Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-088
Validation of ARC-HBR Criteria for Patients Undergoing Percutaneous Coronary Intervention in Thai Population
By Donluck Poonkasem, Krissada Meemook
Presenter
Donluck Poonkasem
Authors
Donluck Poonkasem1, Krissada Meemook2
Affiliation
Vibharam Hospital, Thailand1, Ramathibodi Hospital Mahidol University, Thailand2
View Study Report
TCTAP A-088
Quality, Guidelines and Appropriateness Criteria
Validation of ARC-HBR Criteria for Patients Undergoing Percutaneous Coronary Intervention in Thai Population
Donluck Poonkasem1, Krissada Meemook2
Vibharam Hospital, Thailand1, Ramathibodi Hospital Mahidol University, Thailand2
Background
Recognizing a lack of consensus definition used in identifying patients at high bleeding risk undergoing percutaneous coronary intervention (PCI), the Academic Research Consortium for High Bleeding Risk (ARC-HBR) published a new set of criteria to define this population in 2019. This study aims to validate this new definition for its risk screening capability in Thai population.
Methods
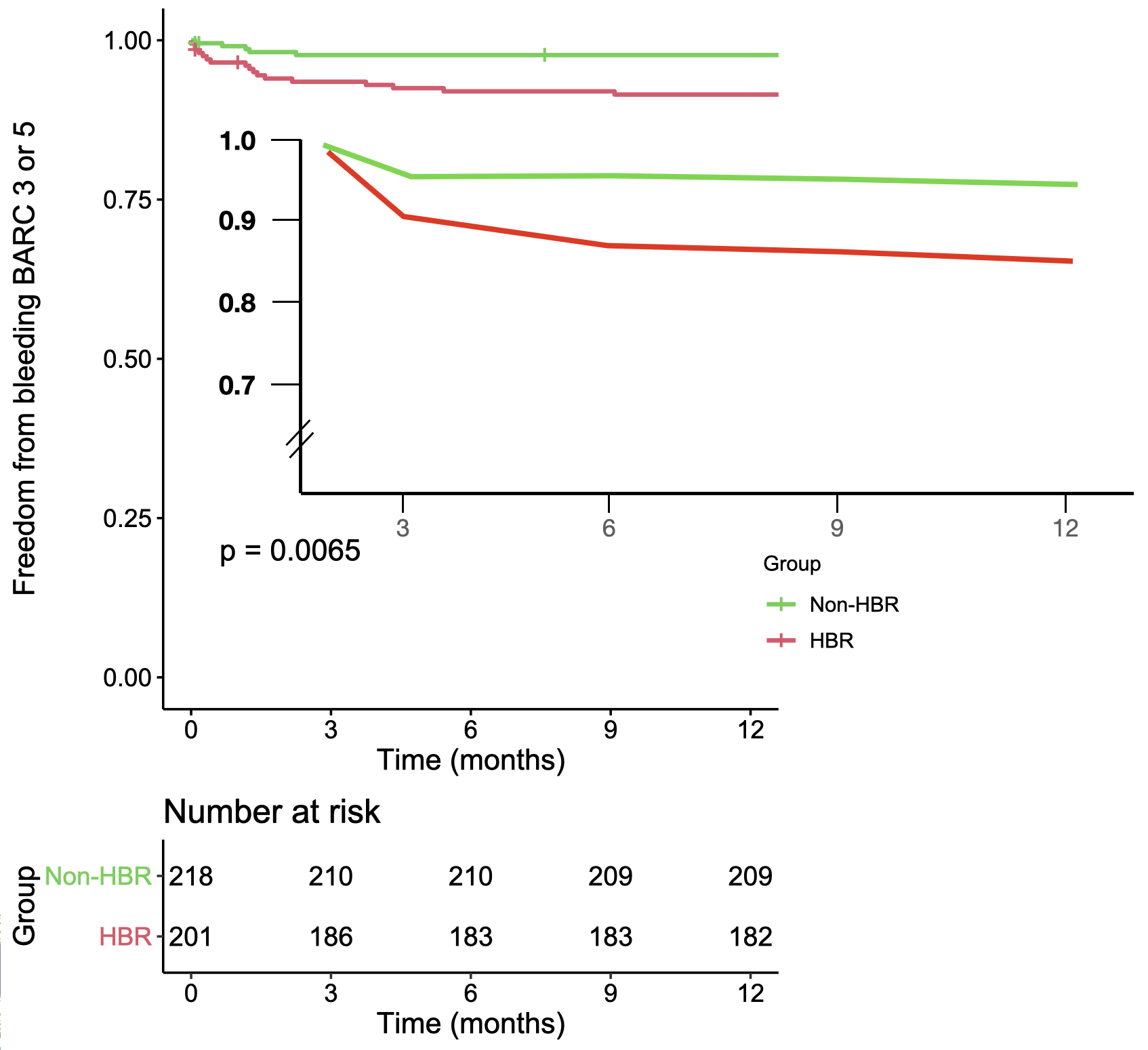
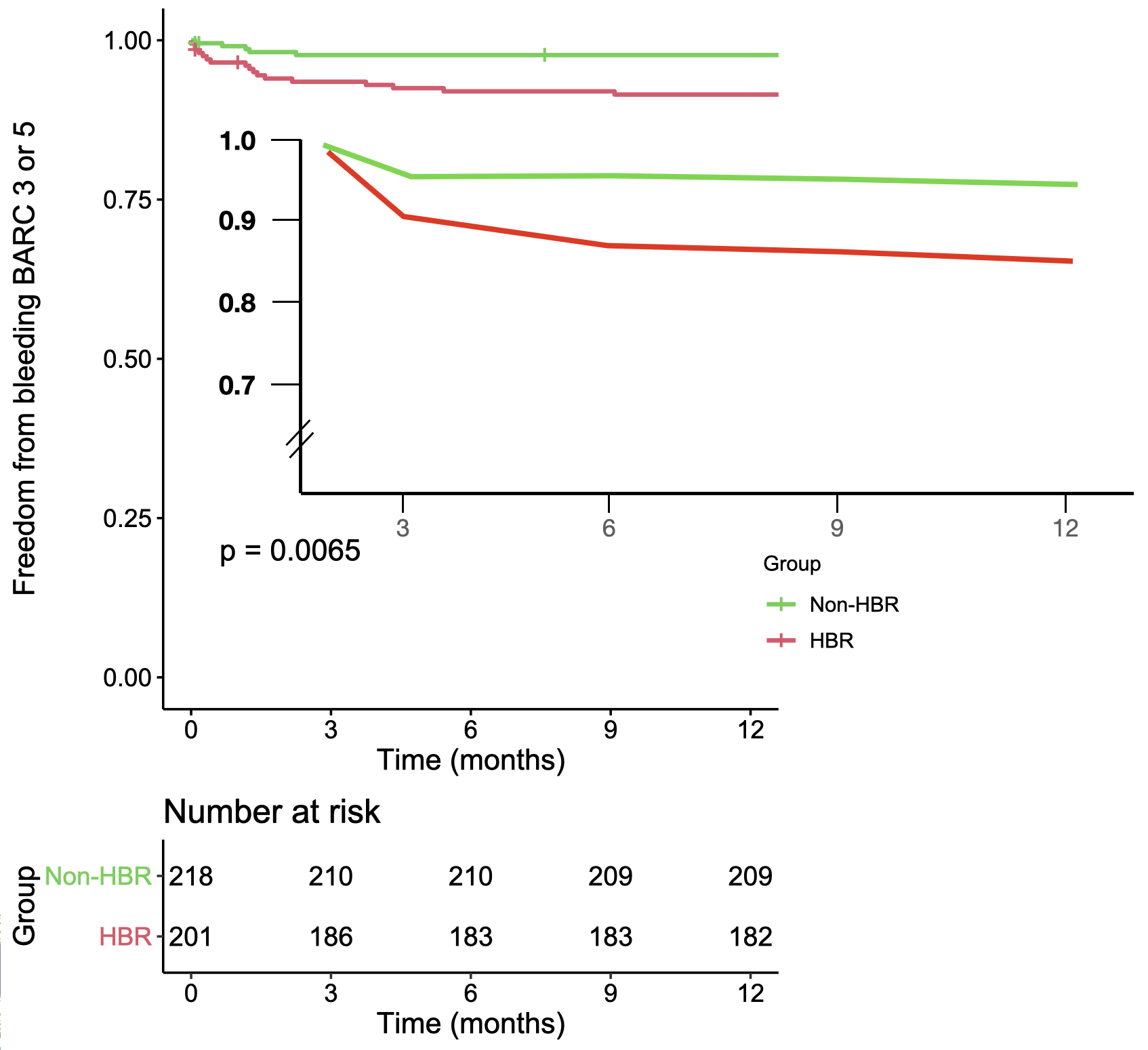
