Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-104
Impact of High Implantation of Transcatheter Aortic Valve on Subsequent Conduction Disturbances and Coronary Access
By Tomoki Ochiai, Futoshi Yamanaka, Koki Shishido, Noriaki Moriyama, Shigeru Saito
Presenter
Tomoki Ochiai
Authors
Tomoki Ochiai1, Futoshi Yamanaka1, Koki Shishido1, Noriaki Moriyama1, Shigeru Saito1
Affiliation
Shonan Kamakura General Hospital, Japan1
View Study Report
TCTAP A-104
Valvular Intervention: Aortic
Impact of High Implantation of Transcatheter Aortic Valve on Subsequent Conduction Disturbances and Coronary Access
Tomoki Ochiai1, Futoshi Yamanaka1, Koki Shishido1, Noriaki Moriyama1, Shigeru Saito1
Shonan Kamakura General Hospital, Japan1
Background
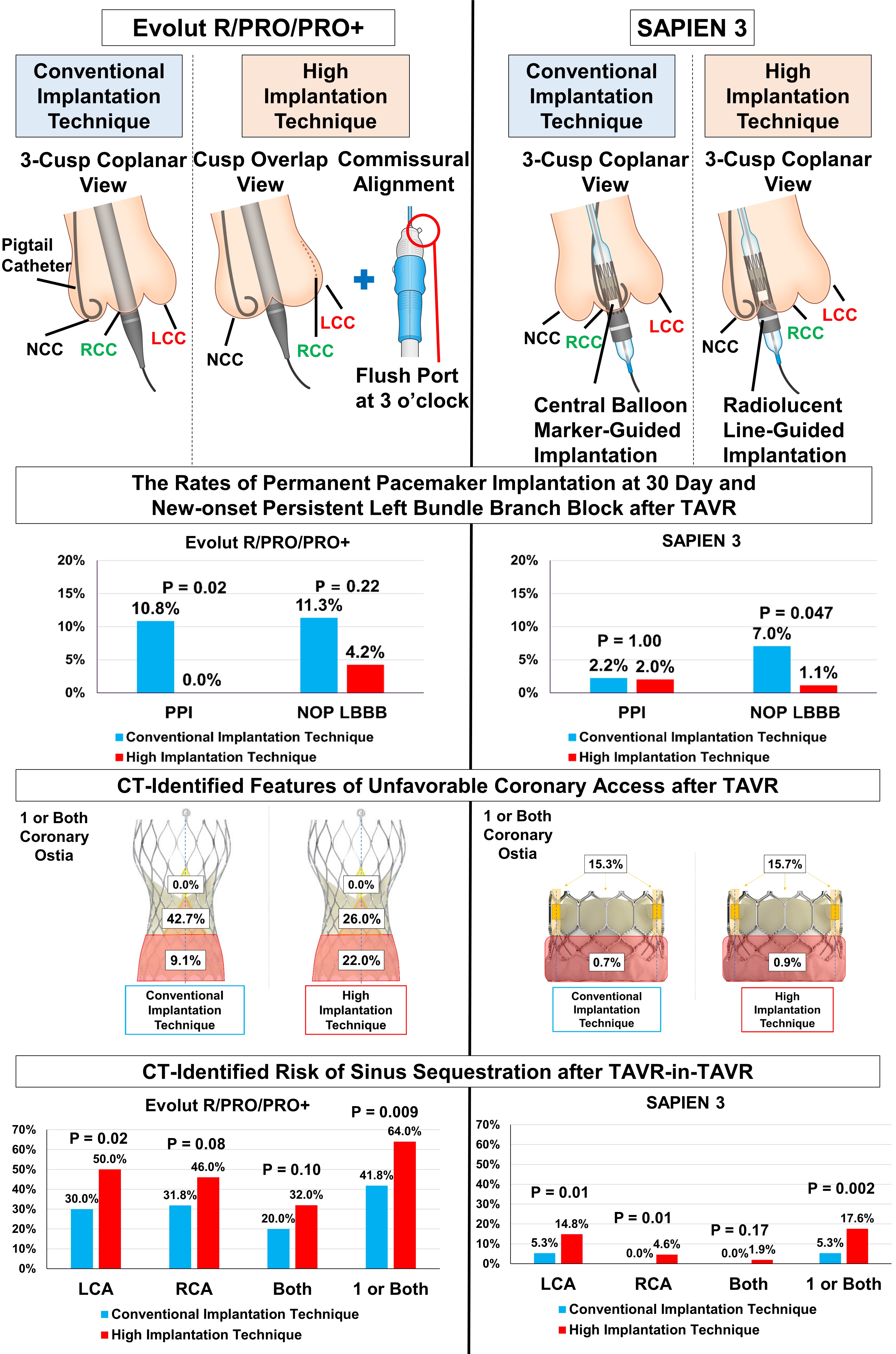
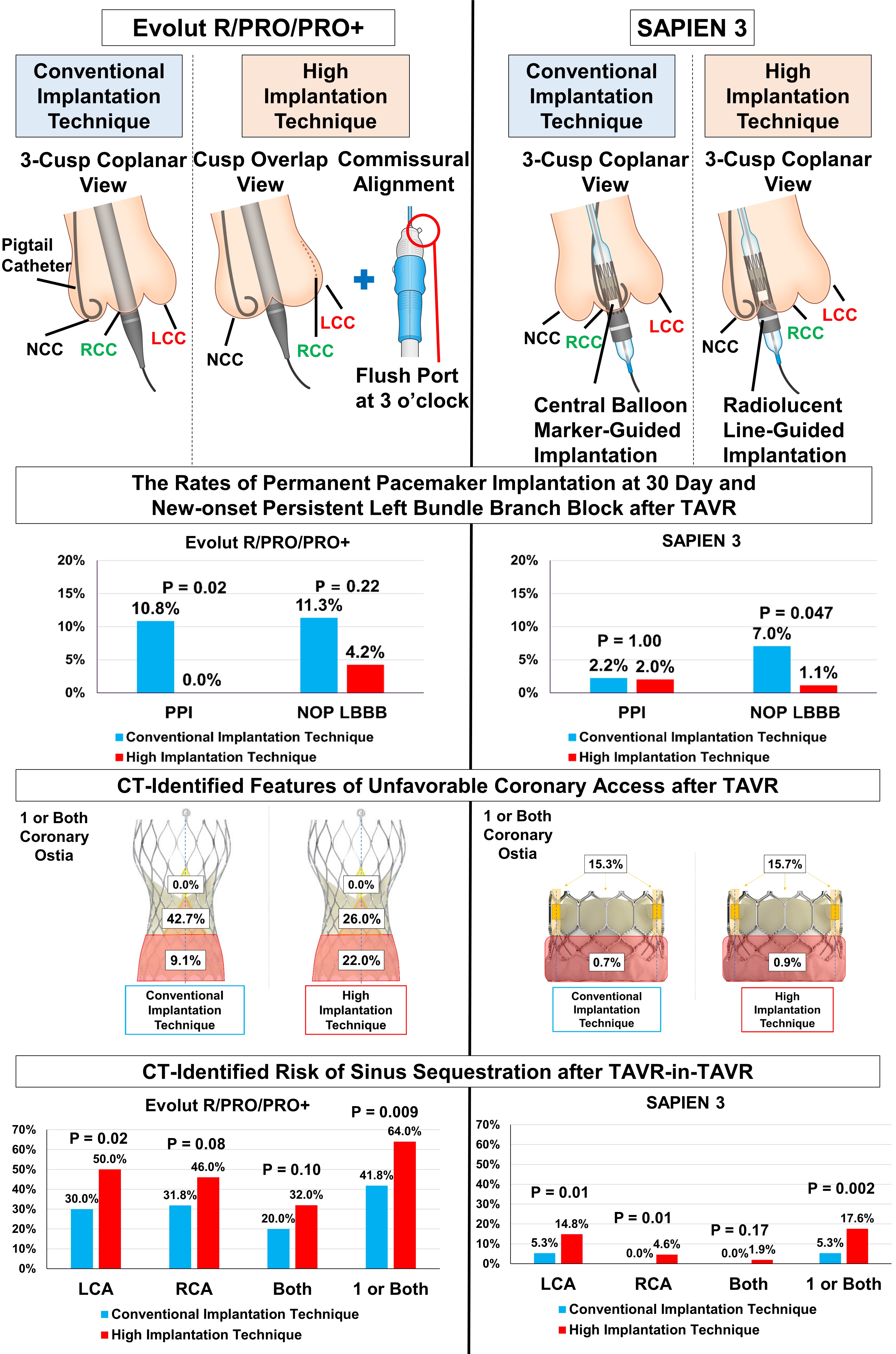
The cusp-overlap and commissural alignment techniques in the Evolut R/PRO/PRO+ and radiolucent line-guided implantation technique in the SAPIEN 3 were introduced to achieve high transcatheter heart valve (THV) implantation during transcatheter aortic valve replacement (TAVR). The aim of this study was to assess the impact of high THV implantation on conduction disturbances and coronary access after TAVR.
Methods
We included 160 and 258 patients who underwent TAVR for severe aortic stenosis with Evolut R/PRO/PRO+ and SAPIEN 3 THVs, respectively. In each group, the incidence of new conduction disturbances was compared between the conventional implantation technique (CIT) and high implantation technique (HIT) groups. All patients underwent post-TAVR computed tomography (CT) to analyze coronary accessibility.
