Innovations of optimal medical therapy (OMT) have left resounding, positive effects on survival in patients with stable coronary artery disease (CAD), an expert said, underscoring the need to maximize OMT, including managing risk factors.
 Sripal Bangalore, MD(New York University School of Medicine, New York, USA) addressed the evolution and role of OMT, or guideline-directed medical therapy (GDMT), in patients with stable CAD and multivessel disease (MVD) on Apr 29 at TCTAP 2022.
Sripal Bangalore, MD(New York University School of Medicine, New York, USA) addressed the evolution and role of OMT, or guideline-directed medical therapy (GDMT), in patients with stable CAD and multivessel disease (MVD) on Apr 29 at TCTAP 2022.
“Atherosclerosis is a systemic condition, meaning systemic GDMT is fundamental for optimal management, even after revascularization,” Bangalore said. “OMT should involve managing lifestyle and behavioral risk factors, achieving physiological goals, and adhering to pharmacotherapy.”
Stable CAD, also known as stable ischemic heart disease (SIHD), is a heart condition that requires medical therapy and, at times, invasive revascularization with coronary bypass artery graft (CABG) surgery or percutaneous coronary intervention (PCI).
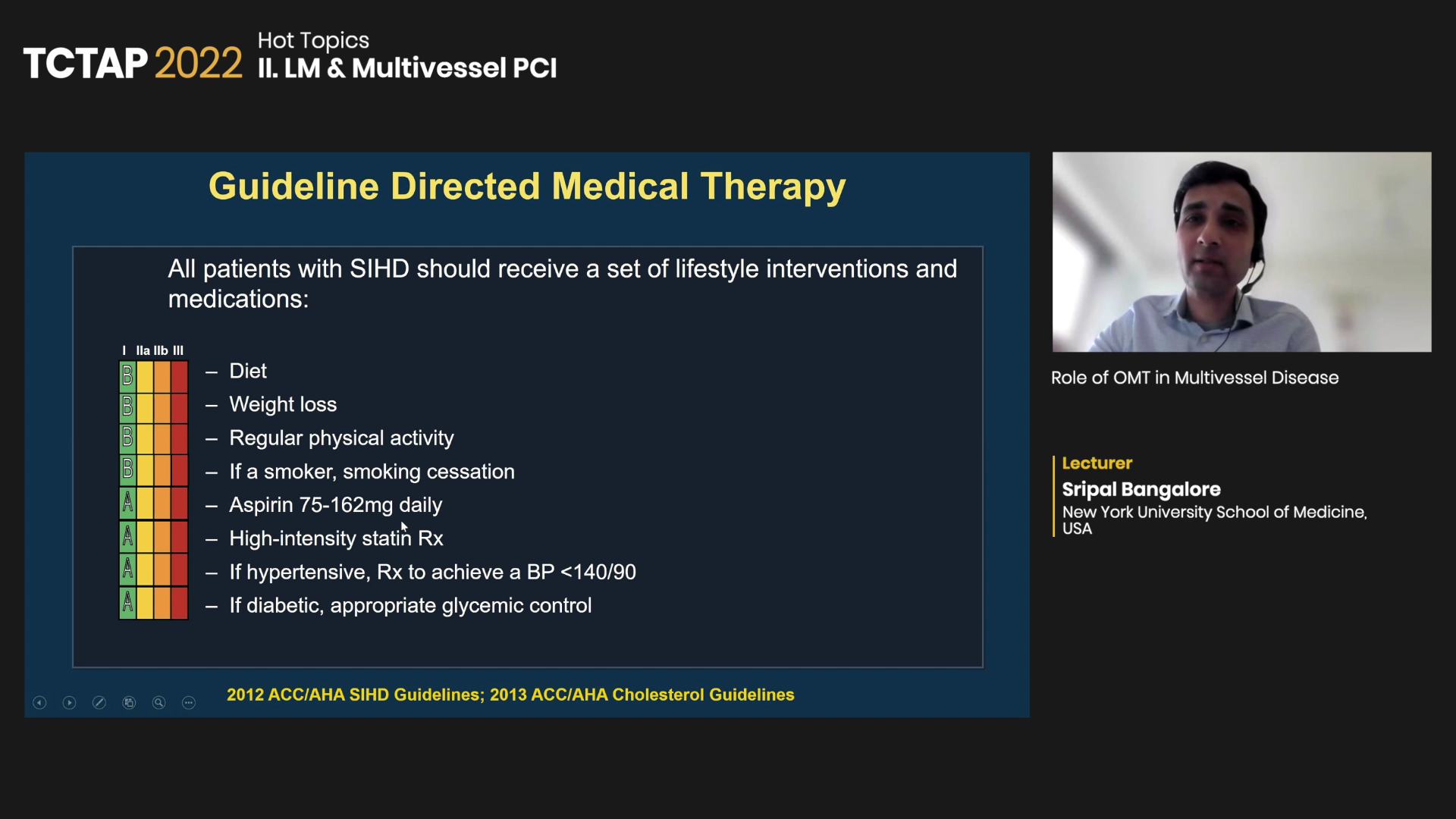
“All SIHD patients should receive a set of lifestyle interventions and OMT, which are critically important for managing stable CAD,” Bangalore said. “Medical therapy should be the backbone of all treatment, including first-line for patients treated with PCI or CABG.”