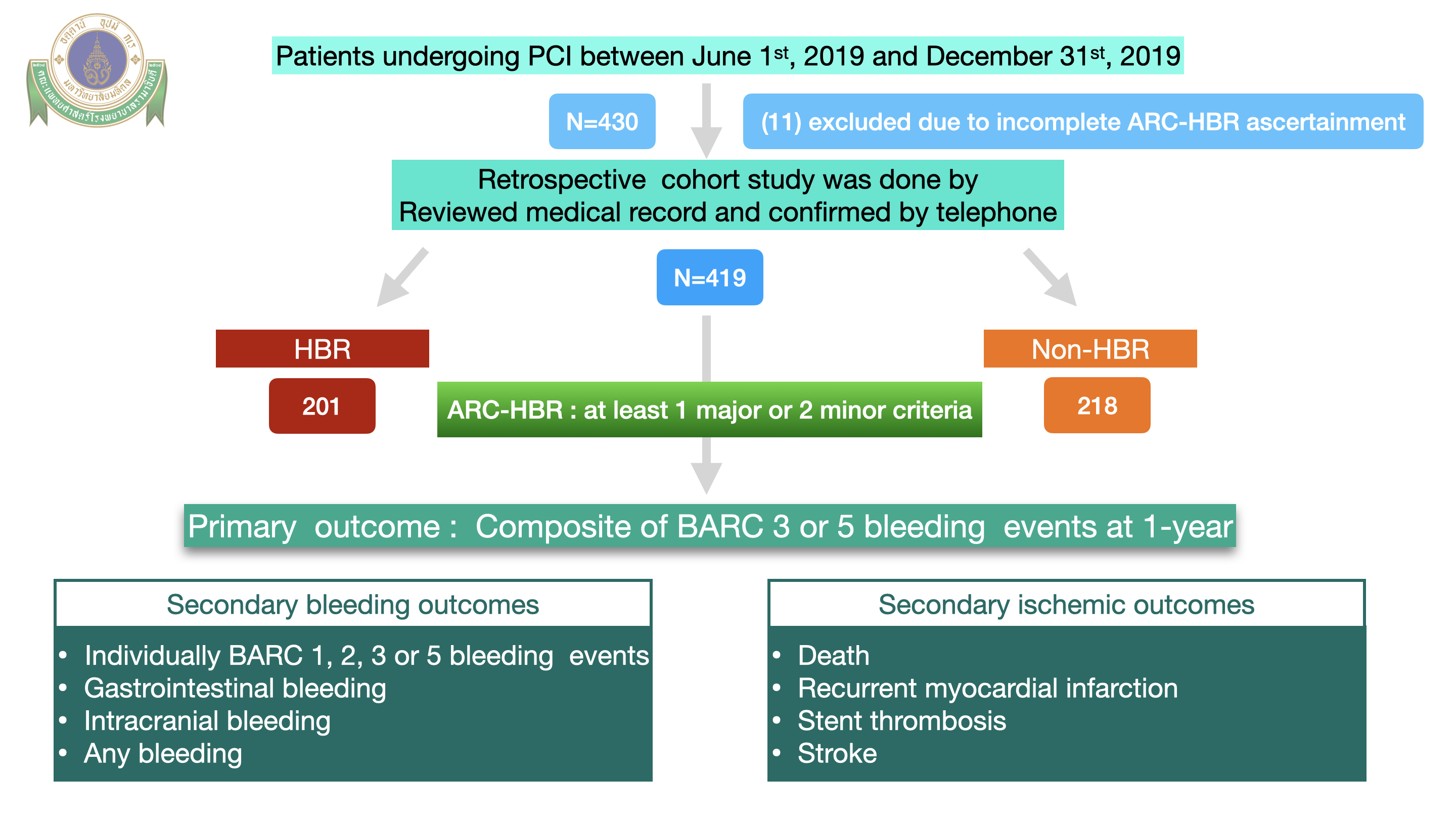
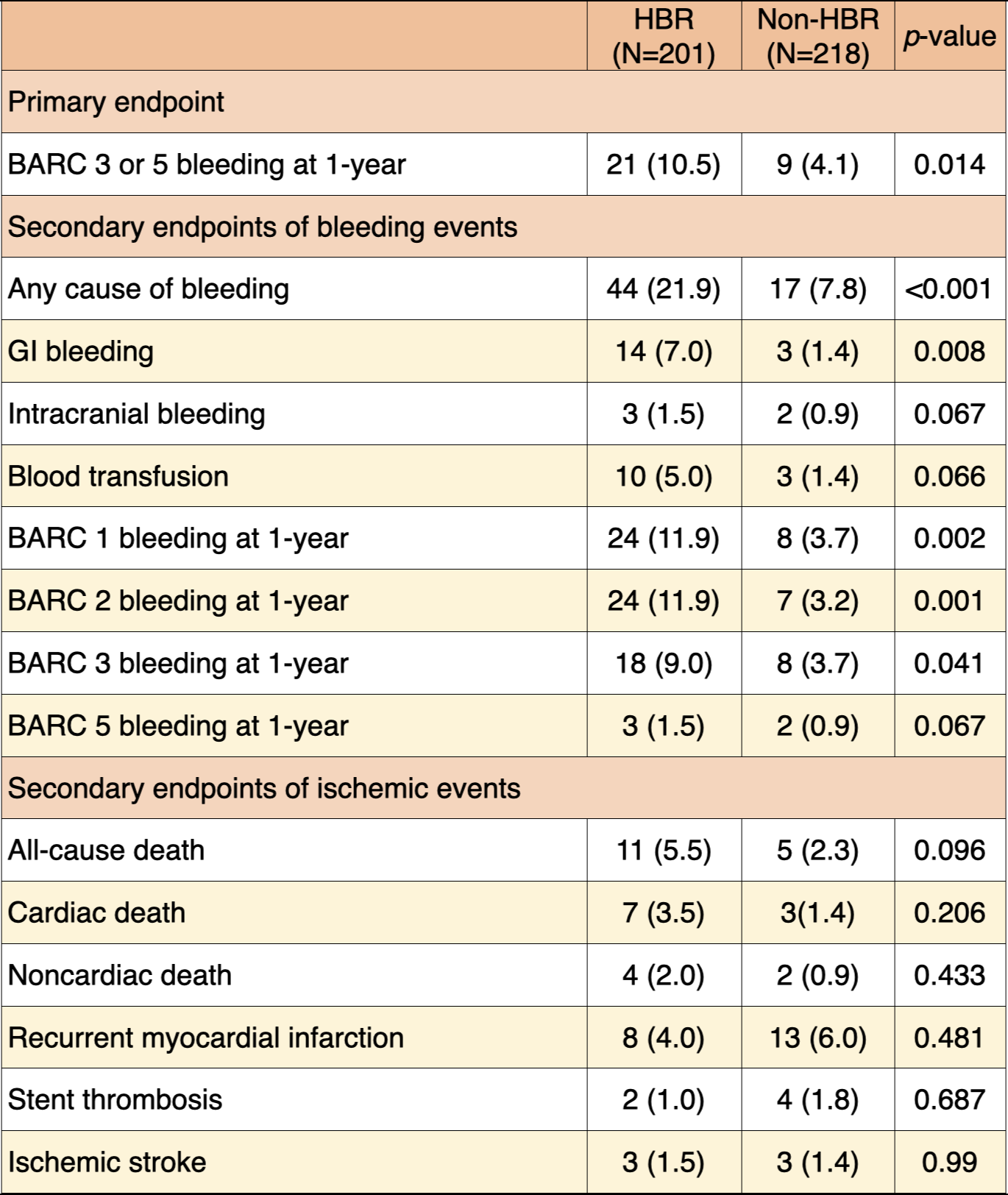
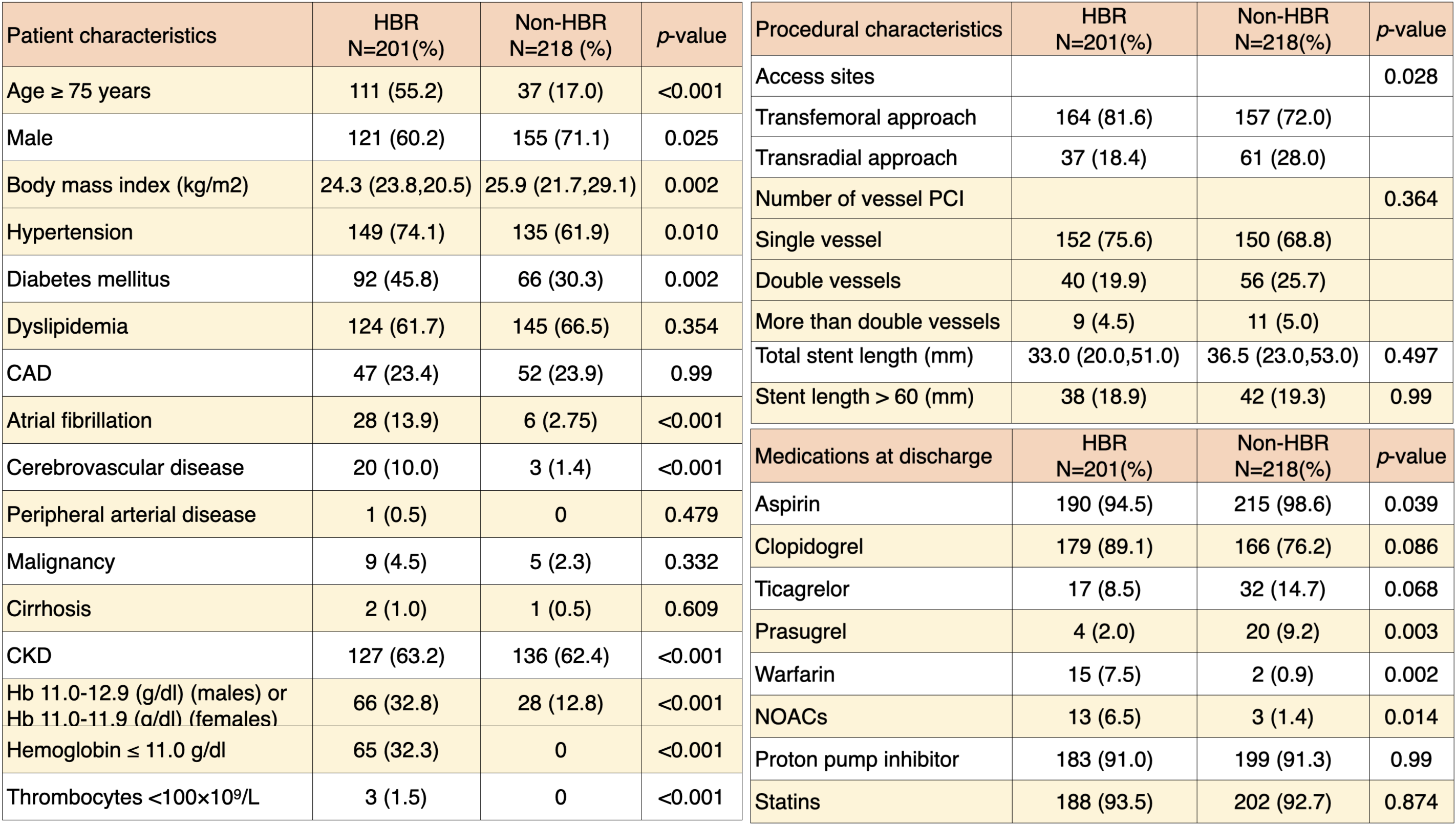
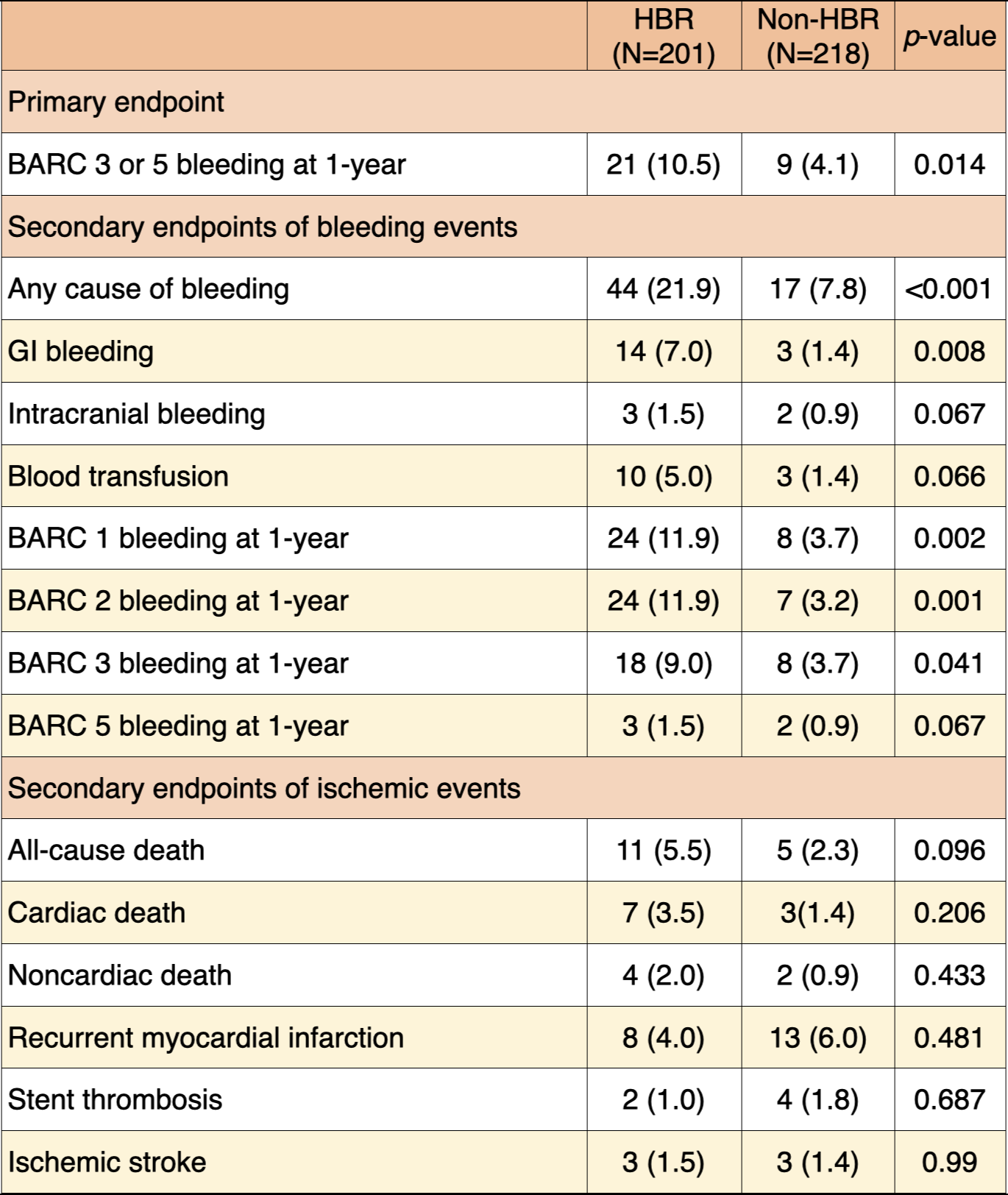
This retrospective cohort study applied the ARC-HBR high bleeding risk (HBR) definition to consecutive patients undergoing PCI in Ramathibodi Hospital between June 1st, 2019 and December 31st, 2019. Patients were diagnosed with