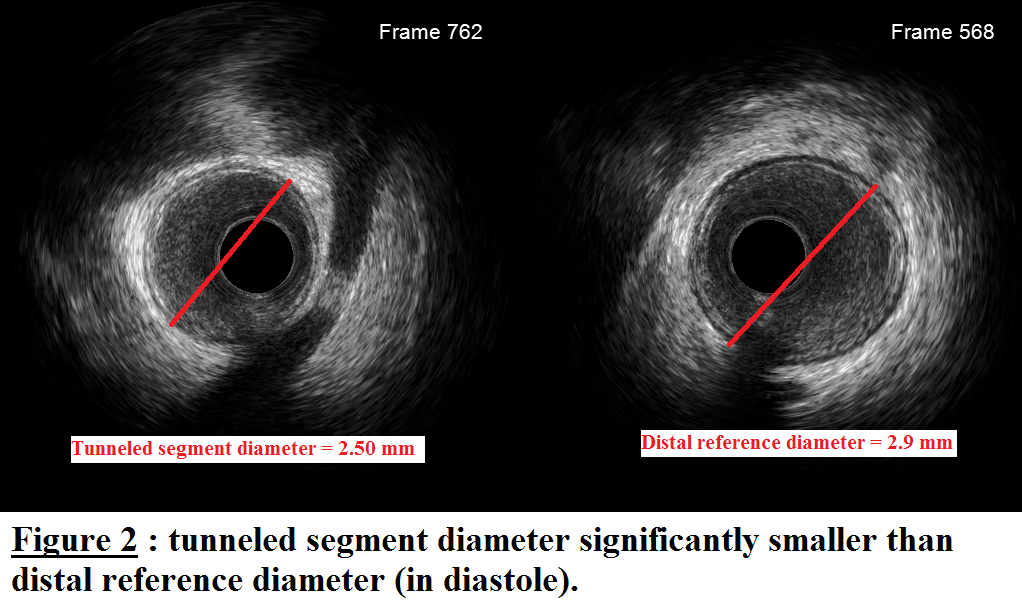
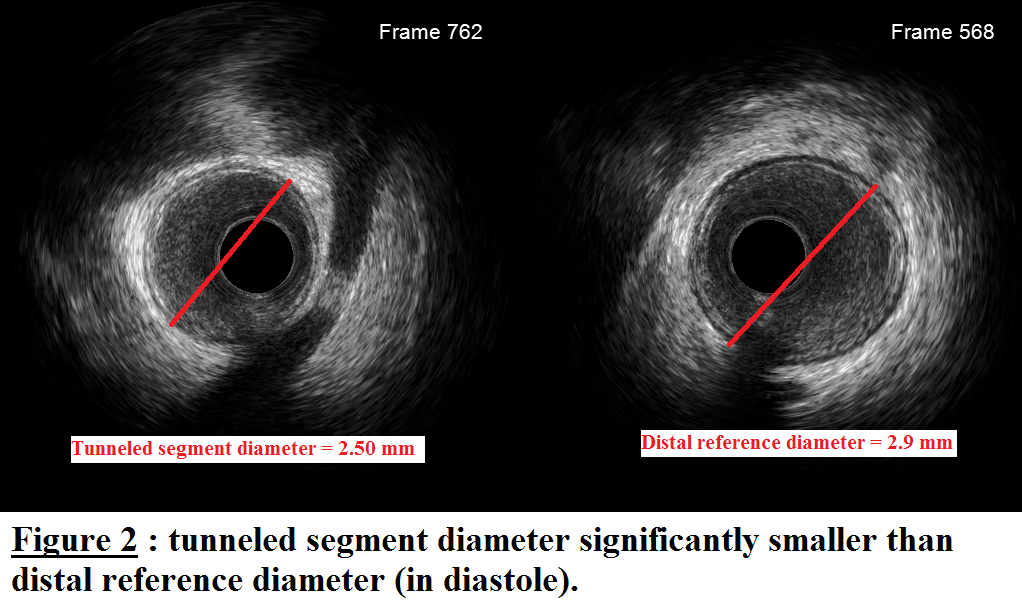
Interestingly, tunneled segment diameter in diastole was found to be smaller than the distal reference diameter, which might explain the reported increased risk of coronary perforation during tunneled segment PCI.
MB depth correlated better than systolic compression index with the difference between distal reference diameter and tunneled segment diameter.
Presence of significant atherosclerosis in the tunneled segment was not rare (21% of MB). Thus, if a percutaneous coronary intervention (PCI) with stent implantation was planned, landing the stent in the MB had to be considered.
Interestingly, tunneled segment diameter in diastole was found to be smaller than the distal reference diameter, which might explain the reported increased risk of coronary perforation during tunneled segment PCI.
MB depth correlated better than systolic compression index with the difference between distal reference diameter and tunneled segment diameter.


