Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-074
Long-Term Visit-To-Visit Glycemic Variability as a Predictor of Major Adverse Limb and Cardiovascular Events in Patients With Diabetes Mellitus
By Jung-Chi Hsu, Yen Yun Yang, Shulin Chuang, Lian-Yu Lin, Jen-Kuang Lee
Presenter
Jen-Kuang Lee
Authors
Jung-Chi Hsu1, Yen Yun Yang2, Shulin Chuang2, Lian-Yu Lin2, Jen-Kuang Lee2
Affiliation
National Taiwan University Hospital Jinshan Branch, Taiwan1, National Taiwan University Hospital, Taiwan2
View Study Report
TCTAP A-074
Diabetes
Long-Term Visit-To-Visit Glycemic Variability as a Predictor of Major Adverse Limb and Cardiovascular Events in Patients With Diabetes Mellitus
Jung-Chi Hsu1, Yen Yun Yang2, Shulin Chuang2, Lian-Yu Lin2, Jen-Kuang Lee2
National Taiwan University Hospital Jinshan Branch, Taiwan1, National Taiwan University Hospital, Taiwan2
Background
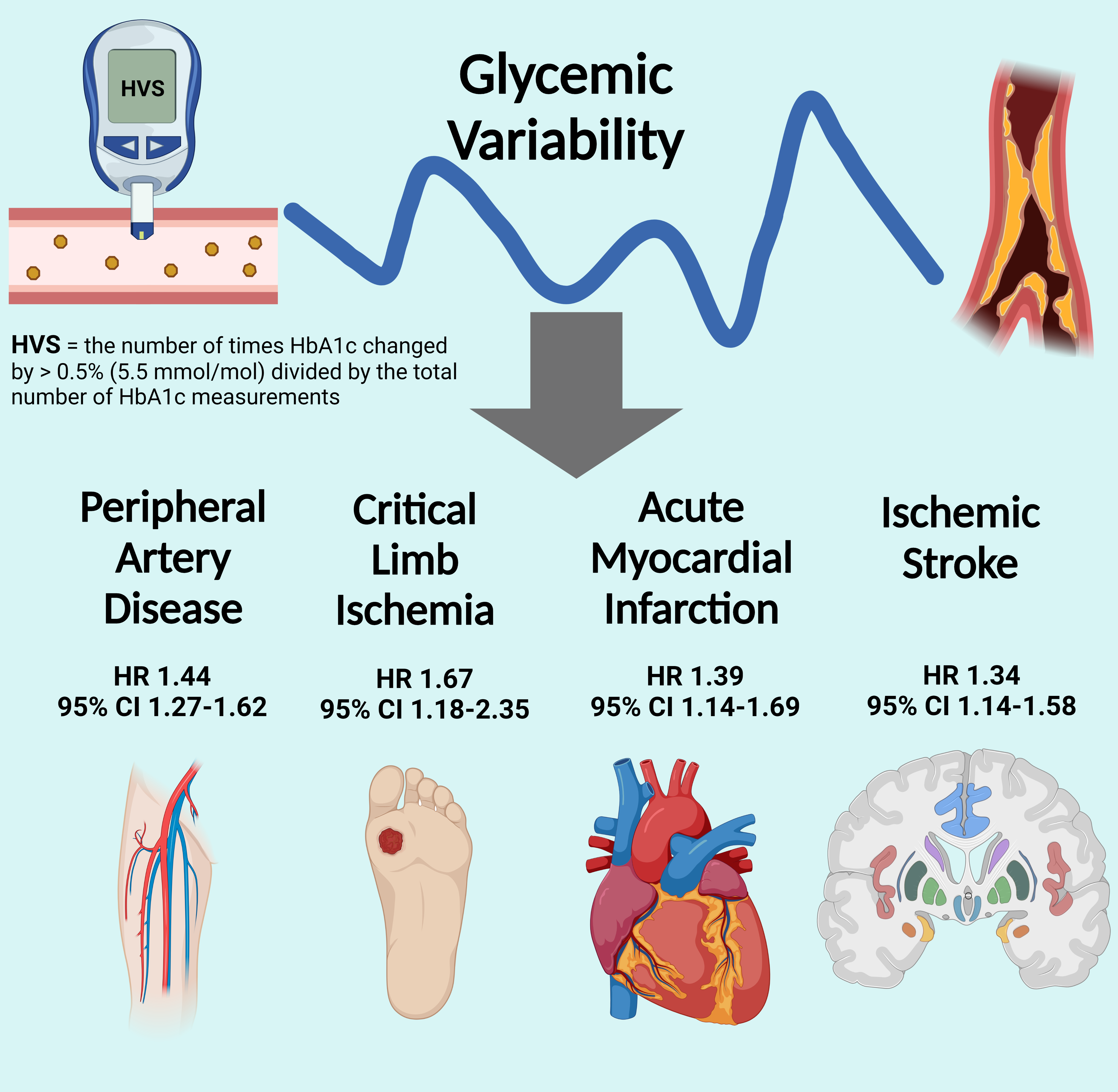
Peripheralarterial disease (PAD) is a severe complication in patients with type 2 diabetes mellitus (T2DM). Glycemic variability (GV) is associated with increased risks of developing microvascular and macrovascular diseases. However, few studies have focused on the association between GV and PAD.
Methods
This cohort study used a database maintained by the National Taiwan University Hospital, a tertiary medical center in Taiwan. For each individual, GV parameters were