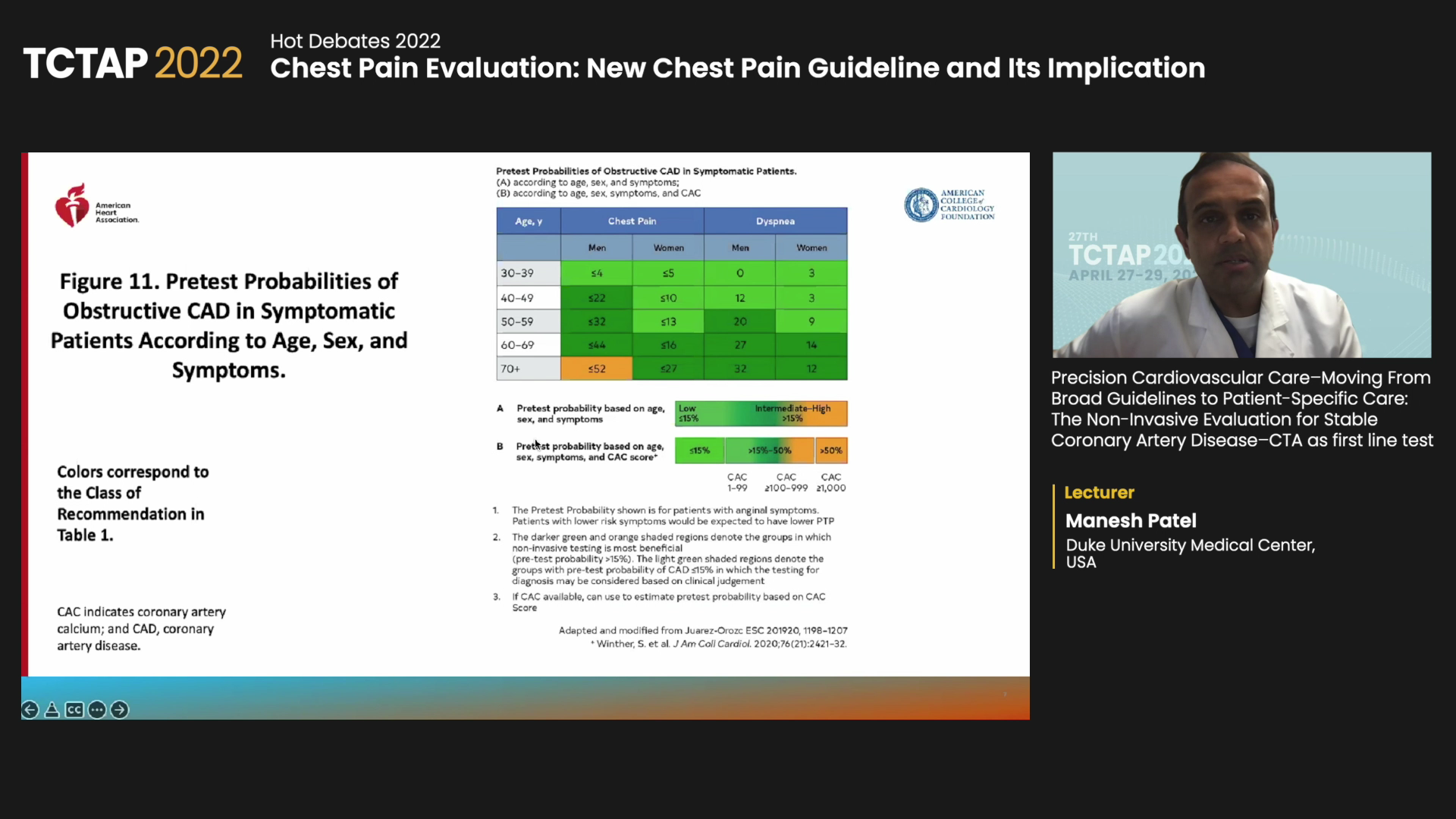
Recent American guidelines on chest pain may help clinicians choose the right noninvasive cardiac test, or skip it entirely, for patients at intermediate risk for coronary artery disease (CAD) based on chest pain symptoms and the presence of risk factors, an expert said.
 “For the first time, we have a guideline on chest pain that helps provide direction,” said Manesh R. Patel, MD(Duke Heart Center, Durham, North Carolina) at TCTAP 2022 on Apr 28. “Over a decade ago, we found that risk stratification with noninvasive testing needed significant improvement.”
“For the first time, we have a guideline on chest pain that helps provide direction,” said Manesh R. Patel, MD(Duke Heart Center, Durham, North Carolina) at TCTAP 2022 on Apr 28. “Over a decade ago, we found that risk stratification with noninvasive testing needed significant improvement.”
“Now, the guideline and its pretest probabilities bring us closer to precisely identifying an appropriate cardiovascular test to diagnose and risk-stratify for CAD in patients at intermediate-risk,” he said.
