Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-060
Intravascular Ultrasonography Guided Percuatneous Coronary Intervention with Everolimus-Eluting Stents or Bypass Surgery for Multivessel Coronary Artery Disease: Post-hoc Analysis of BEST Trial
By Jinho Lee, Hoyun Kim, Yeonwoo Choi, Do-Yoon Kang, Jung-Min Ahn, Duk-Woo Park, Seung-Jung Park
Presenter
Jinho Lee
Authors
Jinho Lee1, Hoyun Kim2, Yeonwoo Choi3, Do-Yoon Kang4, Jung-Min Ahn4, Duk-Woo Park4, Seung-Jung Park4
Affiliation
Kyung Hee University Medical Center, Korea (Republic of)1, Bucheon Sejong Hospital, Korea (Republic of)2, Changwon Hanmaeum Hospital, Korea (Republic of)3, Asan Medical Center, Korea (Republic of)4
View Study Report
TCTAP A-060
Imaging: Intravascular
Intravascular Ultrasonography Guided Percuatneous Coronary Intervention with Everolimus-Eluting Stents or Bypass Surgery for Multivessel Coronary Artery Disease: Post-hoc Analysis of BEST Trial
Jinho Lee1, Hoyun Kim2, Yeonwoo Choi3, Do-Yoon Kang4, Jung-Min Ahn4, Duk-Woo Park4, Seung-Jung Park4