calculated, including fasting glucose coefficient of variability (FGCV) and HbA1c variability score (HVS). Multivariable Cox regression models were constructed to estimate the relationships between GV parameters and composite scores for major adverse limb events (MALEs) and major adverse cardiovascular events (MACEs).
Results
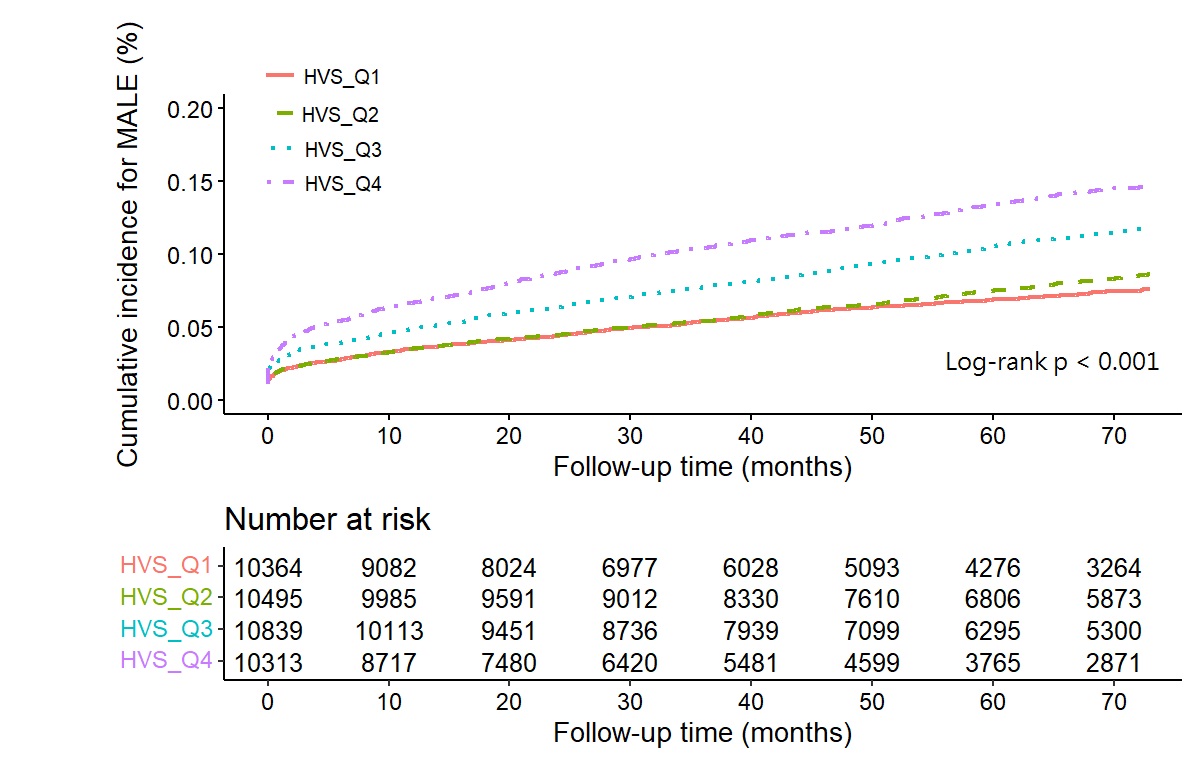
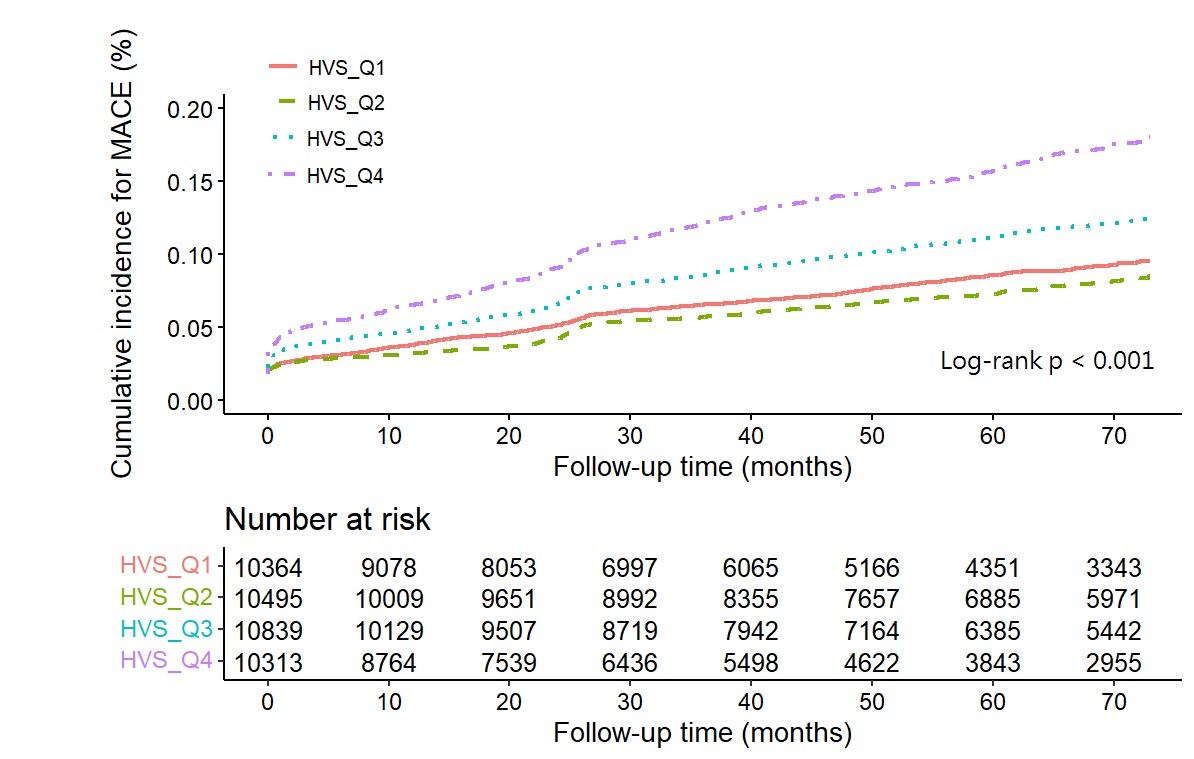
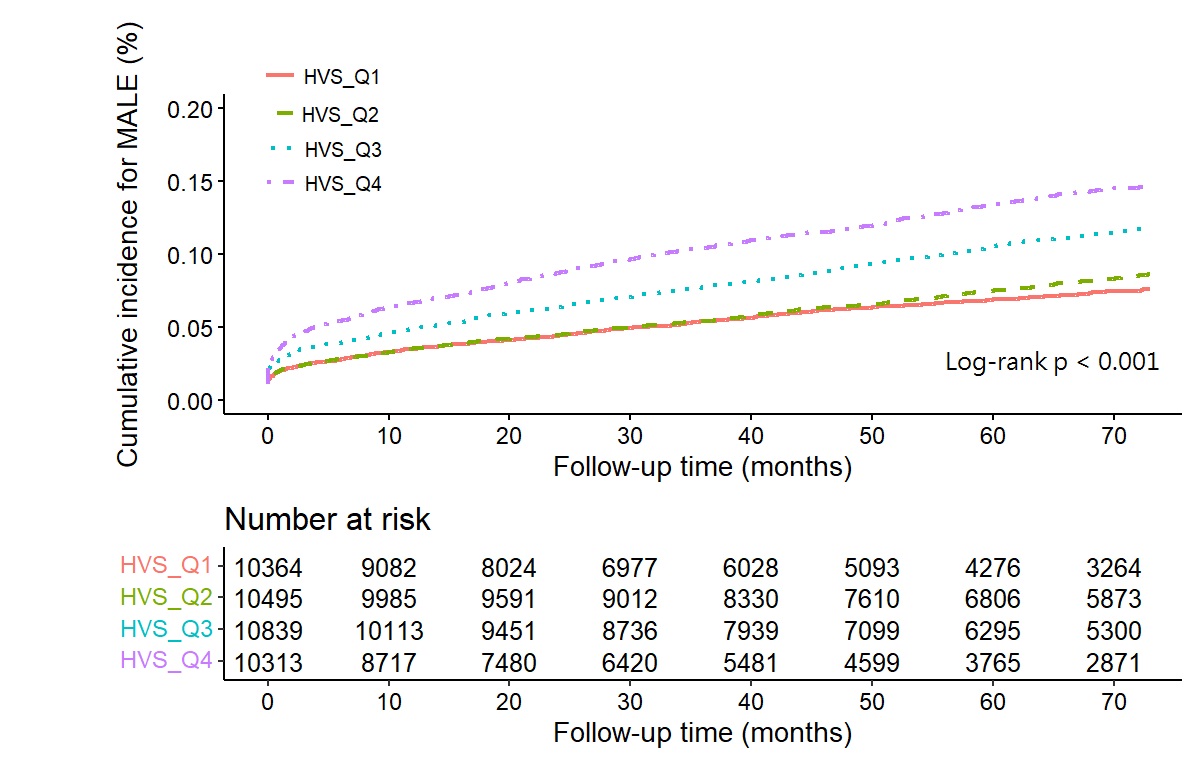
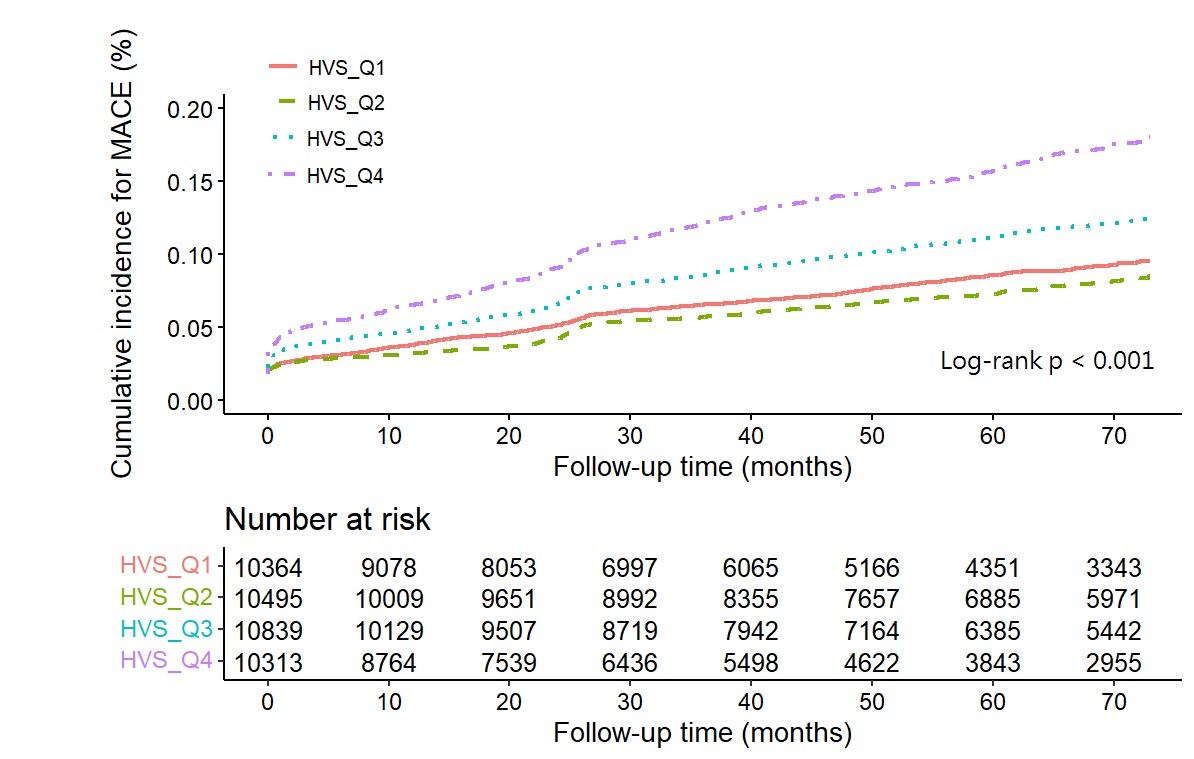
Between 2014 and 2019, a total of 45,436 adult patients with prevalent T2DM were enrolled for analysis, and GV was assessed during a median follow-up of 64.4 months. The average number of visits and time periods