Leading with coronary angiography and intravascular imaging can help reveal the degree of calcification in coronary lesions and predict stent expansion during percutaneous coronary intervention (PCI) with drug-eluting stents (DES), an expert said.
 Akiko Maehara, MD (Cardiovascular Research Foundation, New York, USA) shared intracoronary imaging strategies for calcified coronary lesions to improve PCI outcomes at the 27th TCTAP 2022 on Apr 27.
Akiko Maehara, MD (Cardiovascular Research Foundation, New York, USA) shared intracoronary imaging strategies for calcified coronary lesions to improve PCI outcomes at the 27th TCTAP 2022 on Apr 27.
“Starting with angiography is quite helpful,” Maehara said. “No calcium on angiography signifies either small or insignificant calcium volume and good stent expansion; however, angiography-detected calcium indicates a strategy may require more than just balloon-stenting for calcium fracture.”
“Overall, understanding the entire calcium volume and confirming calcium fracture before stenting is important,” she said. “Imaging modalities and scoring systems like the optical coherence tomography (OCT) based calcium scoring system and intravascular ultrasound (IVUS) calcium score help operators choose a proper treatment modality.”
Coronary calcification is associated with increased procedural challenges and worse outcomes, acting as a significant barrier to full stent expansion during PCI.
Although angiography is the primary tool for PCI, the range and depth of details it provides are limited compared to contemporary invasive intracoronary imaging tools like IVUS and OCT that enable examination of “angiographically-invisible” calcification.
But lack of standardization for both imaging modalities and clinically relevant calcium characteristics have led to the underutilization and heterogeneous use of intracoronary imaging across operators and centers.
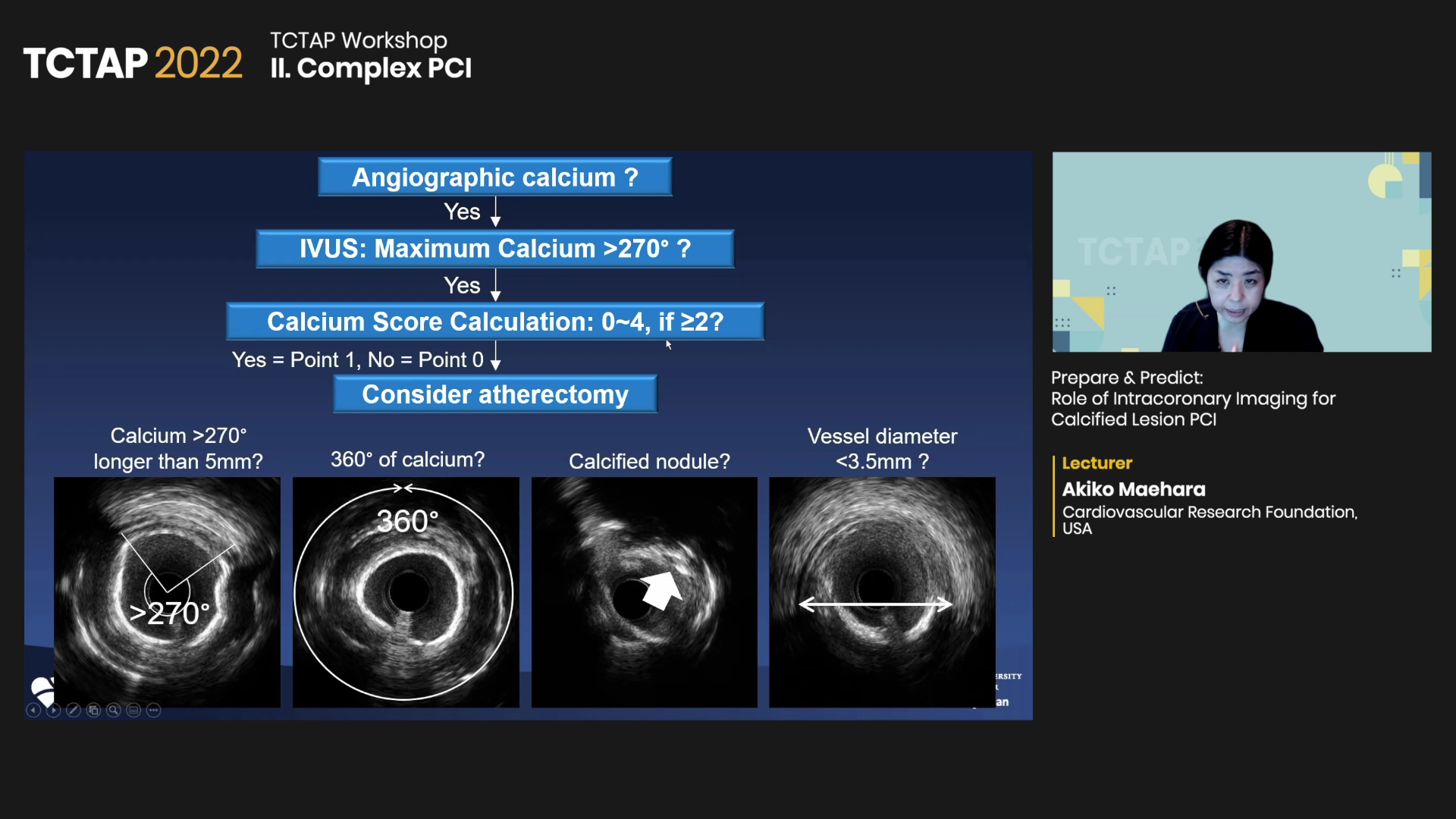
To address the ambiguity of imaging strategies for complex PCI procedures, Maehara emphasized using coronary angiography first, followed by IVUS or OCT, and their scoring system for calcification.
“Although IVUS and OCT can reveal finer calcium details, studies show that angiographically-invisible calcium does not inhibit stent expansion, Maehara said. “This indicates that initial angiography can detect significant lesion calcification and predict good stent expansion.”
For scoring indexes, the OCT-based calcium scoring system developed by Maehara’s team can help identify independent predictors of stent expansion based on criteria such as the maximum calcium angle (>180°, 2 pt), maximum calcium thickness (>0.5 mm, 1 pt), and calcium length (>5 mm, 1 pt), she said.
A multivariate analysis of the OCT-based calcium scoring system showed lesions with a calcium score 0-3 points was associated with excellent stent expansion. In contrast, a 4-point lesion was associated with poor stent expansion (96% vs. 78%, p<0.01).
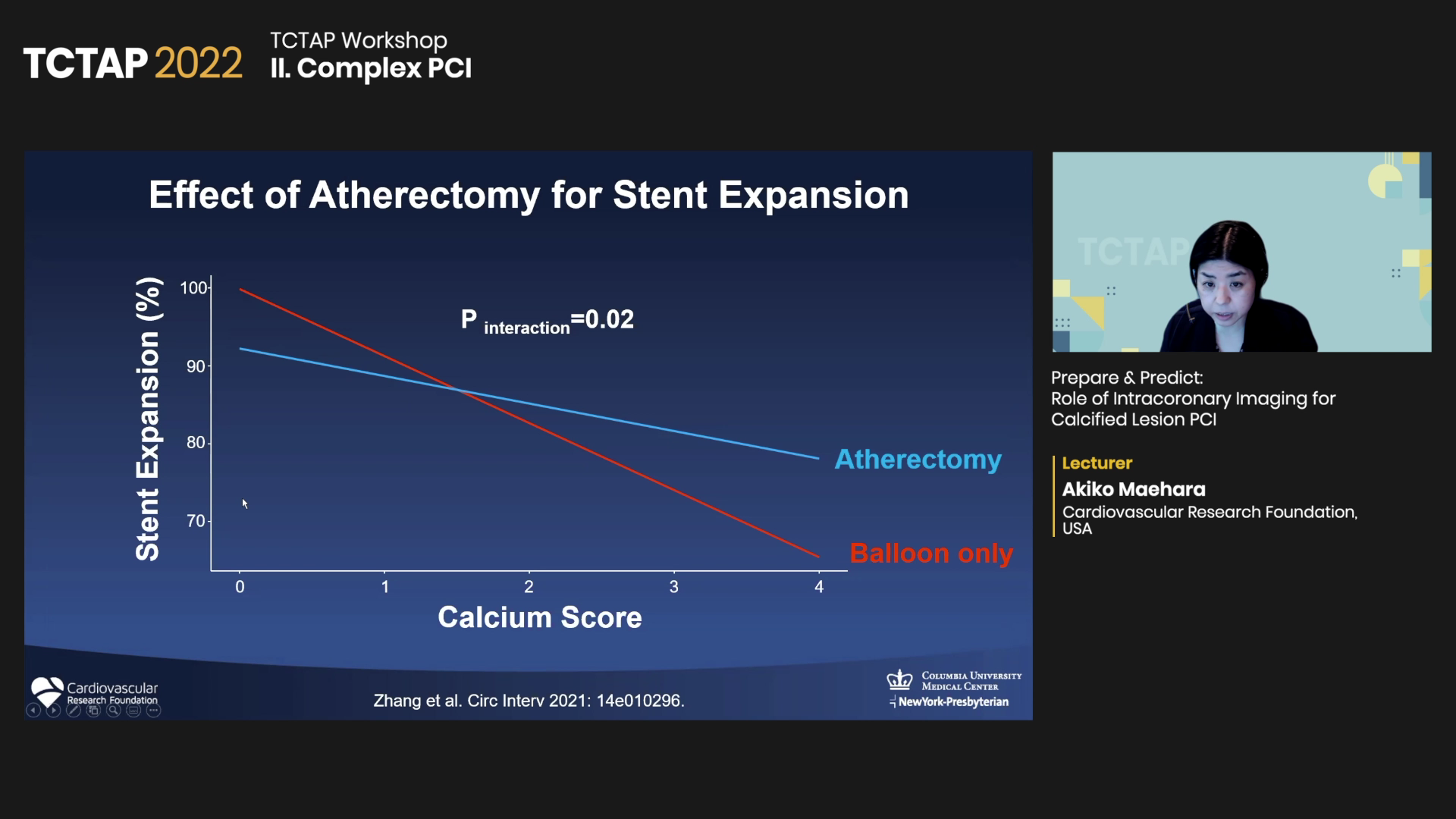