HBR if at least one major or two minor criteria were met, and they were then followed for a year. The primary outcome of this study was the risk of Bleeding Academic Research Consortium (BARC) 3 or 5 bleeding at 1-year. Additionally, secondary outcomes were also evaluated, including the risk of gastrointestinal (GI) bleeding and ischemic outcomes—cardiovascular death, recurrent myocardial infarction (MI), and stent thrombosis.
Results
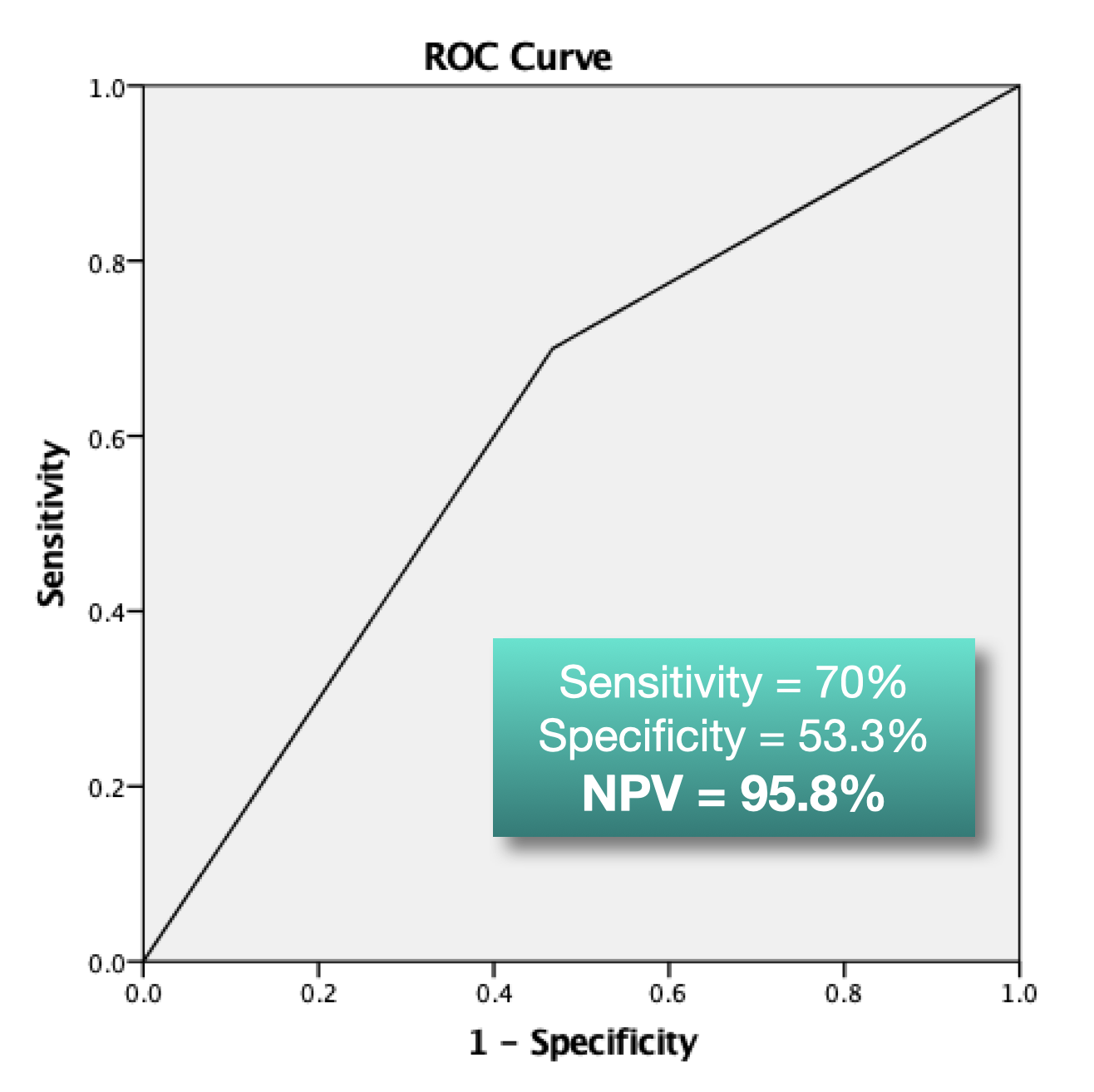
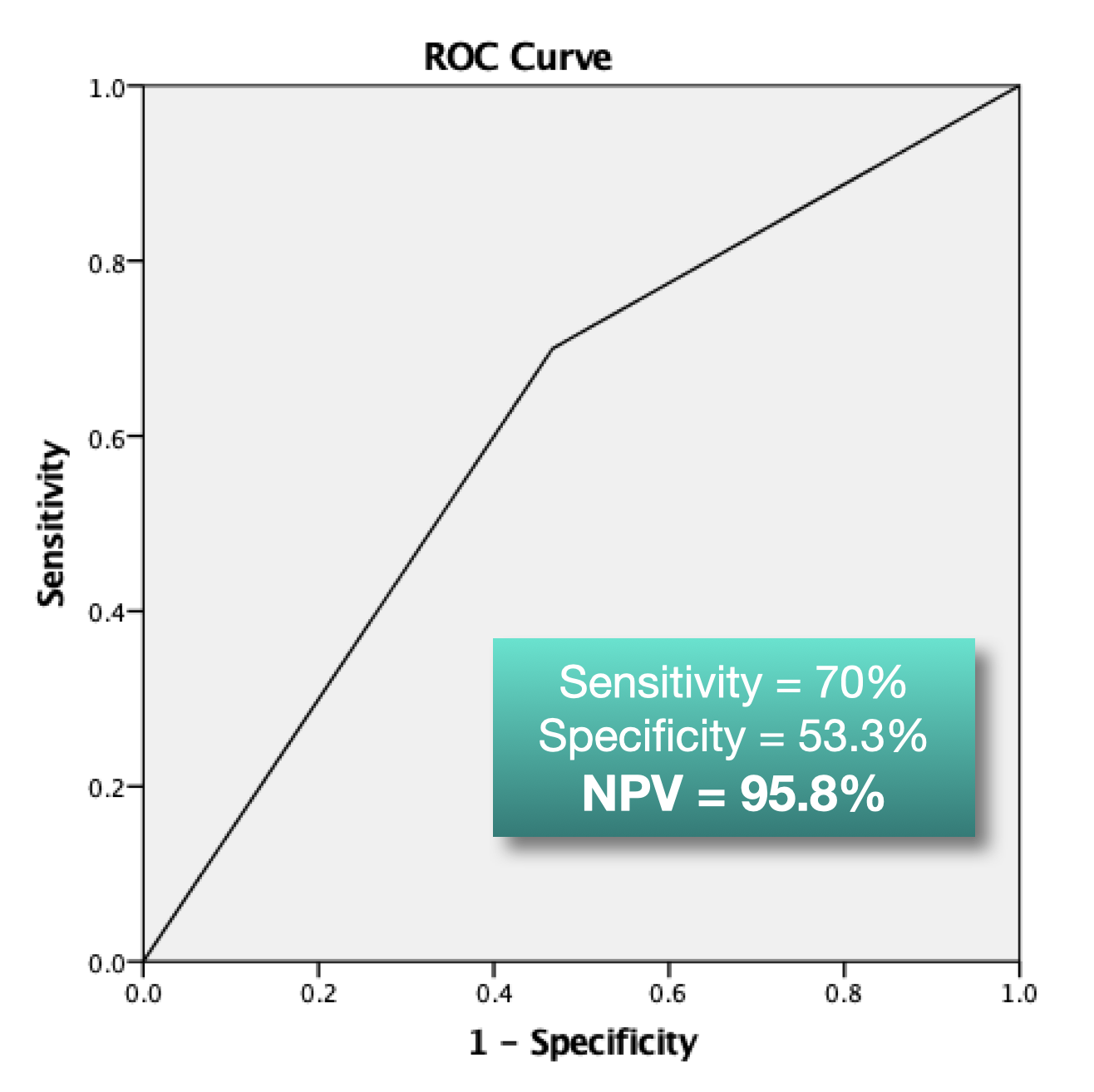
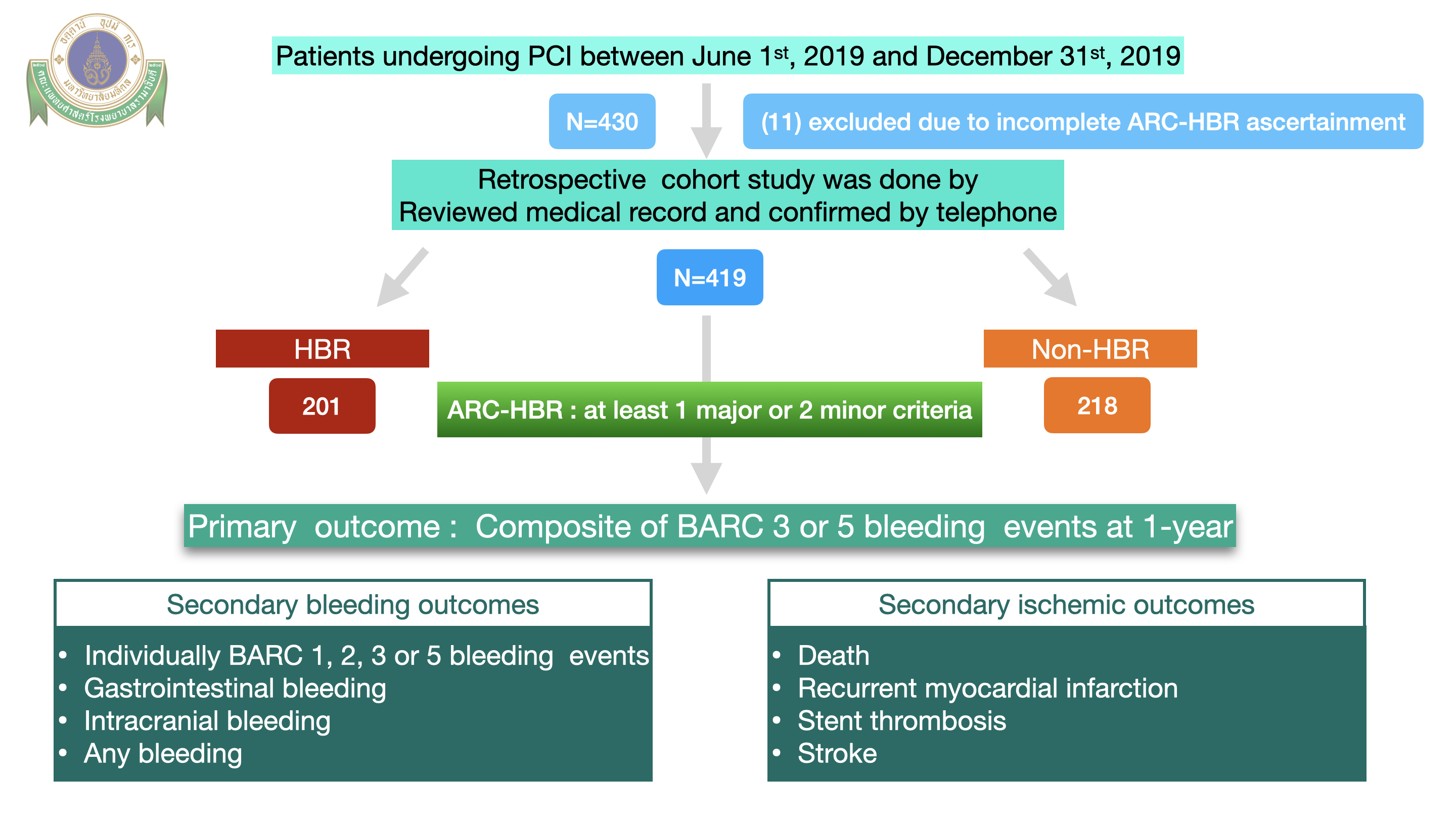
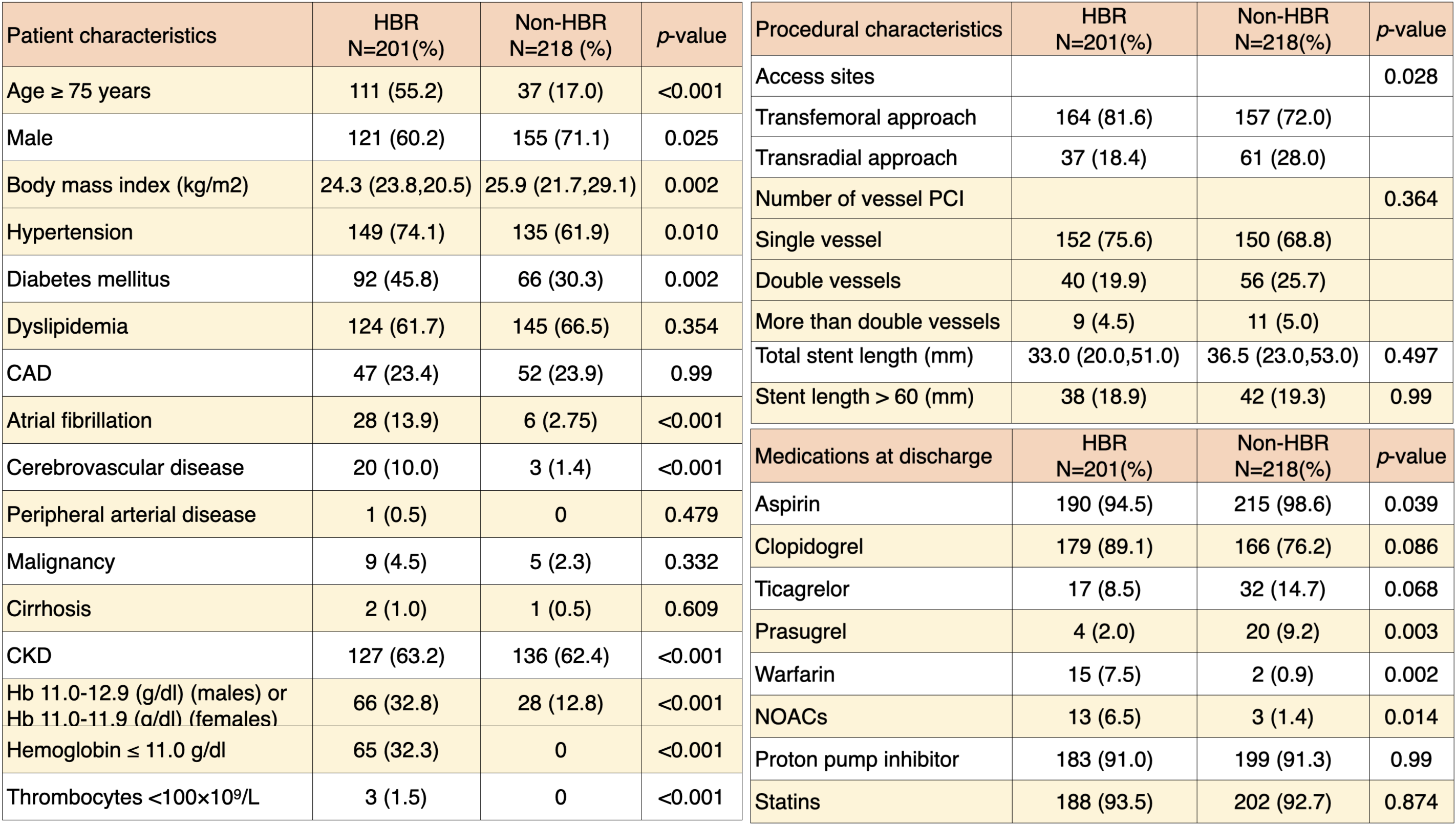
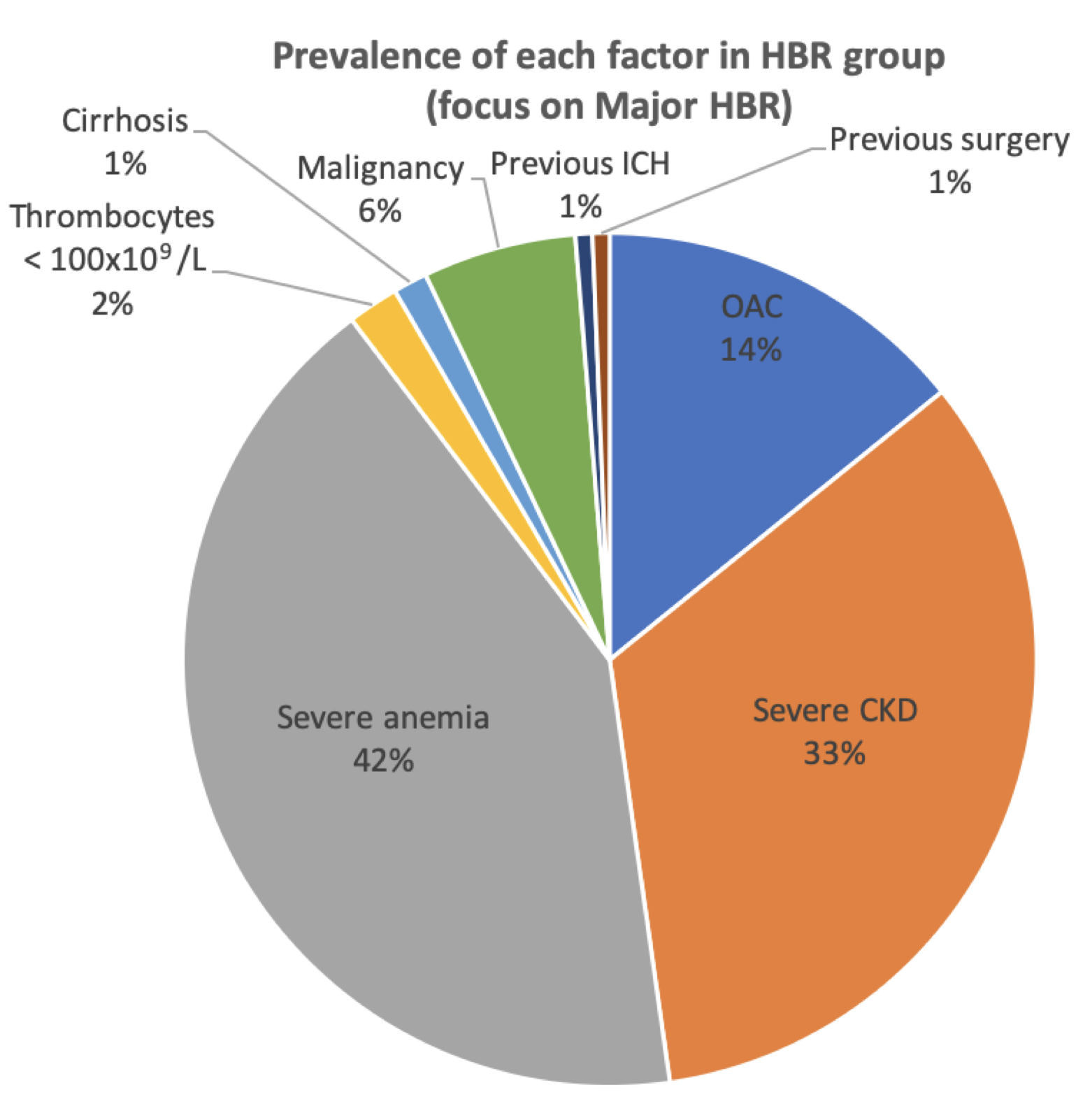
The study included 419 PCI patients (68.6 ± 12.6-year-old, 65.9% male). Two hundred and one (48%) patients identified as HBR had an increased risk of BARC 3 or 5 bleeding (10.45% vs. 3.67%; p = 0.011) and GI bleeding (6.97% vs. 1.38%; p = 0.008). There was no statistical difference among ischemic outcomes; cardiovascular death (3.48% vs. 1.38%; p = 0.21), recurrent MI (3.98% vs. 5.96%; p = 0.48), and stent thrombosis (1% vs. 1.83%; p = 0.68). The ROC curve indicated that the sensitivity of ARC-HBR is 70%, whereas the specificity is 53.3%.
Conclusion
The ARC-HBR criteria were successful in identifying patients with an increased risk of 1-year major (BARC 3 or 5) bleeding events in our study cohort of Thai patients undergoing PCI. This HBR definition could be used to help identify patients at high risk of bleeding, allowing doctors to prescribe appropriate types, doses, and durations of antiplatelets.