Evidence supports GDMT for lifestyle interventions like diet, weight loss, exercise and smoking cessation. Medications include antiplatelet therapy with aspirin (75-162 mg daily), lipid-lowering statin therapy, beta-blockers and hypertension drugs like angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARB).
‘Modern OMT diminishes survival benefits of CABG, PCI’
Improvements in OMT also displace some of the known survival benefits of revascularization in stable CAD, Bangalore said on the controversial topic.
As previously reported by SummitMD, comparing studies on revascularization versus OMT from the 1970s to the present day showed diminished survival benefits of PCI and CABG in the “OMT era.”
“Randomized controlled trials (RCTs) in the OMT era consistently show no difference in mortality between revascularization and OMT for the individual endpoints,” Bangalore said.
“One of the biggest problems today is that people paint broad strokes of CABG and revascularization as superior to OMT based on the composite endpoint without looking at individual endpoints.
“But data on the mortality endpoint sends a consistent message. The COURAGE trial in 2007 and the BARI 2D trial in 2009 showed no difference in death, and even the FAME 2 trial from 2012, largely viewed as a positive trial for PCI, showed no difference in mortality.”
The recent ISCHEMIA and ISCHEMIA-CKD trials found no difference in survival between revascularization and OMT, despite the “lingering confusion” on the curves separating for the endpoint of death: “Again, the two curves are superimposed with no curves crossing for 5-years.”
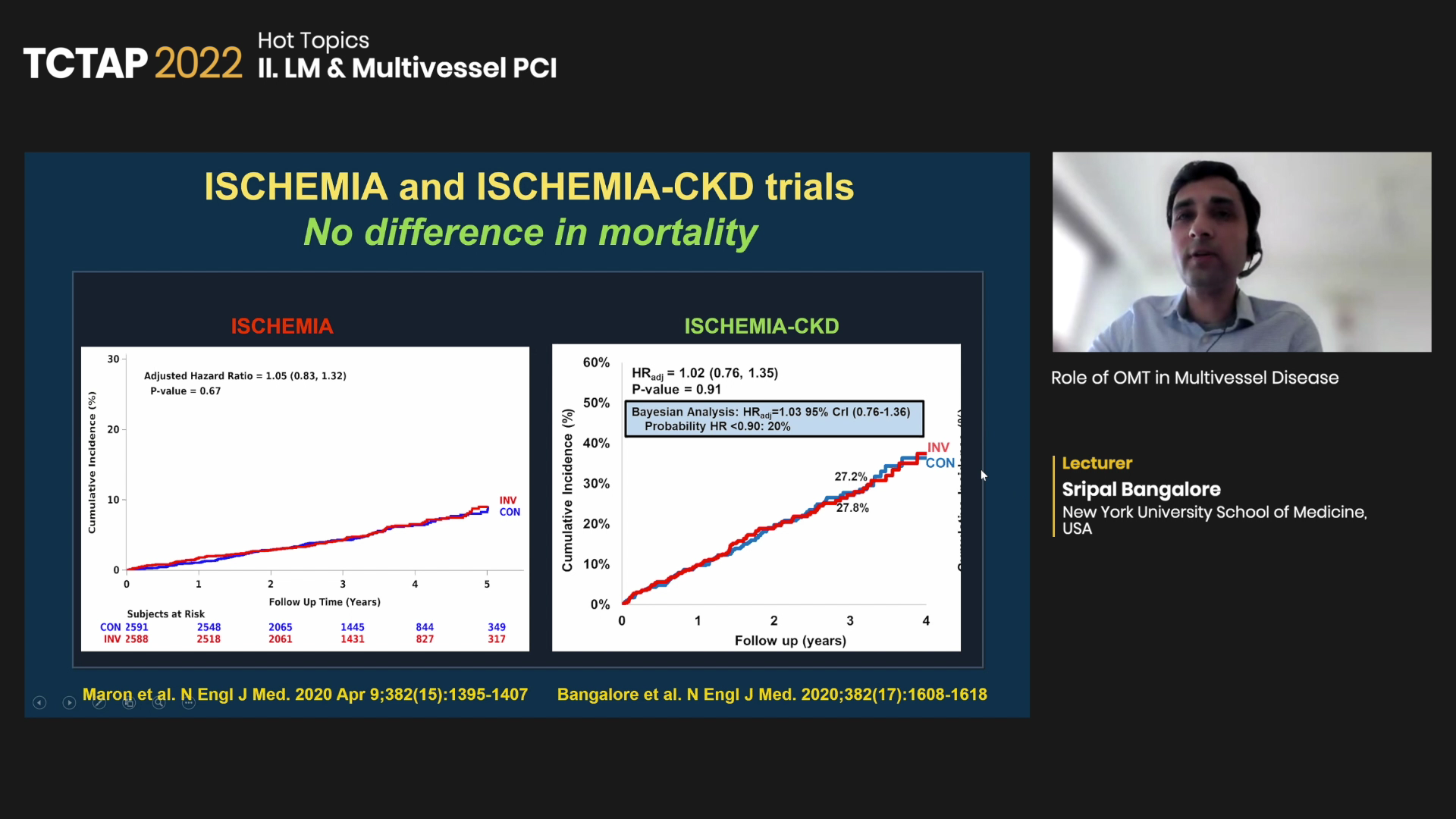
When pooling the data into a meta-analysis, Bangalore and investigators found no difference between revascularization and OMT for the endpoint of mortality (RR 0.99, 95% CI, 0.90-1.09).
Modern trials also demonstrate similar mortality rates between CABG and OMT in patients with triple-vessel disease, an area of much “confusion,” he said.
