Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-041
The Outcome of Percutaneous Coronary Intervention in Bangladeshi Patients With Low Left Ventricular Ejection Fraction
By Fazila Tun-Nesa Malik, Md Kalimuddin, Nazir Ahmed, Mohammad Badiuzzaman, Ashok Kumar Dutta, Dhiman Banik, Habibur Rahman, Tawfiq Shahriar Huq, Nazmun Laila
Presenter
Nazmun Laila
Authors
Fazila Tun-Nesa Malik1, Md Kalimuddin1, Nazir Ahmed1, Mohammad Badiuzzaman1, Ashok Kumar Dutta1, Dhiman Banik1, Habibur Rahman1, Tawfiq Shahriar Huq1, Nazmun Laila1
Affiliation
National Heart Foundation Hospital & Research Institute, Bangladesh1
View Study Report
TCTAP A-041
Complex and Higher Risk Procedures for Indicated Patients (CHIP)
The Outcome of Percutaneous Coronary Intervention in Bangladeshi Patients With Low Left Ventricular Ejection Fraction
Fazila Tun-Nesa Malik1, Md Kalimuddin1, Nazir Ahmed1, Mohammad Badiuzzaman1, Ashok Kumar Dutta1, Dhiman Banik1, Habibur Rahman1, Tawfiq Shahriar Huq1, Nazmun Laila1
National Heart Foundation Hospital & Research Institute, Bangladesh1
Background
One of the most neglected groups of research involvinginterventional cardiology is patients with severe left ventricular dysfunction(LVD). The incidence ofsystolic myocardial dysfunction is increasing among patients with coronaryartery disease (CAD). Left ventricular ejection fraction (LVEF) representsone of the strongest predictors of cardiovascular events in patients with CAD.Patients with severe LVD were frequently older with more co-morbid conditions,may be unable to tolerate the hemodynamic effects and contrast load of long andcomplex procedures, and often have CAD that is harder to treat with increasedfrequency of chronic total occlusions, multi-vessel disease, and diffusedisease. Patients with severe ischemic LVD are associated with highermorbidity, an increased risk of sudden death, Poor quality of life, and frequentre-hospitalization for heart failure. There is limited dataregarding short- and long-term outcomes of patients with severe LVD undergoingpercutaneous coronary intervention (PCI) worldwide. The aim of the study was toevaluate the clinical outcome of patients with low LVEF undergoing PCI.
Methods
Data of this retrospectivestudy was collected from National Heart Foundation Hospital & ResearchInstitute PCI database. All information was gathered from January2015 to July 2022, on patients who underwent PCI. Patients were eligible forenrollment if they had a left ventricular ejection fraction of 35% or less (asassessed by echocardiography); which was considered as low LVEF. Patients withST-elevation myocardial infarction (STEMI), Non-ST elevation myocardialinfarction (NSTEMI), unstable angina and chronic coronary syndrome wereincluded in this study. All procedures were performed without mechanicalcirculatory support. Furosemide was given intravenously or through an infusionpump when required. Adrenaline was given intracoronary when it was required. Majoradverse cardiac events (MACE) were all-cause mortality, myocardial infarction,revascularization, and heart failure requiring hospitalization. Continuous variables were described using the mean and standarddeviation (SD) anddiscrete variables were expressed as numberof cases and percentage. Allanalyses were performed using SPSS statistical software version 16.0 (SPSSInc., Chicago, IL, USA). All patients underwent telephonic follow-up in September2022.
