Fractional flow reserve (FFR)-guided percutaneous coronary intervention (PCI) can be beneficial for patients with multivessel coronary artery disease (MV-CAD), despite recent negative study results, an expert said.
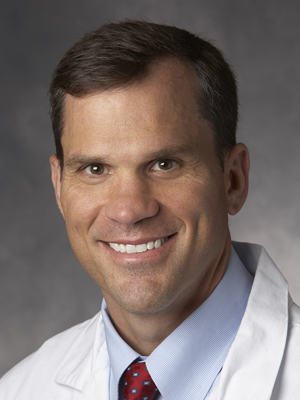 “Was 2021 a bad year for FFR?” asked William F. Fearon, MD(Stanford University School of Medicine, California, USA), the principal investigator of the FAME 3 trial at TCTAP 2022 on Apr 28. “Some investigators have interpreted the FUTURE, FLOWER-MI and FAME-3 studies published last year as negative trials, but that is not necessarily the case.”
“Was 2021 a bad year for FFR?” asked William F. Fearon, MD(Stanford University School of Medicine, California, USA), the principal investigator of the FAME 3 trial at TCTAP 2022 on Apr 28. “Some investigators have interpreted the FUTURE, FLOWER-MI and FAME-3 studies published last year as negative trials, but that is not necessarily the case.”
Last year, the FUTURE, FLOWER-MI and FAME 3 trials found no benefit with FFR-guided PCI compared to angiography-guided PCI for MV-CAD patients, resulting in uncertainty on its role in revascularization.
Despite the unfavorable results, Fearon pointed out that the studies included patients with very low rates of negative FFR, indicating that FFR-guided PCI can be beneficial for patients with MV-CAD if the application is appropriate, and results are heeded.
“Rules should be followed for any test to be useful, and for FFR, includes deferring PCI when the value is greater than 0.80,” he said. “To optimize benefits, FFR should be applied when the significance of a lesion is uncertain.”
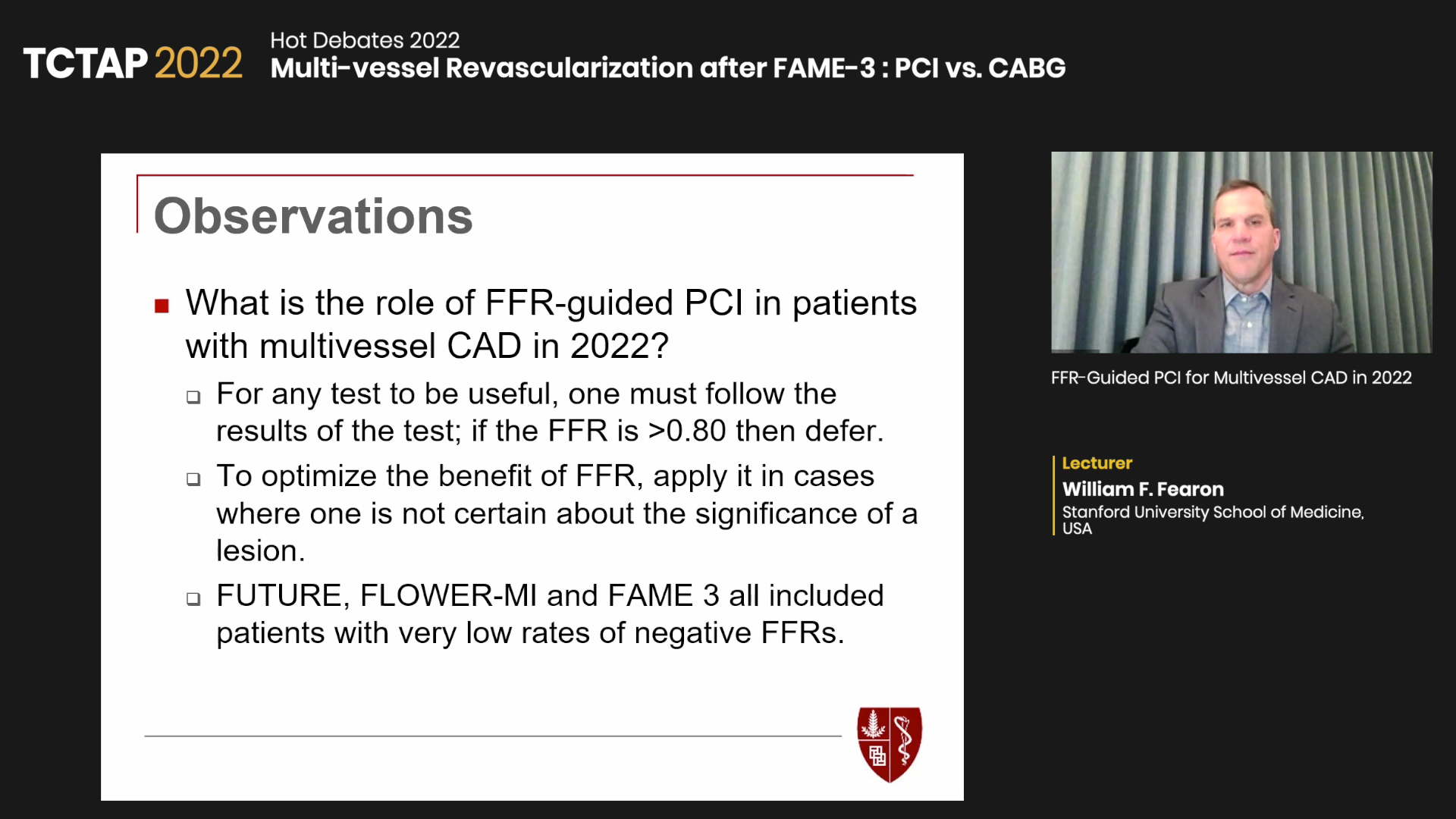
Limitations of the FUTURE, FLOWER-MI and FAME 3 studies also bar conclusions from being absolute and prod deeper analysis to understand the role of FFR in revascularization for MV-CAD, he said.
FUTURE
FUTURE investigators randomized 927 patients to an angiography-guided strategy or FFR-guided strategy with optimal medical therapy (OMT), PCI or coronary artery bypass graft (CABG). The primary endpoint was major adverse cardiac and cerebrovascular events (MACCE) at 1-year.
| FUTURE (2021) | |
|---|---|
| Design | Prospective, randomized, open-label superiority trial in France |
| Patient population | MV-CAD (n=927) |
| Randomization (1:1) | FFR-guided strategy (PCI+OMT, CABG+OMT, OMT only) vs. angio-guided strategy (PCI+OMT, CABG+OMT, OMT only) |
| Primary endpoint | MACCE (death, MI, stroke or unplanned revascularization) at 1-year. |
