Contemporary trials on stable ischemic heart disease (SIHD) are refuting notions that coronary artery bypass graft (CABG) extends survival more than optimal medical therapy (OMT), an expert said recently.
And such data were reflected in the updated, albeit controversial, 2021 American College of Cardiology, American Heart Association and Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) guidelines on coronary artery revascularization published in Circulation last December.
 At TCTAP 2022 on Apr 27, Sripal Bangalore, MD(New York University School of Medicine, New York, USA) addressed the confusion surrounding the controversial recommendations, having served on the writing committee of the 109-page document drafted to replace the 2012 ACC/AHA guidelines for SIHD.
At TCTAP 2022 on Apr 27, Sripal Bangalore, MD(New York University School of Medicine, New York, USA) addressed the confusion surrounding the controversial recommendations, having served on the writing committee of the 109-page document drafted to replace the 2012 ACC/AHA guidelines for SIHD.
“The recommendations on triple-vessel disease generated the controversy, and the notion was that the guideline committee simply downgraded CABG recommendations,” he said. “But the committee considered various factors like recent studies that showed no survival benefit with revascularization compared to OMT.”
“In the 1980s, there was a clear benefit with CABG in triple-vessel disease at 6-months when comparing surgery to no surgery,” he said. “But fast forward to the BARI 2D trial in 2009 that looked at CABG versus medical therapy in the same population, and results show no difference between CABG and medical therapy.
“This is purely looking at the mortality endpoint of CABG only, not percutaneous coronary intervention (PCI), and studies show less benefit than the ‘80s.”
Controversial 2021 US CABG recommendations trigger surgical backlash
Major American surgical groups, including the American Association for Thoracic Surgery (AATS) and the Society of Thoracic Surgeons (STS), and several international surgical associations withdrew endorsement for the updated guidelines last December.
The main objections pertained to the knockdown of CABG from a Class I to a Class IIb and the equalizing of PCI to CABG (both Class IIb) for patients with multivessel disease (MVD) and normal ejection fraction (EF).
Also protested was the Class IIa recommendation for PCI as a reasonable alternative to CABG to improve survival for patients with left main disease (LMD).
Among other disagreements, using the ISCHEMIA trial as the only evidence to back the changes fueled the controversy.
| 2021 ACC/AHA/SCAI myocardial revascularization guidelines | ||
|---|---|---|
| COR | LOE | Recommendation |
| Left main disease | ||
| I | B-R | In patients with SIHD and significant LM stenosis, CABG is recommended to improve survival |
| IIa | B-NR | In selected patients with SIHD and significant LM stenosis where PCI can provide equivalent revasc to CABG, PCI is reasonable to improve survival |
| Multivessel disease | ||
| IIb | B-R | In patients with SIHD, normal EF, significant stenosis in 3 major coronary arteries (w/ or w/o proximal LAD) and anatomy suitable for CABG, CABG may be reasonable to improve survival |
| IIb | B-R | In patients with SIHD, normal EF, significant stenosis in 3 major coronary arteries (w/ or w/o proximal LAD) and anatomy suitable for PCI, the usefulness of PCI to improve survival is uncertain. |
‘Updates reflect mortality benefits of CABG found in modern trials’
Bangalore cleared up the “confusion” at the virtual conference, noting that the committee sifted out older data and backed contemporary ones for purely the mortality endpoint.
“Most of the confusion comes from the mortality and composite endpoints,” he said. “For the Class IIb recommendation for CABG in MVD, the guideline focuses only on the benefit of survival, not the primary composite endpoint.”
While older studies showed a clear survival benefit with CABG compared to no CABG, advances in modern medical therapy closed the gap between CABG and OMT to a non-existent difference.
Meta-analysis of older studies showed that although CABG had survival benefits to 5-years, the curves began to converge at 10-years and result in a smaller absolute difference.
Meanwhile, contemporary trials in the “modern era of OMT” like COURAGE (2007), BARI 2D (2009) and FAME 2 (2012) consistently showed no significant difference between revascularization and OMT for the mortality endpoint for SIHD patients.
Recent trials like ISCHEMIA and ISCHEMIA-CKD also showed no survival benefit with revascularization than medical therapy alone.
We’re not saying don’t revascularize for triple-vessel disease; other reasons for revasc can include preventing other CVD events, improving QoL and considering patient preference.
A modern meta-analysis published in 2020 on 14 randomized controlled trials (RCTs) and 14,877 patients by Bangalore’s research team (average follow-up: 4.5 years) also showed routine revascularization was not associated with improved survival but lowered the risk of nonprocedural myocardial infarction (MI) and unstable angina.
Results also showed revascularization led to greater freedom from angina but at the expense of higher rates of procedural MI.
“Although RCTs in the pre-OMT era showed a clear benefit with CABG for improving survival compared to no surgery, these studies were conducted with no medical therapy,” Bangalore said. “Now, recent SIHD studies on revascularization show no improvement in cardiac death with revascularization compared to OMT.”
“Although a recent meta-analysis by Navarese showed a near 20% mortality reduction with coronary revascularization and medical therapy (RR 0.79, 95% CI, 0.67–0.93, P<0.01), the included trials were conducted more than 10 years ago.
“Even when considering the data, the absolute reduction is 0.2% per year, making it important for patients to consider since the mortality benefit is small.
“The consistent message across COURAGE, BARI 2D and FAME 2 was the lack of mortality difference between revascularization and medical therapy. Again, the focus is on mortality only, which is a point of lingering confusion.”
