Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-017
Acute Coronary Syndrome in Very Elderly Patients: Long-Term Clinical Outcome With or Without Percutaneous Coronary Intervention, a Single Centre Experience.
By Vipin Thomachan, Ali Shamsi, Gohar Jamil, Ahmed Siddiqui, Mohammed El-Harari, Andria Maria Badics, Sadek Mokahal, Anwar Al Zaabi, El Shafie Taha, Maha Al Ketbi, Khaled Shaheen, Soviachen Kurian, Mohammed Anasullah Siddiqui
Presenter
Vipin Thomachan
Authors
Vipin Thomachan1, Ali Shamsi1, Gohar Jamil1, Ahmed Siddiqui1, Mohammed El-Harari1, Andria Maria Badics1, Sadek Mokahal1, Anwar Al Zaabi1, El Shafie Taha1, Maha Al Ketbi1, Khaled Shaheen1, Soviachen Kurian2, Mohammed Anasullah Siddiqui3
Affiliation
Tawam Hospital, United Arab Emirates1, Royal Hobart hospital, Australia2, RAK Health Sciences University, United Arab Emirates3
View Study Report
TCTAP A-017
Acute Coronary Syndromes (STEMI, NSTE-ACS)
Acute Coronary Syndrome in Very Elderly Patients: Long-Term Clinical Outcome With or Without Percutaneous Coronary Intervention, a Single Centre Experience.
Vipin Thomachan1, Ali Shamsi1, Gohar Jamil1, Ahmed Siddiqui1, Mohammed El-Harari1, Andria Maria Badics1, Sadek Mokahal1, Anwar Al Zaabi1, El Shafie Taha1, Maha Al Ketbi1, Khaled Shaheen1, Soviachen Kurian2, Mohammed Anasullah Siddiqui3
Tawam Hospital, United Arab Emirates1, Royal Hobart hospital, Australia2, RAK Health Sciences University, United Arab Emirates3
Background
Coronary artery disease (CAD) is a leading cause of morbidity and mortality worldwide and its prevalence increases with advancing age. Management of acute coronary syndrome (ACS) in the very elderly patient is challenging, quiet often leading to unfavorable outcome as this group is less likely to receive standard guideline directed therapy due to multiple reasons like atypical presentations, delay in recognition, more complex CAD, frailty, cognitive impairment, multiple co-morbidities etc. They are underrepresented in clinical trials comparing management strategies in acute coronary syndrome.
Methods
This retrospective cohort study was aimed to evaluate the mid to long term outcome of treatment strategies in octogenarians presenting with acute coronary syndrome.
Results
In-hospital (17.5% vs 11.5%; p value0.3248) and 6-month (21.9% vs 13.5%; p=0.2045) mortality was numerically high in conservative group but it was not statistically significant. One-year all-cause mortality was significantly higher in conservative group than in PCI group (34.9%vs. 15.3%; p=0.0072). Subsequently the survival curve started diverging with significantly higher mortality in conservative group. During the mid to long term follow up for 3.5±2.2 years (1 to 93 months) total mortality was 71.1% in conservative group and42.3% in PCI group (p=0.0004). Most deaths were noncardiac in both groups (54.3% vs. 68.2%; p=0.2516). Combination of infection, sepsis and AKI were the most important cause of death in both groups (54.8% vs.50%; p=0.6938).