| Result | No difference between FFR arm and control arm: 14.6% vs. 14.4% (HR 0.97, 95% CI, 0.69-1.36; P=0.85) |
Although the study ended prematurely due to signals of increased mortality in the FFR-guided group, results at 1-year showed no difference in MACCE rates between the two groups.
Follow-up results showed no difference in mortality between angiography-guided therapy and FFR-guided therapy, indicating that the early signal of increased mortality with FFR-guidance was a “play of chance,” Fearon said, making it difficult to demonstrate real differences in outcomes.
Regarding why FFR-guidance did not outperform angiography guidance, Fearon listed the patient population, FFR-measured lesion characteristics and differing treatment strategies in both groups as major reasons.
“FUTURE had a fairly complex patient population with a relatively high SYNTAX score of 19, and more than half had triple-vessel CAD,” he said. “127 lesions were negative (FFR >0.80) but received PCI anyway, which accounted for 27% of the FFR-negative lesions.
“Among other limitations, the study was underpowered with only 54% of the planned population enrolled, and 9% of the control group and 17% of the FFR group had OMT only, indicating only 8% of patients in both groups received different treatment.”
FLOWER-MI
The FLOWER-MI trial studied FFR-guided PCI in 1,163 STEMI patients with MV-CAD who had undergone successful PCI with at least one major vessel with ≥50% diameter stenosis.
Patients were randomized to FFR-guided complete revascularization (n=586) or angiography-guided complete revascularization (n=577). The primary composite endpoint included death, myocardial infarction (MI) or unplanned hospitalization with urgent revascularization at 1-year.
| FLOWER-MI (2021) | |
|---|---|
| Design | Investigator-initiated, randomized, open-label, multicenter trial with blinded endpoint evaluation in France |
| Patient population | STEMI with MV-CAD (n=1,163) |
| Randomization (1:1) | FFR-guided complete revascularization vs. angiography-guided complete revascularization |
| Primary endpoint | Composite of all-cause death, nonfatal MI or unplanned hospitalization leading to urgent revascularization at 1-year. |
| Result | FFR arm vs. angiography arm: 5.5% vs. 4.2% (HR 1.32, 95% CI, 0.78-2.23; P=0.31) |
Results showed no difference in the 1-year primary composite endpoint but more non-fatal MIs in the FFR-guided group (3.1% vs. 1.7%; HR 1.77, 95% CI, 0.82-3.84) when examining the individual components of the composite endpoint.