The IVUS calcium score, also developed by Maehara and colleagues, helps determine calcium fracture, a characteristic strongly associated with improved stent expansion.
The score recommends atherectomy when two or more out of four criteria are satisfied: maximum superficial calcium >270° in lesions longer than 5 mm, circumferential calcium, presence of calcified nodule, and IVUS-based vessel diameter <3.5 mm. Studies have shown that atherectomy helps stent expansion in patients with high calcium scores.
For IVUS-detected calcified nodules treated with PCI, the risk of in-stent restenosis was significantly higher. As a potential solution, Maehara proposed shockwave lithotripsy as a potential solution, although its long-term outcomes are uncertain.
An OCT-based study on 31 patients with severely calcified lesions treated with shockwave lithotripsy (Shockwave Coronary Rx Lithoplasty System, Shockwave Medical) showed high-resolution imaging helped achieve calcium modification with calcium nodule and stent expansion.
For in-stent restenosis, Maehara noted that measuring neointimal calcium can aid understanding of what is happening in older stents and confirm calcium to predict the expansion of a new stent.
“The value of the OCT and IVUS calcium scores has been established, so the takeaway is recognizing the total calcium volume,” Maehara said. “Starting with angiography and utilizing intravascular imaging based on the calcium scoring system helps PCI for angiographically visible or non-visible calcified lesions.”
Edited by

Se Hun Kang, MD
CHA Bundang Medical Center, Korea (Republic of)
Written by



