Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-057
Comparison of Intravascular Ultrasound and Two Dimensional Quantitative Coronary Angiography for the Measurement of Left Main Coronary Artery Diameter
By Mohamed Saad-Eddine Bouzghaia, Chakib Lamraoui, Khalil Lebcira
Presenter
Mohamed Saad-Eddine Bouzghaia
Authors
Mohamed Saad-Eddine Bouzghaia1, Chakib Lamraoui2, Khalil Lebcira2
Affiliation
Le Rameau d'Olivier Private Hospital, Algeria1, Universitary Hospital of Bejaia, Algeria2
View Study Report
TCTAP A-057
Imaging: Intravascular
Comparison of Intravascular Ultrasound and Two Dimensional Quantitative Coronary Angiography for the Measurement of Left Main Coronary Artery Diameter
Mohamed Saad-Eddine Bouzghaia1, Chakib Lamraoui2, Khalil Lebcira2
Le Rameau d'Olivier Private Hospital, Algeria1, Universitary Hospital of Bejaia, Algeria2
Background
Intravascular ultrasound (IVUS) is the gold standard for accurate measurements of left main coronary artery (LMCA) diameter.
Thus, it is the recommended imaging modality for percutaneous coronary intervention (PCI) guidance, including stent sizing and/or proximal optimisation technique balloon’s size.
However IVUS is not widely available, and angiography is still the most widely used imaging modality for LMCA PCI guidance.
Data regarding accuracy of angiography for LMCA diameter measurement are scarce.
Thus, it is the recommended imaging modality for percutaneous coronary intervention (PCI) guidance, including stent sizing and/or proximal optimisation technique balloon’s size.
However IVUS is not widely available, and angiography is still the most widely used imaging modality for LMCA PCI guidance.
Data regarding accuracy of angiography for LMCA diameter measurement are scarce.
Methods
We prospectively analysed angiographic and IVUS data of consecutive patients undergoing LMCA IVUS evaluation at the Universitary Hospital of Bejaia (Algeria) from April to August 2022.
Results
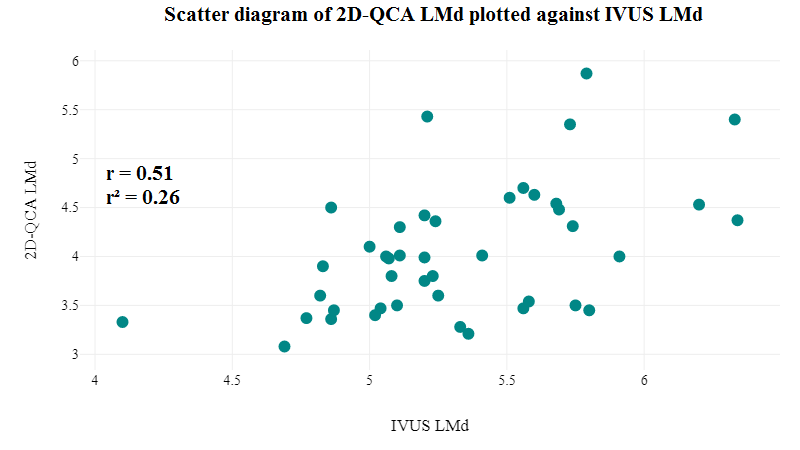
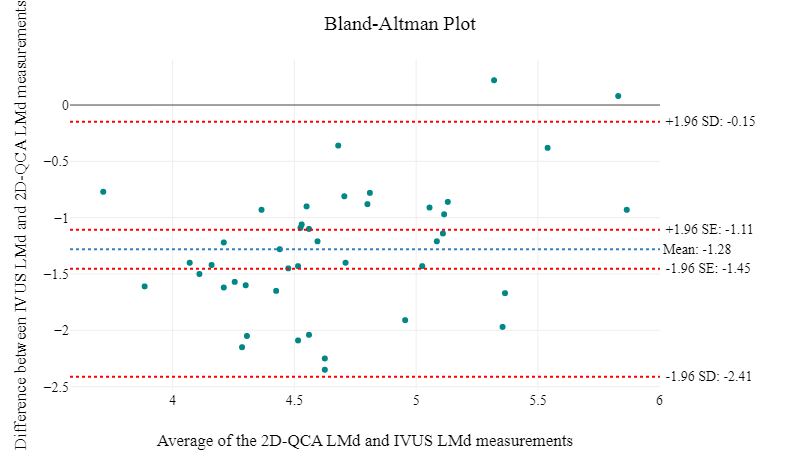
Forty-three patients’ data were obtained during the study period.