were 13.38 and 157.87 days for HVS group and 14.27 and 146.59 days for FGCV groups, respectively. The incidence rates for cardiac death, PAD, amputation, and critical limb ischemia (CLI) were 5.38, 20.11, 0.06, and 2.41 per 1000 person-years in FGCV groups and 5.35, 20.32, 0.07, and 2.50 per 1000 person-years in HVS groups, respectively. In the Cox regression model with full adjustment, the highest FGCV quartile was associated with significantly increased risks of MALEs (hazard ratio [HR]: 1.57, 95% confidence interval [CI]: 1.40–1.76, p < 0.001) and MACEs (HR: 1.40, 95% CI: 1.25–1.56, p < 0.001). Similarly, the highest HVS quartile was associated with significantly increased risks of MALEs (HR:1.44, 95% CI: 1.28–1.62, p < 0.001) and MACEs (HR: 1.28, 95% CI: 1.14–1.43,p < 0.001). The highest FGCV and HVS quartiles were both associated with the development of PAD and CLI (FGCV: PAD [HR: 1.57, p < 0.001], CLI [HR: 2.19,p < 0.001]; HVS: PAD [HR: 1.44, p < 0.001], CLI [HR: 1.67, p = 0.003]). The Kaplan–Meier analysis showed significantly higher risks of MALEs and MACEs with increasing GV magnitude (log-rank p < 0.001).
Conclusion
Among individuals with diabetes, increased GV is independently associated with the development of MALEs, including PAD and CLI, and MACEs. The benefit of maintaining stable glycemic levels for improving clinical outcomes warrants further studies.