Results
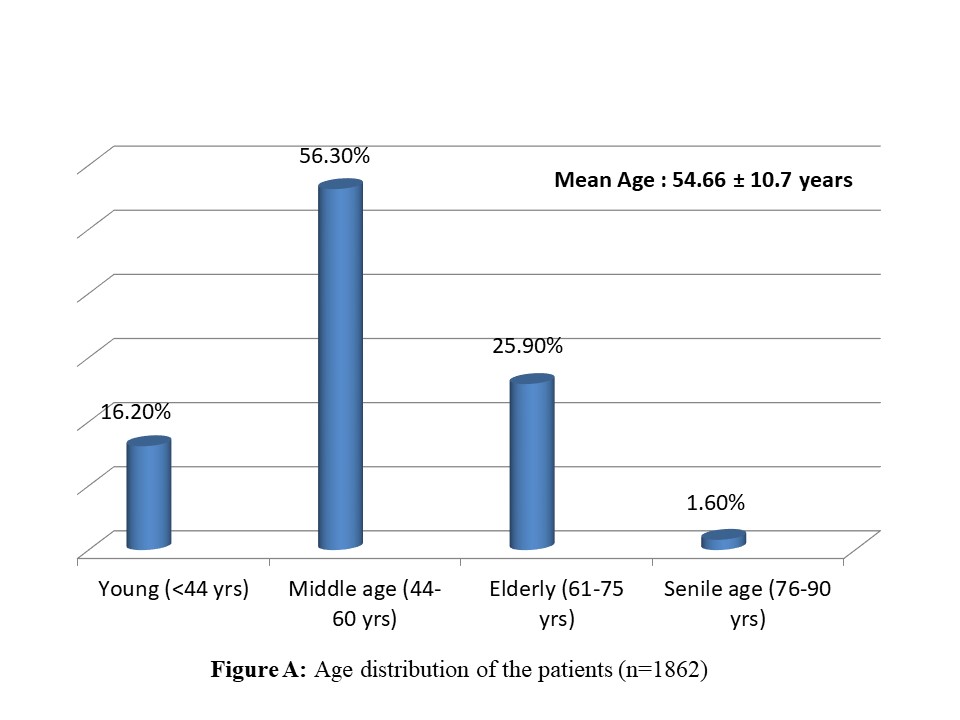
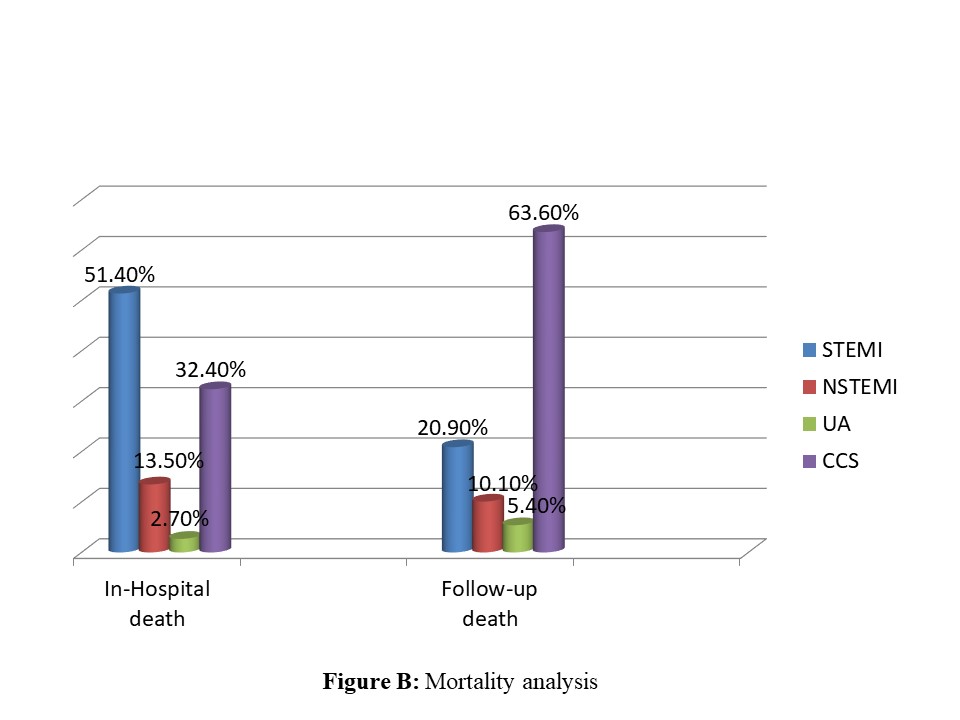
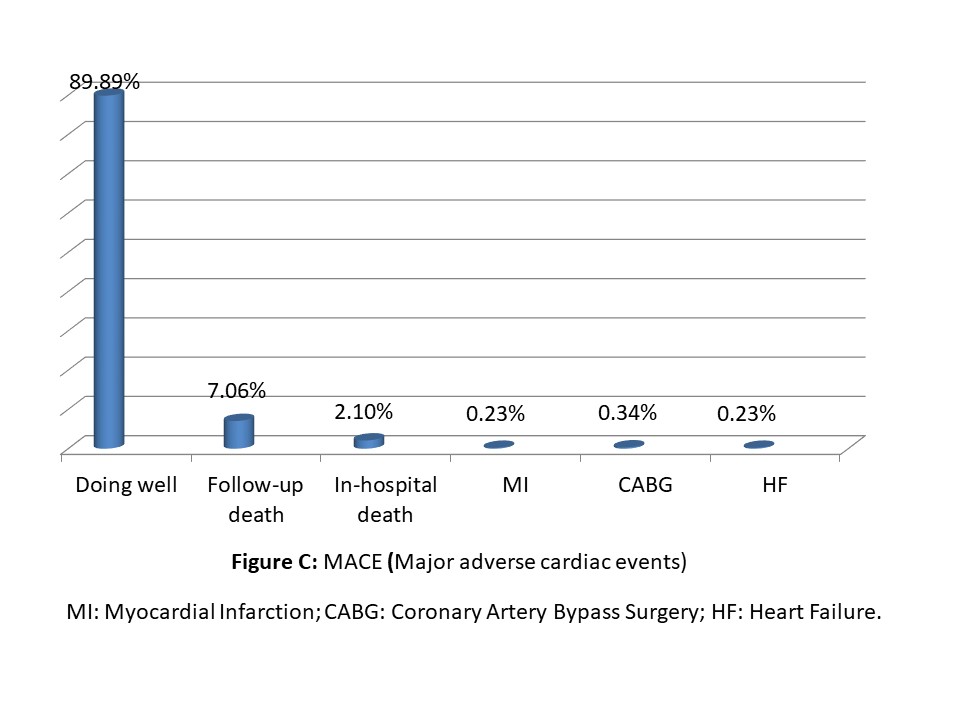
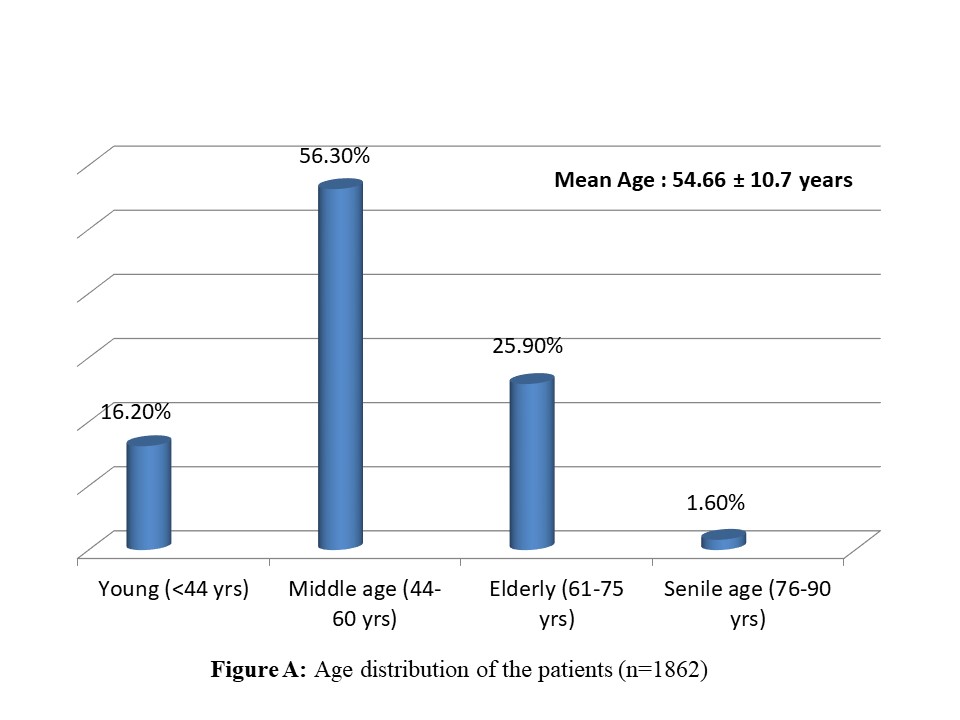
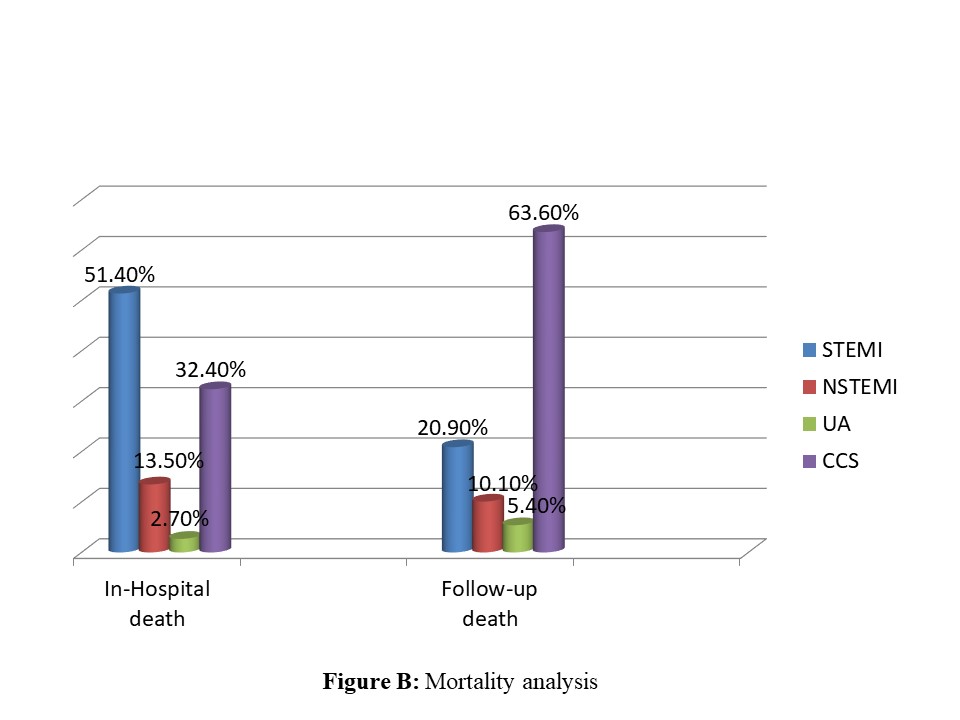
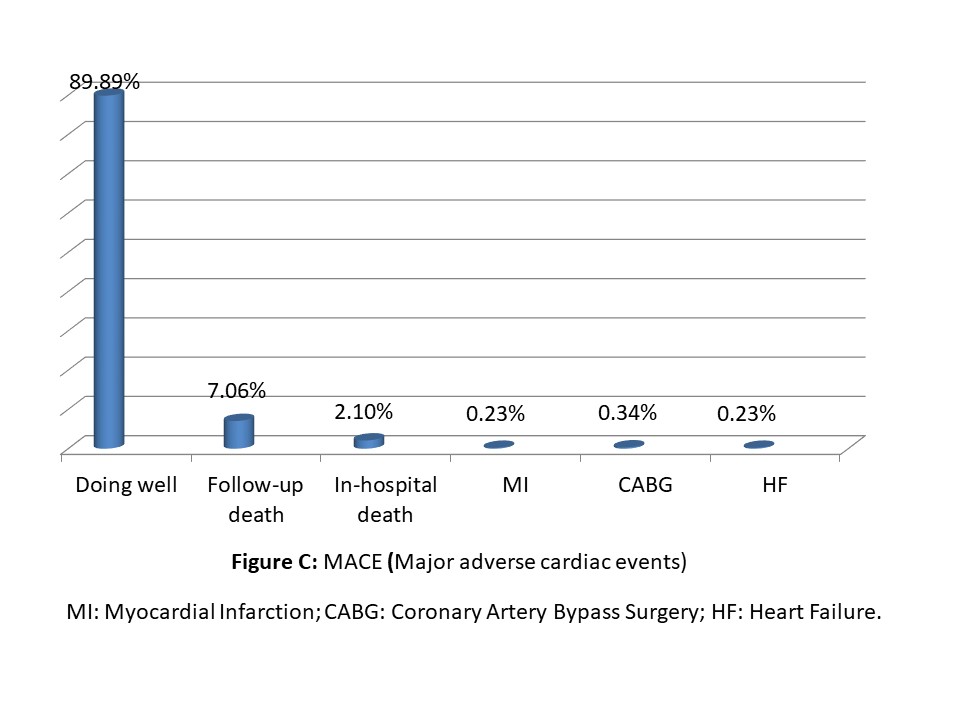
A total of 1862 patients were included in thisstudy. The mean age of the patients was 54.66 ± 10.7 years (Figure A) and 88.7%of the patients were male. Hypertension (70.2%) was the most common risk factorfollowed by dyslipidemia (55.5%), DM (52.7%), smoking (49.7%), and obesity(36.1%). CKD was the most common co-morbidity (49.7%) and 22.6% of the patientshad a prior myocardial infarction. Most of the patients (63.8%) were diagnosed aschronic coronary syndrome (CCS) and the remaining were patients with acute coronarysyndrome. The mean LVEF was 32.63 ± 2.7%. Single vessel disease was present in52.4% of patients, double vessel disease in 41.1% of patients, triple vesseldisease in 6.5% of patients, and11.7% of patients had left main disease. About1.8% of patients underwent staged PCI and 1.2% of patients rotablation. Chronictotal occlusion was present in 7.7% of patients. In-hospital mortality was2.1%. The median follow-up was 22 months. Follow-up death was 7.06%. The in-hospital mortality rate was higher in patients with STEMI and follow-up death was higherin patients with CCS (Figure B). Overall MACE was 10.11% (Figure C).
Conclusion
Data regarding outcomes of PCI or CABG or optimal medicaltherapy in patients with severe LV systolic dysfunction in Bangladesh arelacking. Overall mortality is comparable to other studies. Our studyshowed good clinical outcomes in patients with severe LV systolic dysfunctionwho underwent PCI. PCI may be encouraged in patients with low LVEF.