BARI 2D, for instance, showed similar mortality rates between CABG and OMT in patients with triple-vessel disease (revascularization 86.4 vs. OMT 83.6, p=0.33). Analysis of ISCHEMIA that stratified patients by 1-, 2- or 3-vessel disease showed no difference between OMT and revascularization for the 5-year mortality endpoint.
“When asking if OMT modulates the survival benefit of revascularization in stable CAD, the answer seems to be yes, there is a diminishing, not non-existent, survival benefit when medical therapy is optimized.”
OMT goals still not reached
But more needs to be done to maximize medical therapy and manage risk factors, two major aspects that could improve prognosis and increase survival benefits for patients with SIHD, Bangalore said.
Posthoc study of SYNTAX showed that OMT reduced mortality by 36% at 5-years, greater than the 26% reduction of CABG or PCI in the same time frame (HR 0.64; 95% CI, 0.48-0.85, p=0.002).
“Interestingly, only 29.1% of patients at baseline were taking OMT before revascularization compared to the 41.3% at discharge after PCI or CABG,” Bangalore said. “At 5-years, only 1/3 of patients in both groups were taking OMT (PCI 39.6% vs. CABG 35.7%), indicating more needs to be done to maximize medical therapy for patients undergoing PCI and CABG.”
Cardiovascular risk analysis of the BARI 2D trial also emphasized the importance of maximized OMT. Results showed that managing six risk factors (RF) of smoking, high-density lipoprotein cholesterol (<130 mg/dL), triglycerides (<150 mg/dL), blood pressure (<130/80 mmHg) and glycosylated hemoglobin (<7%) were strongly associated with reduced mortality (p=0.0010).
Particularly, patients with diabetes who controlled the six RFs had a 15% lower risk of death at 5-years. Compared to these patients, those who had 0 to 2 risk factors in control had a two-fold higher risk of mortality (HR 2.0, 95% CI, 1.3-33, p=0.0031).
“Each component played a role in the risk of cardiovascular events,” Bangalore said. “Most patients did not have medical therapy optimized before elective PCI, meaning risk factor management needs work.”