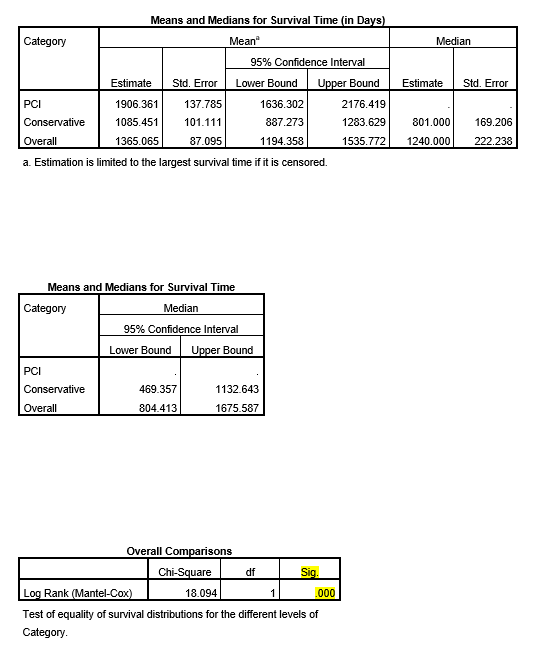
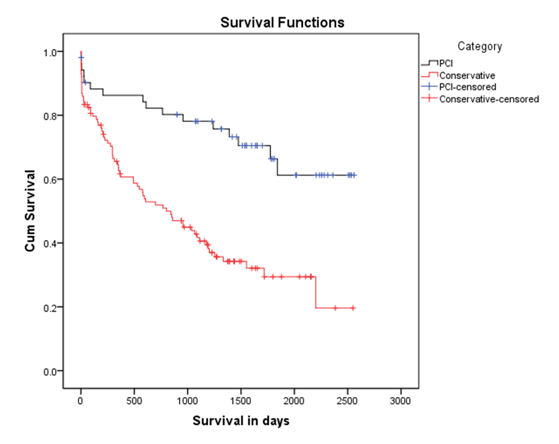
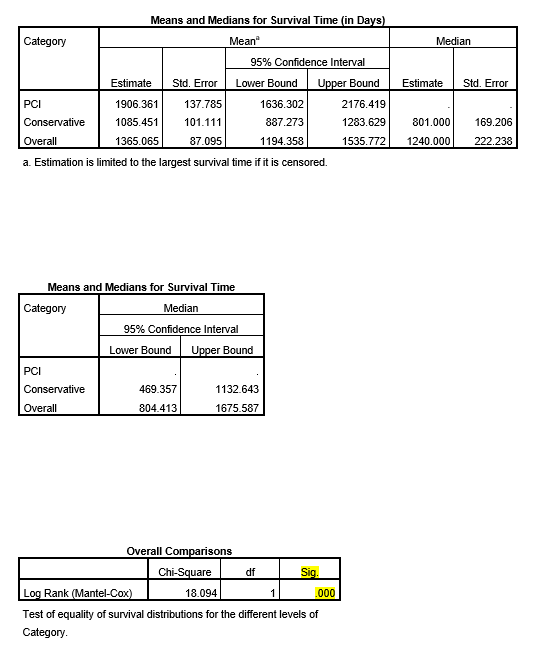
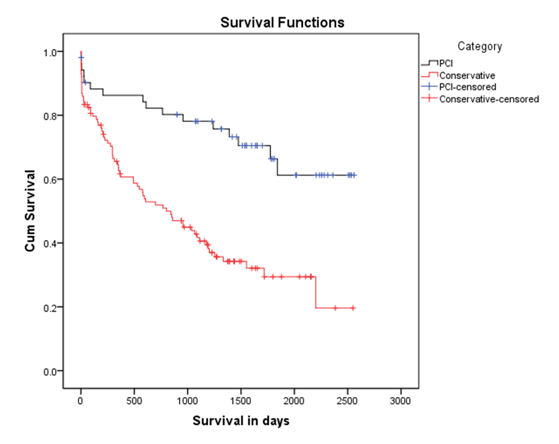
Conclusion
This retrospective cohort study shows that invasive strategy is safe and technically feasible treatment option in selected octogenarians which resulted in significant beneficial effects on long-term mortality. Patients in conservative group were older with more co-morbidities; this could probably explain the higher mortality in non-PCI group though it did not reflect in early mortality which was comparable. Besides, the mid-long term survival difference was markedly significant which was in favor of percutaneous coronary intervention. We conclude that percutaneous coronary intervention is a safe and effective treatment option for acute coronary syndrome in octogenarians and appears superior to conservative strategy resulting in improved survival and reduced early rehospitalizations.


