Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-101
Percutaneous Pulmonary Angioplasty or Medications for Takayasu Arteritis and Pulmonary Hypertension
By Yi-Ting Lu, Di Zhang, Wu Song, Jian-Yu Qu, Xian-Liang Zhou, Sheng Liu
Presenter
Yi-Ting Lu
Authors
Yi-Ting Lu1, Di Zhang1, Wu Song1, Jian-Yu Qu1, Xian-Liang Zhou1, Sheng Liu1
Affiliation
Fuwai Hospital, China1
View Study Report
TCTAP A-101
Pulmonary Intervention: CTEPH, PHTN
Percutaneous Pulmonary Angioplasty or Medications for Takayasu Arteritis and Pulmonary Hypertension
Yi-Ting Lu1, Di Zhang1, Wu Song1, Jian-Yu Qu1, Xian-Liang Zhou1, Sheng Liu1
Fuwai Hospital, China1
Background
Pulmonary artery involvement is not rare for patients with Takayasu arteritis (TA), however, the optimal treatment for patients with TA and pulmonary hypertension (TA-PH) remains unclear. This study aimed to evaluate whether percutaneous transluminal pulmonary angioplasty (PTPA) is associated with improved clinical outcomes for patients with TA-PH.
Methods
Consecutive patients diagnosed with TA and PH at a large referral cardiovascular center between January 2010 and April 2022 were included in this cohort study. Patients were managed with PTPA or medications alone at the discretion of patients and