Published in the Journal of the American College of Cardiology (JACC) last October and co-written with five medical societies, the 2021 American Heart Association (AHA) and American College of Cardiology (ACC) guidance provides recommendations on the historically ambiguous area of evaluating and diagnosing chest pain.
Although the guideline warns against routine testing in low-risk patients, first-line coronary computed tomographic angiography (CCTA) and stress testing – including stress echocardiography, positron emission tomography (PET), single-photon emission computed tomography (SPECT) or cardiac magnetic resonance (MR) – were green-lighted for intermediate- and high-risk patients.
CCTA was particularly strongly recommended in patients with chest pain at intermediate risk for CAD to identify atherosclerotic plaque or obstructive CAD (Class I; LoE: A). In cases of stenosis or inconclusive CCTA, the guidelines recommend fractional flow reserve-computed tomography (FFRct) to diagnose vessel-specific ischemia or aid clinical decisions (Class IIa; LoE: B).
Stress testing earned a Class I recommendation (LoE: B) to diagnose myocardial ischemia and estimate the risk of major adverse cardiovascular events (MACE) in intermediate-risk patients with emergency chest pain and suspected acute coronary syndrome (ACS). Stress testing without imaging got a Class IIa (LoE: B) endorsement to exclude ischemia.
Early imaging to ‘move paradigm’ on chest pain, ischemia cascade
Imaging with earlier disease can push forward classic teaching on chest pain and improve the poor diagnostic yield of coronary angiography found a decade prior, Patel said.
In 2009, Patel and investigators discovered that only a minority of patients (37.6%) without known disease who underwent elective cardiac catheterization had obstructive CAD, indicating problems with the real-world use of noninvasive tests that should have theoretically improved risk stratification and reduced invasive catheterizations in patients without obstructive CAD.
“The system was broken since excess heart catheterizations were not identified and pre-angiography information had little value.” Patel said. “And the system was based on stress testing with almost no CT or FFRCT, so opportunities existed.”
“Accurate anatomic and function evaluation is ideal, but the reality of noninvasive cardiac testing – whether stress echo, stress treadmill or stress SPECT – was no lesion-specific information and high rates of false positives and false negatives.
“Now, earlier CCTA offers visualization of CAD that helps inform treatment decisions and creates an earlier pathway. Good pictures make it hard to argue the presence of atherosclerosis and whether there is no disease or a complex burden.”
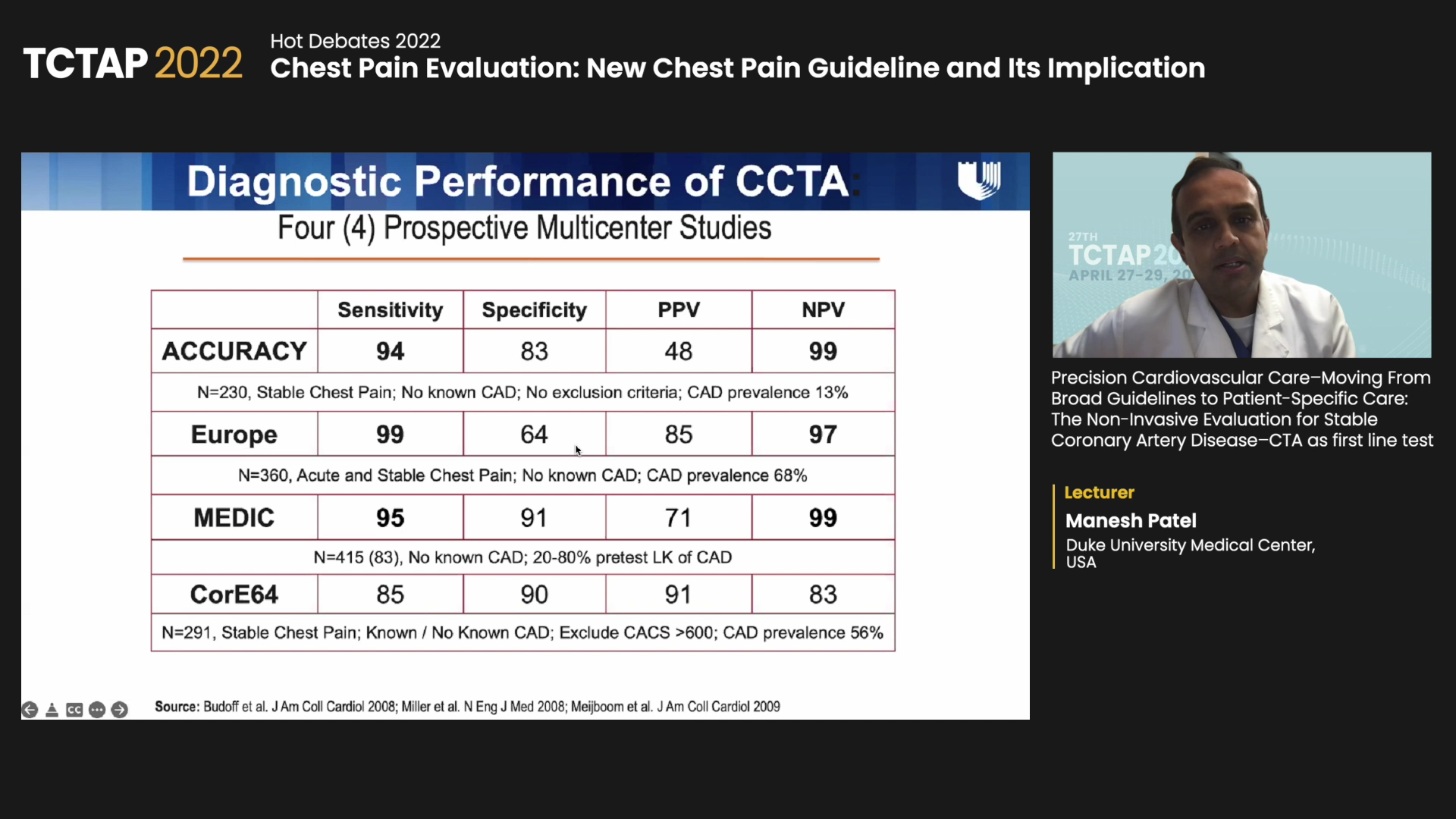
Although four prospective, multicenter studies - ACCURACY, EUROPE, MEDIC and CorE64 – demonstrated the sensitivity and specificity of stress testing and CCTA, results varied depending on the enrolled population. Meanwhile the negative predictive values of CCTA were remarkably high in all studies.