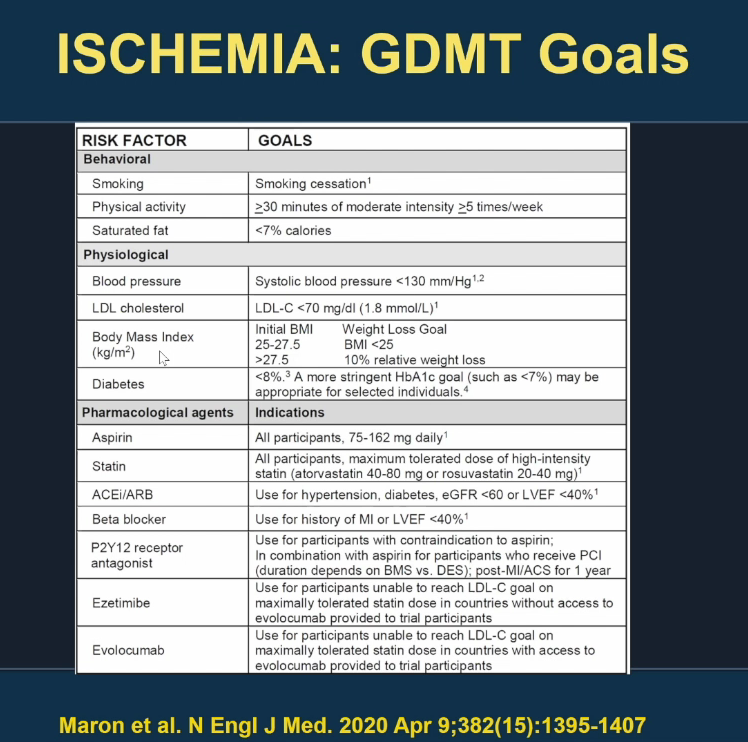
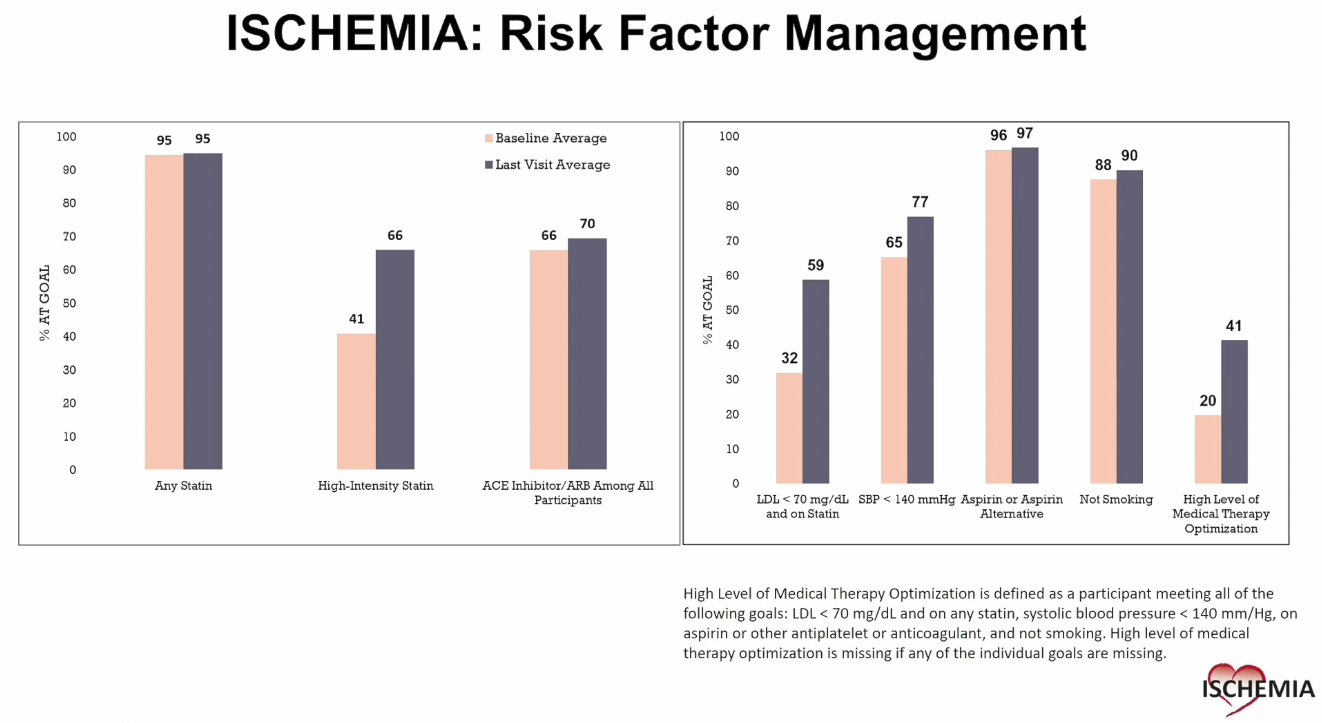
Analyzing GDMT goals in ISCHEMIA showed that around half of the patients failed to control behavioral, physiological, and medication risk factors despite significant efforts, stressing the need to optimize goal achievement and adherence.
Edited by

Joo Myung Lee, MD
Samsung Medical Center, Korea (Republic of)
Written by



