Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-020
Rate of Rehospitalizations and It’s Causes in Octogenarians Following Acute Coronary Syndrome: Percutaneous Coronary Intervention vs. Conservative Medical Management, Long-Term Follow Up
By Vipin Thomachan, Ali Shamsi, Ahmed Siddiqui, Gohar Jamil, Mohammed El-Harari, Maha Al Ketbi, El Shafie Taha, Mohammed Anasullah Siddiqui, Soviachen Kurian, Sajith Sukumarn, Lizy George
Presenter
Vipin Thomachan
Authors
Vipin Thomachan1, Ali Shamsi1, Ahmed Siddiqui1, Gohar Jamil1, Mohammed El-Harari1, Maha Al Ketbi1, El Shafie Taha1, Mohammed Anasullah Siddiqui2, Soviachen Kurian3, Sajith Sukumarn1, Lizy George1
Affiliation
Tawam Hospital, United Arab Emirates1, RAK Health Sciences University, United Arab Emirates2, Royal Hobart hospital, Australia3
View Study Report
TCTAP A-020
Acute Coronary Syndromes (STEMI, NSTE-ACS)
Rate of Rehospitalizations and It’s Causes in Octogenarians Following Acute Coronary Syndrome: Percutaneous Coronary Intervention vs. Conservative Medical Management, Long-Term Follow Up
Vipin Thomachan1, Ali Shamsi1, Ahmed Siddiqui1, Gohar Jamil1, Mohammed El-Harari1, Maha Al Ketbi1, El Shafie Taha1, Mohammed Anasullah Siddiqui2, Soviachen Kurian3, Sajith Sukumarn1, Lizy George1
Tawam Hospital, United Arab Emirates1, RAK Health Sciences University, United Arab Emirates2, Royal Hobart hospital, Australia3
Background
Acute coronary syndrome (ACS) is associated with high morbidity and mortality in octogenarians. Frequent rehospitalization following the index event, due to cardiac or noncardiac causes are very common in this group. Apart from cardiovascular causes, multimorbidity, age related frailty, dementia and cognitive impairments contribute to increased readmissions.
Methods
This retrospective data analysis study was aimed to evaluate the rate and causes of rehospitalizations in octogenarians following the index event. Retrospective analysis of Electronic Medical Records (Cerner) of octogenarians admitted to our hospital between year 2014and 2017 with a primary diagnosis of acute coronary syndrome (ACS) were analyzed. Patients were treated either by percutaneous coronary intervention (PCI) or conservatively (non-PCI) as per the institutional protocol and as per the decision of treating cardiologist based on patient's clinical status. Patients were followed for further events with a mean follow up of3.5± 2.2 years (1month to 93months). Mid to long term outcome in both groups were analyzed and compared. Causes and rate of re-hospitalization during this period were studied.
Results
Data of 170 octogenarians admitted with ACS during this period were selected and analyzed for the study. Of these, 52 patients (30.6%) had undergone percutaneous coronary Intervention (PCI) and 114 patients (67%) were treated conservatively (non-PCI). Patients treated conservatively were comparatively older than PCI group (86.1±6.1 vs83.6±4.6years; p=0.0106). No significant difference in gender ratio between the two groups (49.1% female in non-PCI group and 55.8% female in PCI group; p=0.4245). Majority of the patients presented with NSTEMI (97.4% in non-PCI;71.2% in PCI).
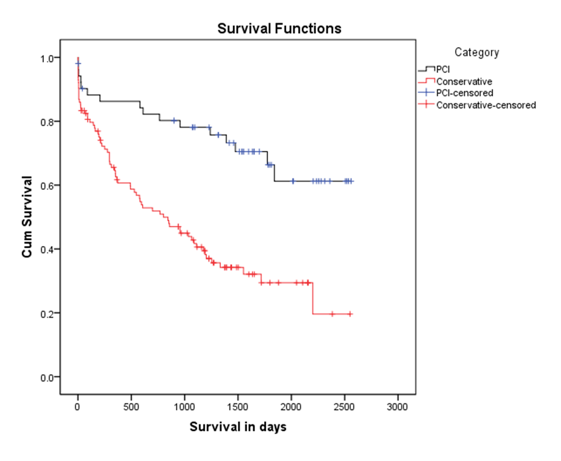
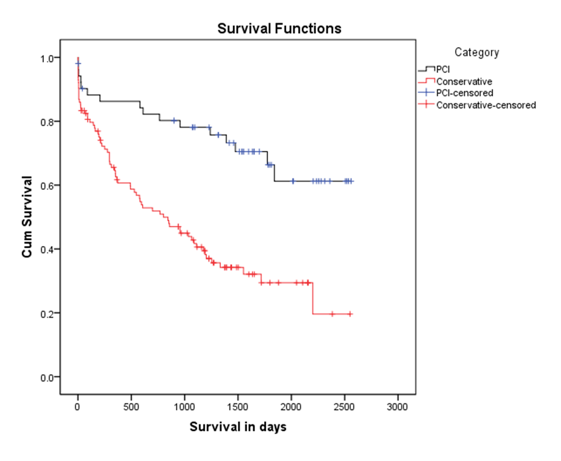
Conclusion
This retrospective data analysis study shows that morbidity and mortality are very high in octogenarians following acute coronary syndrome. Invasive strategy significantly improved the survival in selected patients compared to the conservative treatment strategy. It also reduced the rate of rehospitalizations initially. The initial benefit in rehospitalization rate associated with invasive strategy was not sustained during the long term follow up. This could probably be due to the increasing multimorbidity associated with advancing age.