However, Fearon noted that several trial limitations, including the wide confidence intervals that led FLOWER-MI investigators to warn against “a conclusive interpretation” - need consideration.
“It would have been ideal if randomization occurred after operators stated which non-culprit lesions would be treated. Instead, about 100 more lesions were identified in the FFR-guided arm (n=980) than in the angiography arm (n=891), which explains the similar rates of contrast usage and procedure time.
“You would expect less contrast and time spent with FFR, but this was not the case since more lesions were interrogated in the FFR arm.
“Other limitations include the missing FFR values on 154 lesions in the FFR-guided arm (n=980), and the sizable number of patients with negative FFR (460 lesions with FFR ≤0.80) that received PCI anyways (n=546). This may explain why the FFR and angiography arm had similar numbers of implanted stents in non-culprit lesions (1.1 stents vs. 1.5 stents).”
FAME 3
The FAME 3 trial involved 1,500 patients with triple-vessel CAD randomized to FFR-guided PCI or CABG. The composite primary endpoint was MACCE (death, MI, stroke or repeat revascularization) at 1-year.
| FLOWER-MI | |
|---|---|
| Design | Multicenter, international, non-inferiority trial |
| Patient population | 3-vessel CAD (n=1,500, mean age: 65; male 81%; diabetes 30%; ACS 40%) |
| Randomization (1:1) | CABG vs. FFR-guided PCI with DES |
| Primary endpoint | MACCE (all-cause death, MI, stroke, or repeat revascularization) at 1-year |
| Result | FFR-guided PCI arm vs. CABG: 10.6% vs. 6.9% (HR 1.5, 95% CI, 1.1-2.2). Findings not consistent with non-inferiority of FFR-guided PCI (P=0.35 for non-inferiority). |
Procedural characteristics showed PCI had a shorter time to procedure (4 min vs. 13 min), duration of procedure (87 min vs. 197 min) and length of hospital stay (3 days vs. 11 days) compared to CABG.
Both groups had similar average SYNTAX scores of 26 and number of lesions (n=4). Rates of chronic total occlusion (21% vs. 23%) and bifurcation lesions (69% vs. 66%) were not different.
Results showed a higher 1-year MACCE rate in the PCI arm (10.6% vs. 6.9%; HR 1.5, 95% CI, 1.1-2.2, P=0.35 for non-inferiority), resulting in the trial not meeting the preset criteria for non-inferiority.
There was no clear difference in the individual components of the primary endpoint. Although there was no statistically significant difference for the composite endpoint of death, MI or stroke, the FFR-guided PCI arm had numerically higher event rates.
Patients in the FFR-guided PCI arm had less severe bleeding, kidney injury and atrial fibrillation than CABG. Definite stent thrombosis and symptomatic graft occlusion were rare, and rehospitalization within 30 days occurred less after PCI.
Importantly, there was a relationship between outcomes and SYNTAX scores. FFR-guided PCI had numerically lower MACCE rates than CABG for patients with low SYNTAX scores; however, CABG outperformed FFR-guided PCI in patients with intermediate and high SYNTAX scores.
Fearon said: “It’s important to remember that only 24% of lesions of the FFR-guided patients in FAME 3 had an FFR>0.80, chronic total occlusion was present in 21% of patients, and mean SYNTAX score was 26. In these patients with mostly positive FFR, as we know from previous studies, CABG had better outcomes than PCI, therefore FFR-guided PCI was less likely to have a benefit.
“Both PCI and CABG arms showed favorable results than historical controls, including the SYNTAX trial. CABG did much better than anticipated, and an event rate similar to the SYNTAX trial in FAME 3 would have led to non-inferiority.
“These results show that FFR-guided PCI is less likely to benefit patients with complex CAD - where FFR is mostly positive - and in areas where CABG is known to outperform PCI.”
Edited by
Chang Hoon Lee, MD
VHS Medical Center, Korea (Republic of)
Written by