Results
In the Evolut R/PRO/PRO+ group, the 30-day permanent pacemaker implantation (PPI) rate was significantly lower in the HIT group than in the CIT group (0.0% vs. 10.8%, p=0.02), whereas new-onset persistent left bundle branch block (NOP LBBB) rate was similar between two groups (4.2% vs. 11.3%, p=0.22). In the SAPIEN 3 group, the 30-day PPI rate was similar between two groups (2.0% vs. 2.2%, p=1.00), whereas the NOP LBBB rate was significantly lower in the HIT than in the CIT group (1.1% vs. 7.0%, p=0.047). In the Evolut R/PRO/PRO+ group, post-TAVR CT showed that the HIT group had a higher incidence of one or both coronary ostia overlap with the THV skirt (22.0% vs. 9.1%, p=0.03) and a lower incidence of one or both coronary ostia overlap with the THV commissural posts (26.0% vs. 42.7%, p=0.04) compared with CIT group. These incidences were similar between the CIT and HIT groups in the SAPIEN 3 group. In both THVs, CT-identified risk of sinus sequestration after TAVR-in-TAVR was significantly higher in the HIT group than in the CIT group (Evolut R/PRO/PRO+ group: 64.0% vs. 41.8%, p=0.009; SAPIEN 3 group: 17.6% vs. 5.3%, p=0.002).
Conclusion
High THV implantation substantially reduced conduction disturbances after TAVR. However, post-TAVR CT revealed the risk for unfavorable future coronary access. Patient-specific THV implantation depth and commissural alignment should be considered to balance the risks of conduction disturbances and unfavorable coronary access after TAVR.