doctors and in accordance with local practice guidelines. The primary outcome was all cause mortality. Heart failure classified by New York Heart Association and measures of right heart function were also analyzed.
Results
Among 154 patients with TA-PH included in this analysis, 88 of them had PTPA and 66 received medical treatment. Baseline characteristics were similar between the PTPA group and the medication group. During a median follow-up time of 43.8 months, all-cause death occurred in 7 (8.0%) patients in PTPA group and 27 (40.9%) in the medication group (hazard ratio [HR], 0.15; 95% confidence interval [CI], 0.06-0.33; P<0.001). Patients received PTPA also had less severe heart failure symptoms and significantly improved right heart function. Four patients in the PTPA group had intraoperative hemoptysis and no perioperative death was observed.
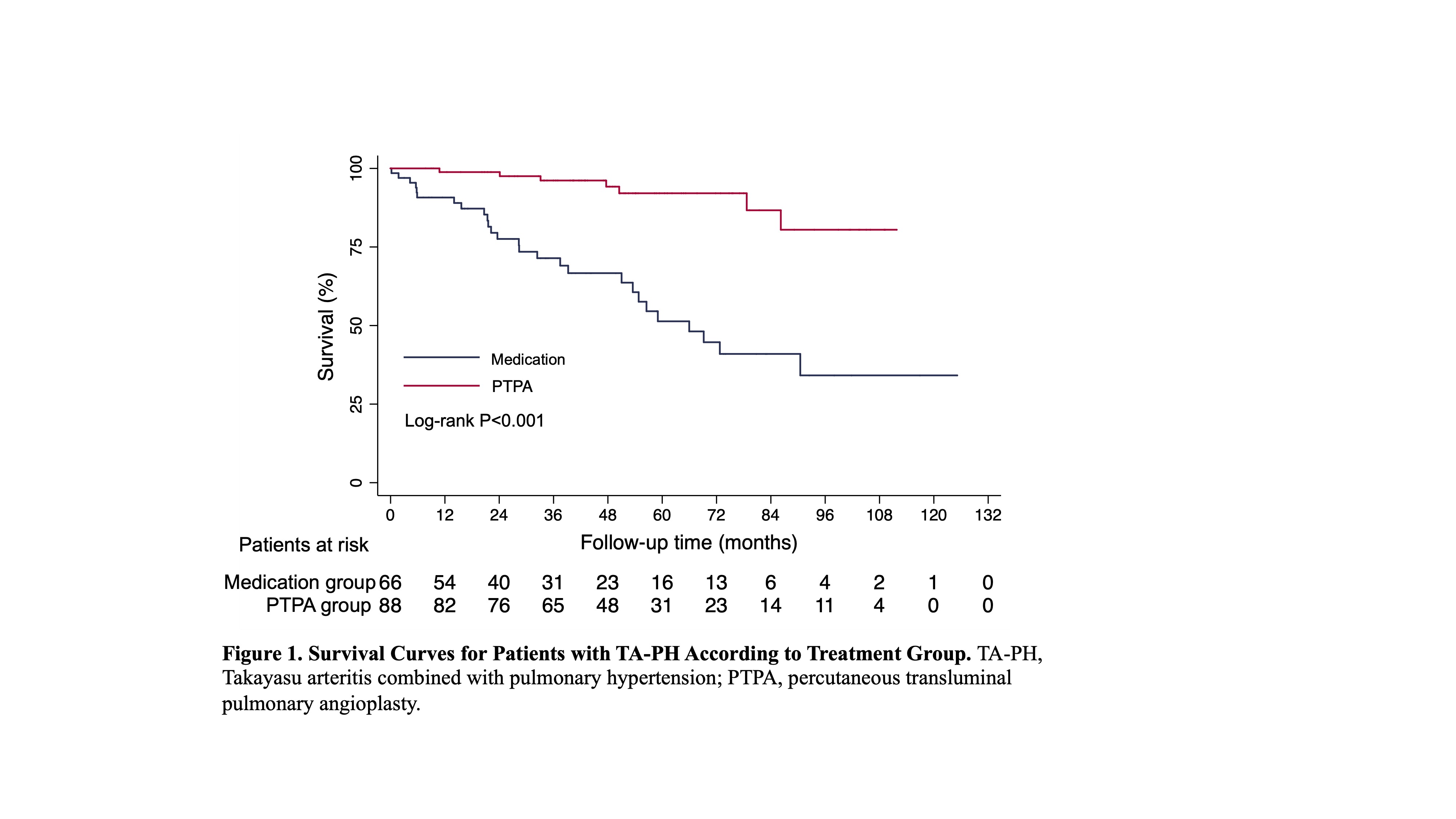
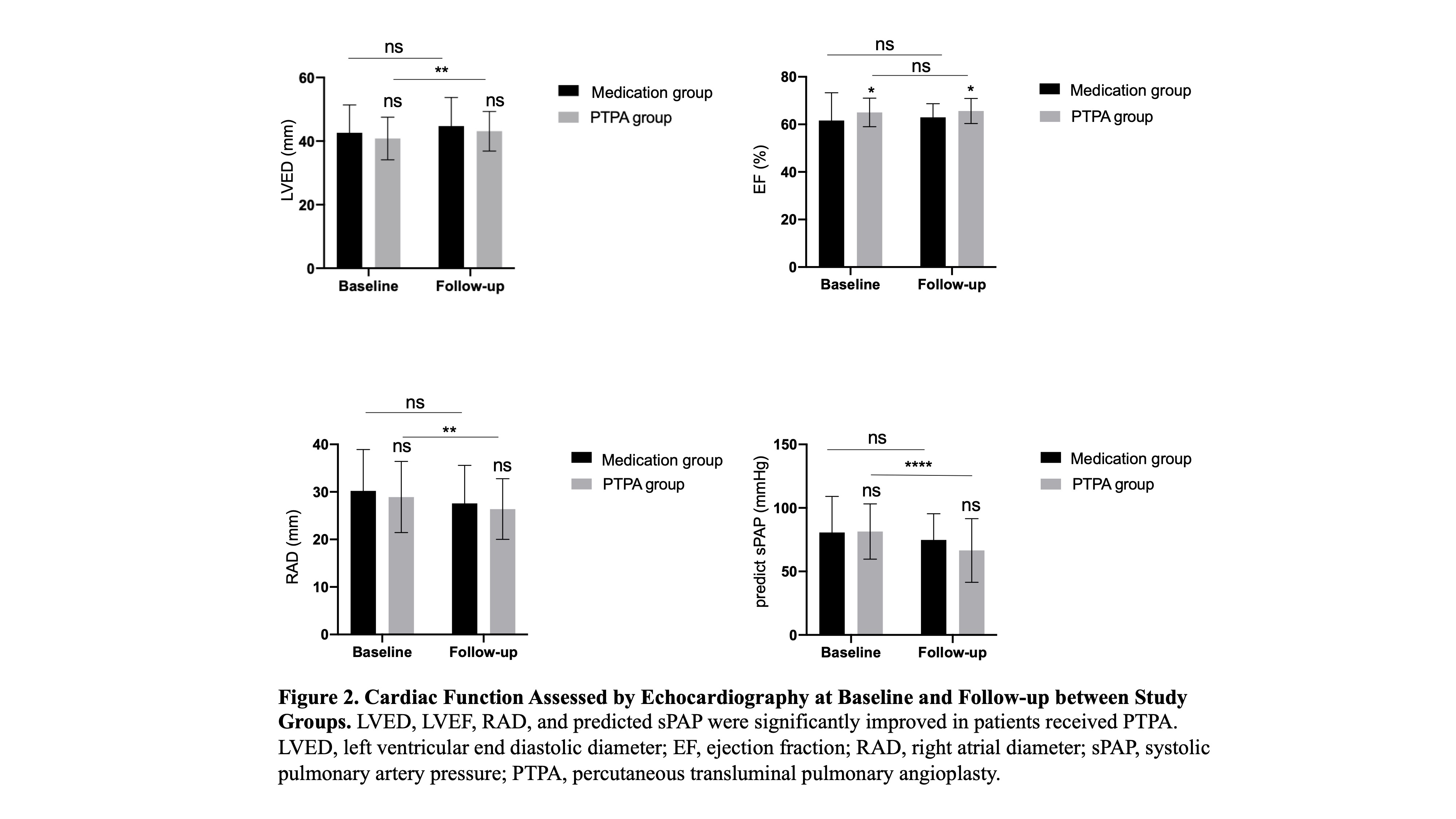
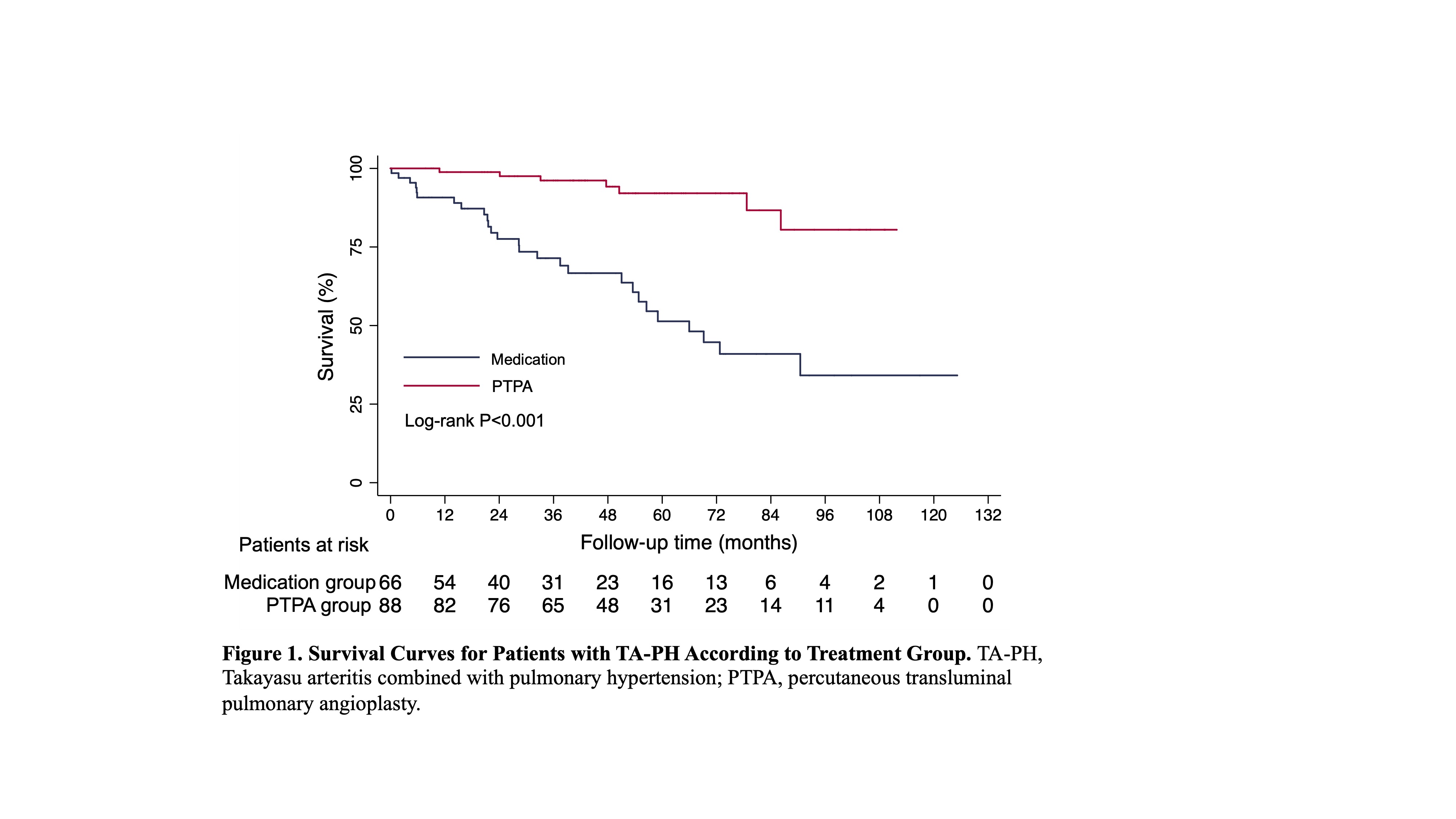
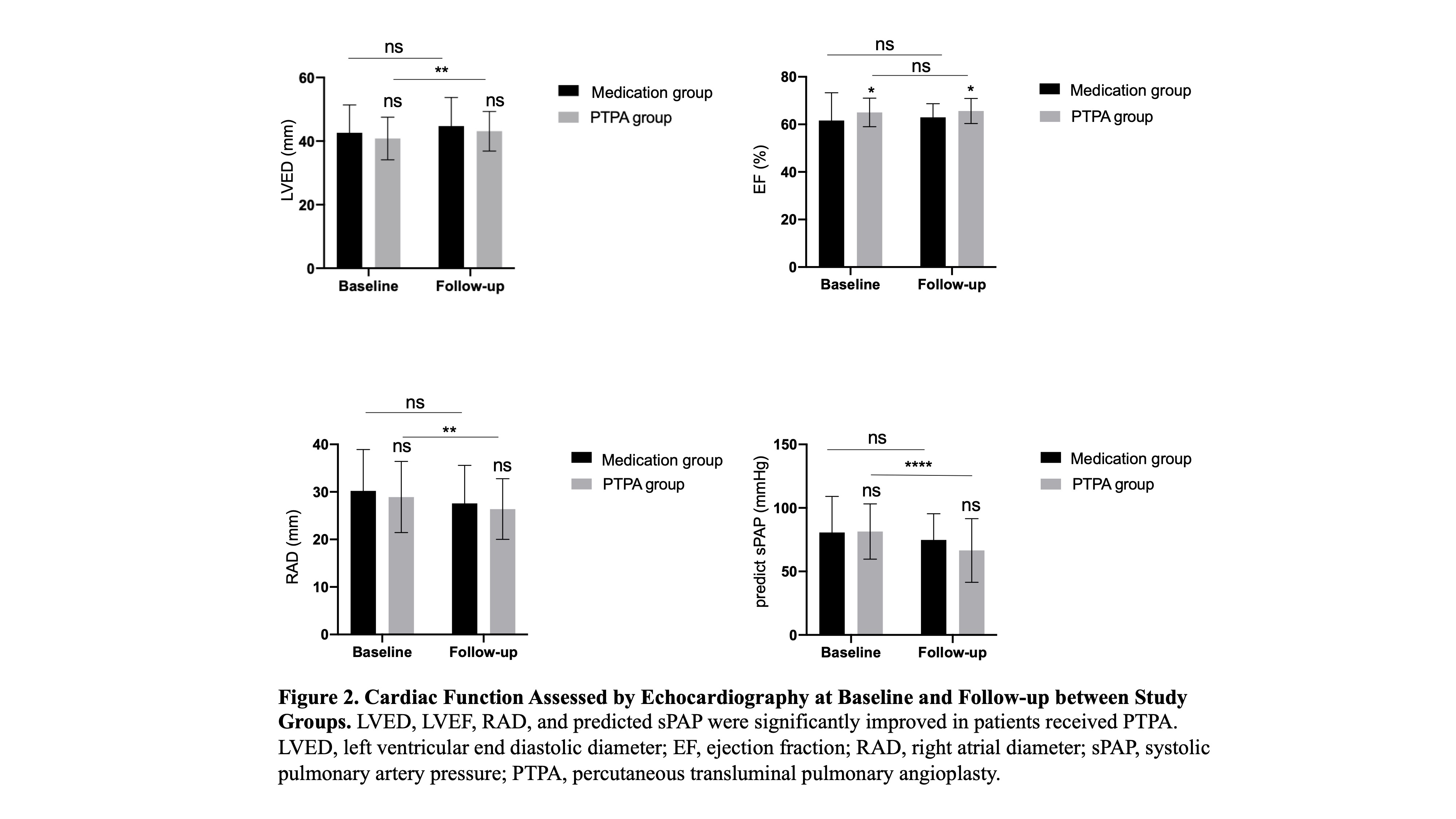
Conclusion
PTPA was associated with significantly reduced risk of death and improved heart function as compared with medication alone for patients with TA-PH. PTPA seemed to be a promising alteration for TA-PH patients.