Table 1 : Comparison of LMCA diameters measured by IVUS and 2D-QCA
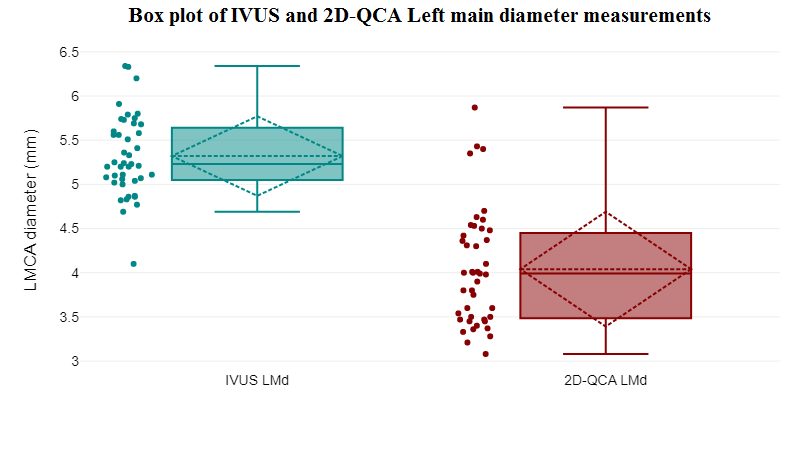
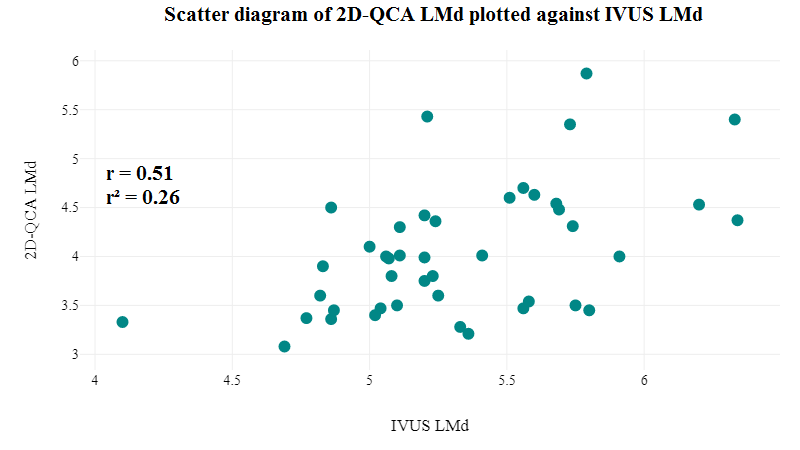
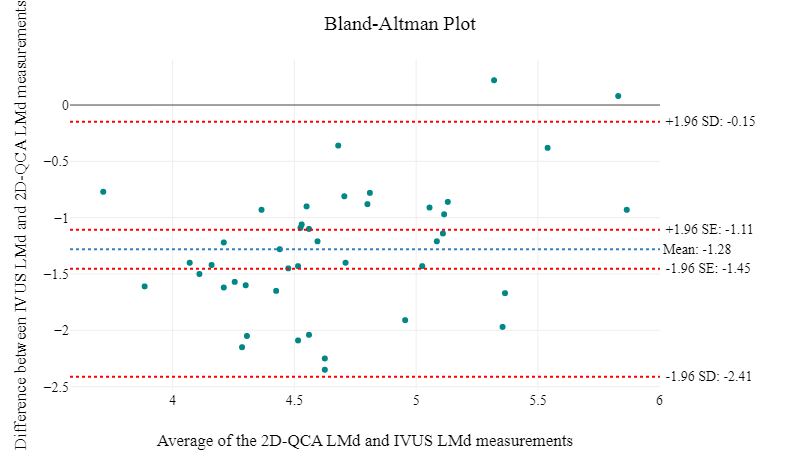
Table 1 : Comparison of LMCA diameters measured by IVUS and 2D-QCA
| | IVUS LMd (mm) | 2D-QCA LMd (mm) |
| Mean ± SD | 5.32 ± 0.46 | 4.04 ± 0.66 |
| Median | 5.23 | 3.99 |
| Minimum | 4.1 | 3.08 |
| Maximum | 6.34 | 5.87 |
Conclusion
Angiography derived left main coronary artery diameters measurements were significantly smaller than the gold standard IVUS measurements. Furthermore, correlation between the two measurements was only moderate, making any correction formula to cause a sizing error of more than 0.5 mm in 30% of patients in our study population. Hence, two dimensional angiography derived left main measures are not accurate enough to guide left main percutaneous coronary interventions and may result in inadequate stent and/or balloon sizing.