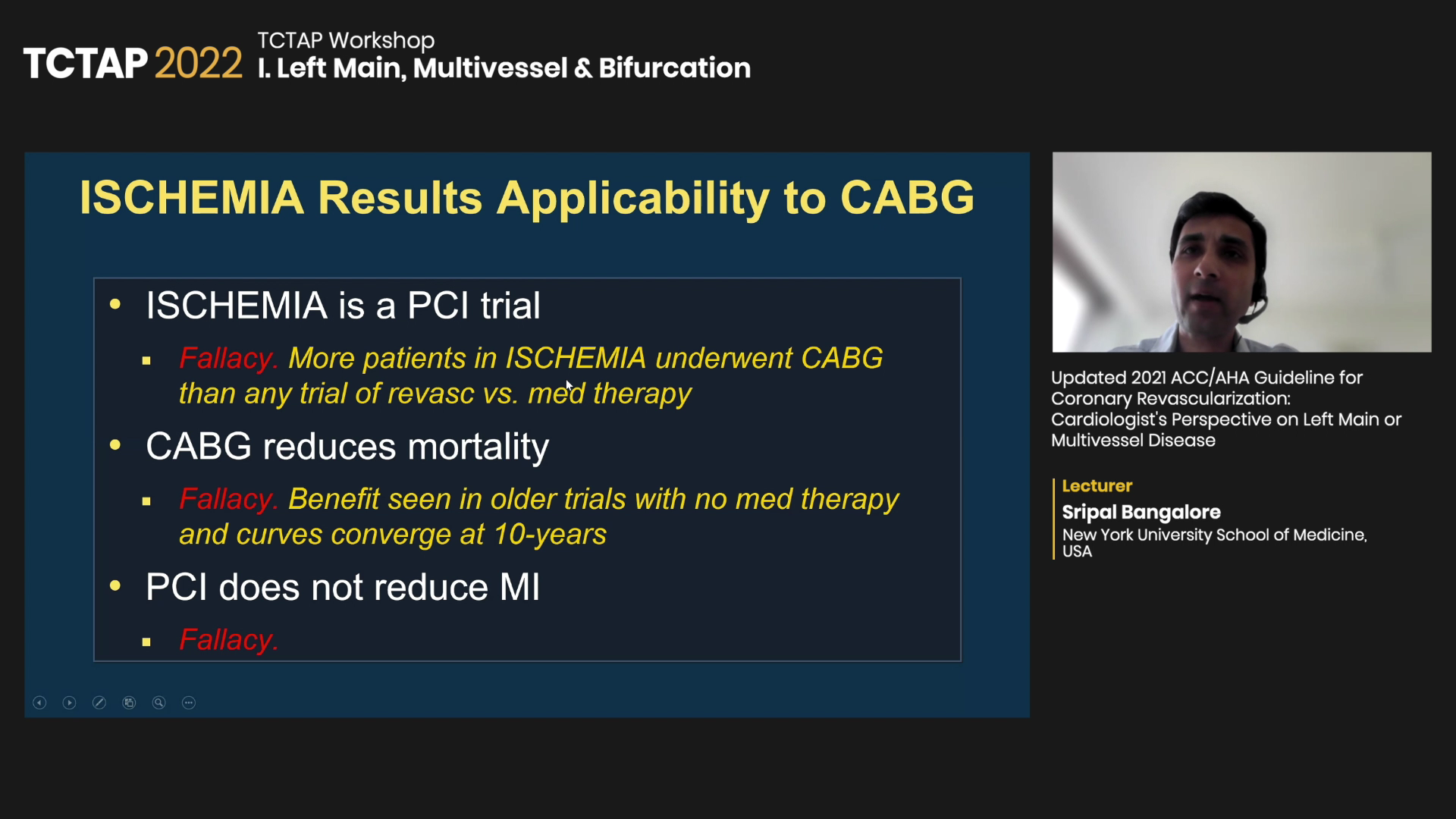
‘Assumptions’ of survival benefit with CABG, no MI benefit with PCI ‘fallacies’ in subgroups
Lack of survival benefits with CABG applies to patient subgroups of LMD, left ventricular (LV) dysfunction, triple-vessel disease, proximal left anterior descending (LAD) coronary artery disease and extensive ischemia, Bangalore said.
“The 2012 ACC/AHA guidelines suggested that revascularization reduces mortality for all SIHD patients, but evidence shows that STICH was the only trial that clearly demonstrated survival benefits for LV dysfunction,” he said. “Contemporary trials show no survival benefit with revascularization in subgroups with triple-vessel disease, proximal LAD disease and extensive ischemia.”
For LMD, data did show survival benefits for SIHD and high-risk subgroups, but the trials were from the 1990s – making their application in modern practice “questionable.”
Regarding the ISCHEMIA study, he said: “ISCHEMIA is not just a PCI trial since more than 500 patients were treated with CABG, and that far exceeds any other trials from the 1980s that compared CABG to no CABG.”
The notion that PCI fails to lower MI is another fallacy since ISCHEMIA showed PCI significantly reduced spontaneous MI (types 1, 2, 4b, 4c), albeit, with an increase in procedural MI (types 4a, 5), he said.
For angina-related quality-of-life (QoL), studies showed revascularization had sustained, durable improvement at 4-years, mostly in symptomatic patients, indicating non-mortality-related benefits.
“We’re not saying don’t revascularize for triple-vessel disease,” he said. “There are benefits like preventing other cardiovascular events such as spontaneous MI and improving QoL for symptomatic patients.
“Other reasons for revascularization include improving angina-related QoL and reducing spontaneous MI. Patient preference is also an important factor, which the guidelines underscore with recommendations for patient and heart team discussions.”
Edited by

Ju Hyeon Kim, MD
Asan Medical Center, Korea (Republic of)
Written by