Kyung Hee University Medical Center, Korea (Republic of)1, Bucheon Sejong Hospital, Korea (Republic of)2, Changwon Hanmaeum Hospital, Korea (Republic of)3, Asan Medical Center, Korea (Republic of)4
Background
TheLong-term outcome of Intravascular ultrasonography (IVUS) guided percutaneouscoronary intervention (PCI) with everolimus-eluting stent and coronary-arterybypass grafting (CABG) are limited in patients with multivessel coronary arterydisease
Methods
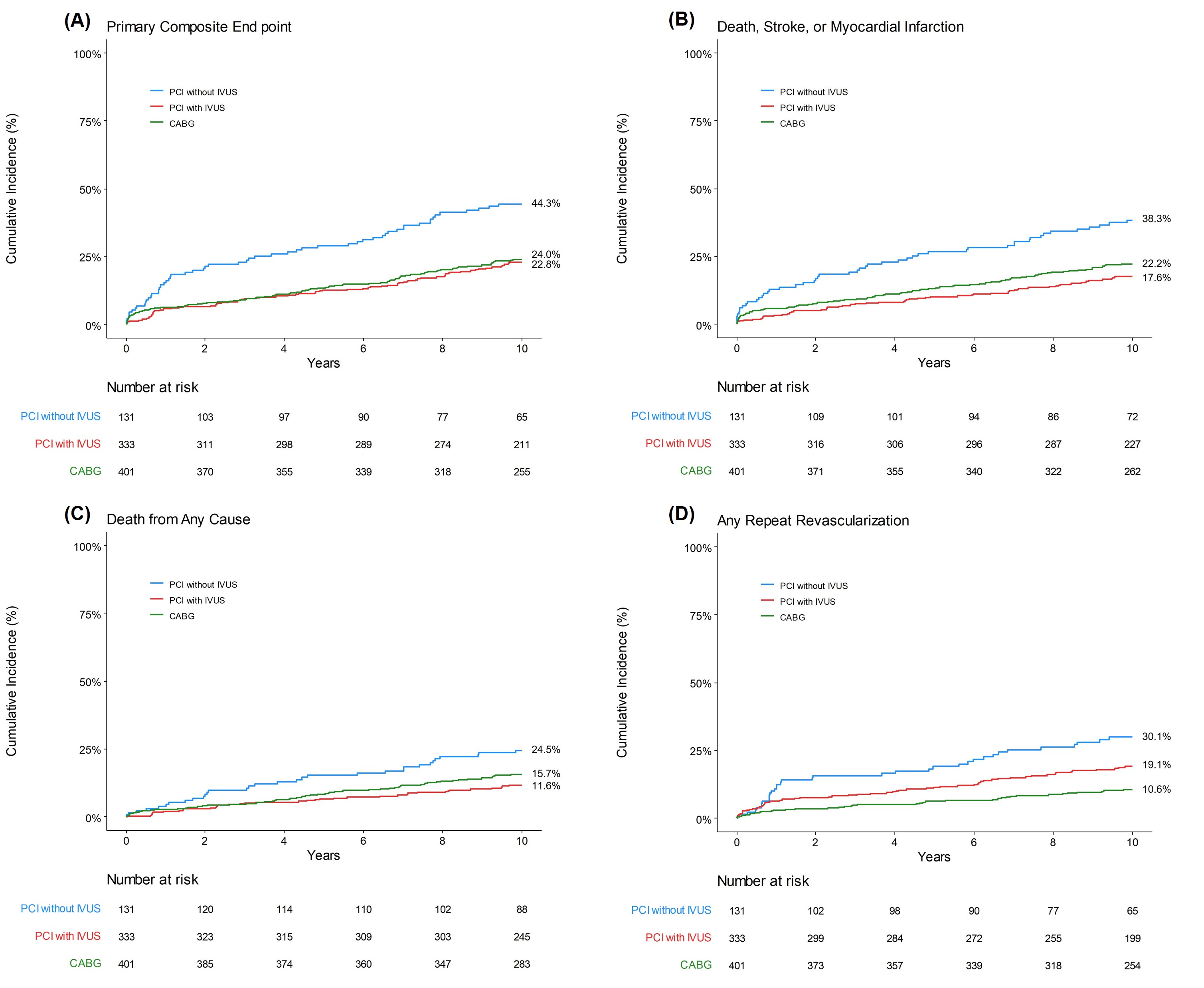
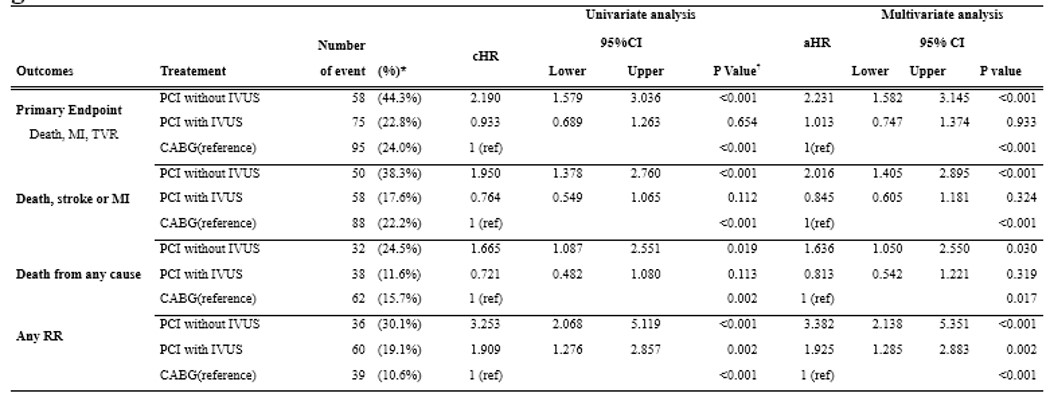
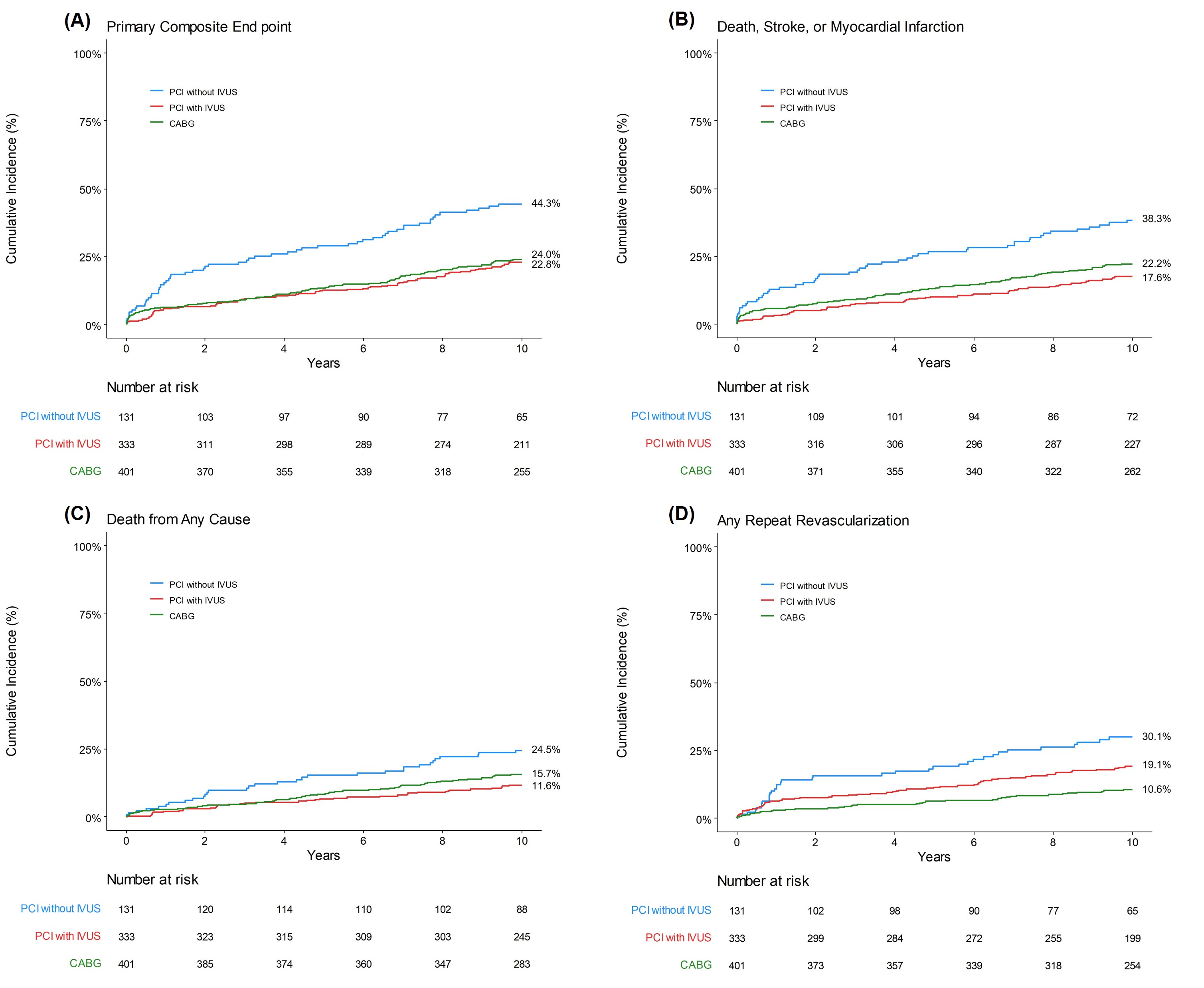
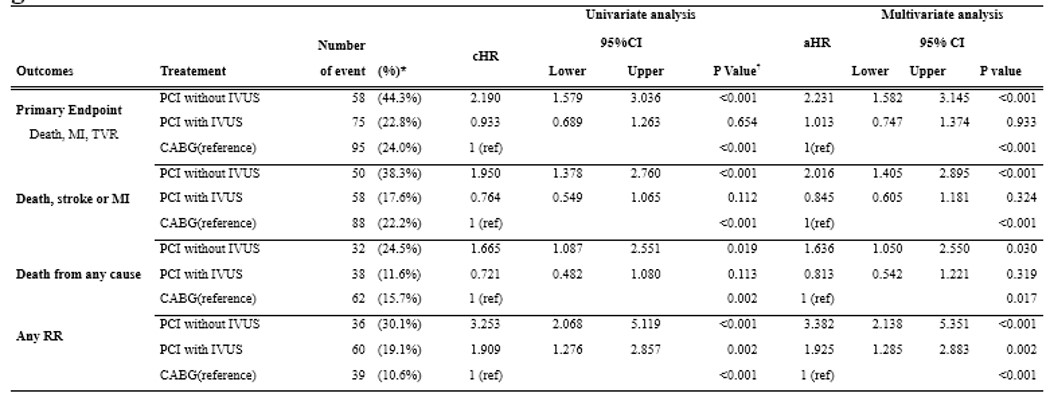
We analyzed patient data from BEST trial, randomlyassigned 880 patients with angiographic multivessel coronary artery disease toreceive PCI with everolimus-eluting stent or CABG between July 2008 andSeptember 2013. Post-hoc analysis divided patient data into IVUS guidance PCIor angiographic-guided PCI or received CABG. The primary end point was thecomposite of death from any cause, myocardial infarction, or target-vesselrevascularization.
Results
During a median follow-up of 11.8 years (interquartilerange, 10.6 to 12.5 years, the maximum of 13.7 years), the primary end point occurredin 58 patients (44.3%) in the PCI without IVUS group and 75 patients (22.8%) inthe PCI with IVUS group and 95 patients (24.0%) in the CABG group (adjusted hazardratio for PCI with IVUS as compared with the CABG group [aHR] 0.93; 95%confidence interval [CI], 0.74 to 1.13; P=0.93). IVUS-guided PCI group was similarrisk of composited of death, myocardial infarction, or stroke than CABG group (17.6%and 22.0%, aHR 0.84; 95% CI 0.60 to 1.18, P=0.32). However, any repeatrevascularization (19.1% and 10.6%. aHR 1.92; 95% CI 1.28 to 2.88, P = 0.002)were more frequent in IVUS-guided PCI than CABG group.
Conclusion
Inpatients with multivessel coronary artery disease, there were no significantdifferences between IVUS-guided PCI and CABG in the rates of major adversecardiac events compared with angiography-guided PCI with higher rate of majoradverse cardiac events. during an extended-follow-up of up to 14 years