Overcoming these limitations, the 2015 PROMISE trial, co-authored by Patel and investigators, randomized 10,003 symptomatic patients to either first-line CCTA or functional testing (exercise electrocardiography, nuclear stress testing or stress echo). Baseline characteristics included hypertension in 65%, diabetes in 21% and dyslipidemia in 67% (mean age: 60; women 52%).
Investigators found no statistically significant difference in the composite primary endpoint of death, MI, hospitalization for unstable angina or major procedural complication at 25-months (CCTA 3.3% vs. functional testing 3.0%, aHR 1.04; 95% CI, 0.83-1.29, P=0.75), indicating CCTA did not improve clinical outcomes over functional testing in symptomatic patients with suspected CAD.
CCTA had fewer secondary endpoint events of catheterizations showing no obstructive CAD than functional testing (3.4% vs. 4.3%, P=0.022). Interestingly, more patients underwent revascularization, including coronary artery bypass graft (CABG), in the CCTA arm than in the functional arm (6.2% vs. 3.2%, P=0.022).
“Revascularization rates with CABG were almost two-fold (72 vs. 38),” Patel said. “But there was no significant difference in death or non-fatal MI at 3-years between the groups, although graphs showed early separation and late catch-up.”
However, the SCOT-HEART trial published in the New England Journal of Medicine (NEJM) in 2018 fatal MI at 5-years without significantly raising rates of coronary angiography or revascularization compared to standard of care alone. Accordingly, CCTA became more popular for patients with stable chest pain.
Evolving data for CCTA, FFRCT to enhance precision for chest pain tests
Focus is now on increasing precision, Patel said: “In addition to imaging in CAD, hopes of combining anatomy and function are on the rise. Multiple companies have performed FFRct with computational fluid dynamics to predict downstream pressure drop.”
Early data from a 2012 study, for instance, showed CCTA plus noninvasive FFRct improved diagnostic accuracy compared to CT alone in stable patients with suspected or known CAD and intermediate stenosis, which led to studies like DISCOVER-FLOW, DeFACTO and NXT that provided HeartFlow FFRct data.
The PLATFORM study also showed that CCTA and FFRct were associated with a significantly lower rate of invasive angiography showing no obstructive CAD, effectively reducing the number of patients without obstructive disease from being sent to the cath lab.
Conducted by Patel and investigators, the ADVANCE Registry found FFRct compared to CT alone changed management in 2/3 of 5,083 enrolled patients, and 1-year results showed patients with abnormal CT-FFRs had worse outcomes than those with normal measurements, regardless of stenosis severity.
“Data for CCTA, FFR-CT, and all tests actually, are evolving significantly,” he said. “More science is coming, including the development of a risk-prediction score based on the PROMISE trial.
“The ongoing PRECISE trial, which finished enrolling 2,100 patients, is also underway to study a precision-based testing algorithm that excludes testing in low-risk patients but offers first-line CCTA in intermediate- and high-risk groups.”
Edited by

Osung Kwon, MD
The Catholic University of Korea Eunpyeong St. Mary's Hospital, Korea (Republic of)
Written by



