Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-030
Best of Both Worlds - Debulking With DK Crush in Complex Bifurcation
By Wan Faizal Bin Wan Rahimi Shah, Mohamed Nazrul Mohamed Nazeeb, Afif Ashari, Faten Aqilah Aris, Yee Sin Tey, Wei Liang Lee, Amin Ariff Nuruddin
Presenter
Wan Faizal Bin Wan Rahimi Shah
Authors
Wan Faizal Bin Wan Rahimi Shah1, Mohamed Nazrul Mohamed Nazeeb1, Afif Ashari1, Faten Aqilah Aris1, Yee Sin Tey1, Wei Liang Lee1, Amin Ariff Nuruddin1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-030
CORONARY - Bifurcation/Left Main Diseases and Intervention
Best of Both Worlds - Debulking With DK Crush in Complex Bifurcation
Wan Faizal Bin Wan Rahimi Shah1, Mohamed Nazrul Mohamed Nazeeb1, Afif Ashari1, Faten Aqilah Aris1, Yee Sin Tey1, Wei Liang Lee1, Amin Ariff Nuruddin1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
L. D.
Relevant Clinical History and Physical Exam
Patient is a 63-year-old male with background Diabetes Mellitus and Hypertension. He underwent bypass surgery with 4 grafts in 2017. He presented with dizziness and chest pain. We treated as Unstable Angina, but a CT cerebral angio revealed a right cerebral parietotemporal dural AV fistula. Further referral to neurosurgical team and cerebral DSA revealed bilateral ECA and Torcula Herophili Dural AVF. Suggested cerebral embolization but with graft study beforehand to delineate cardiac risk.
Relevant Test Results Prior to Catheterization
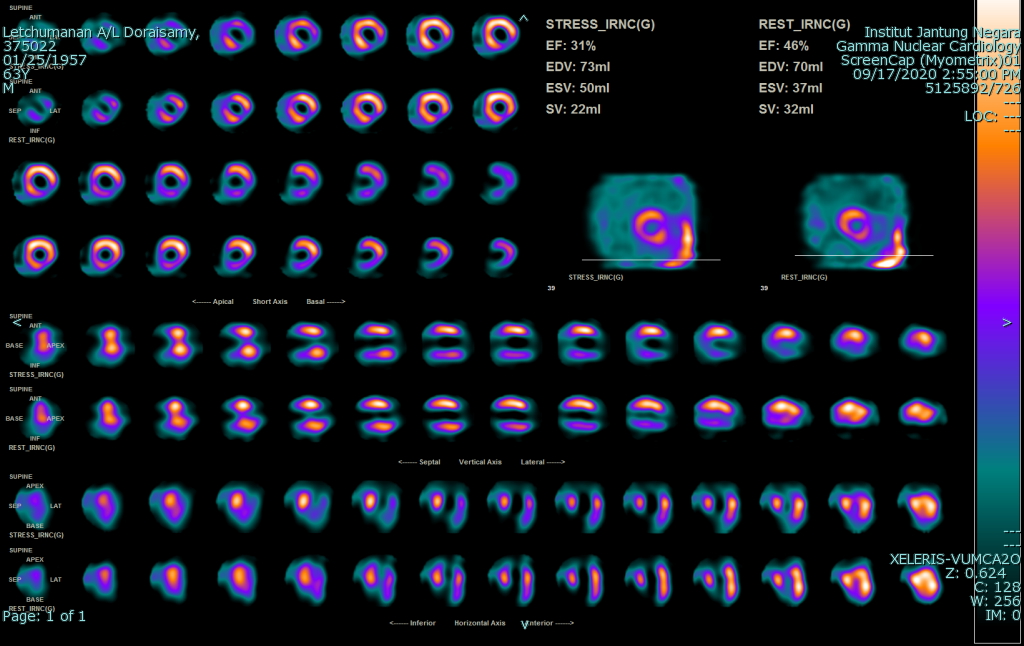
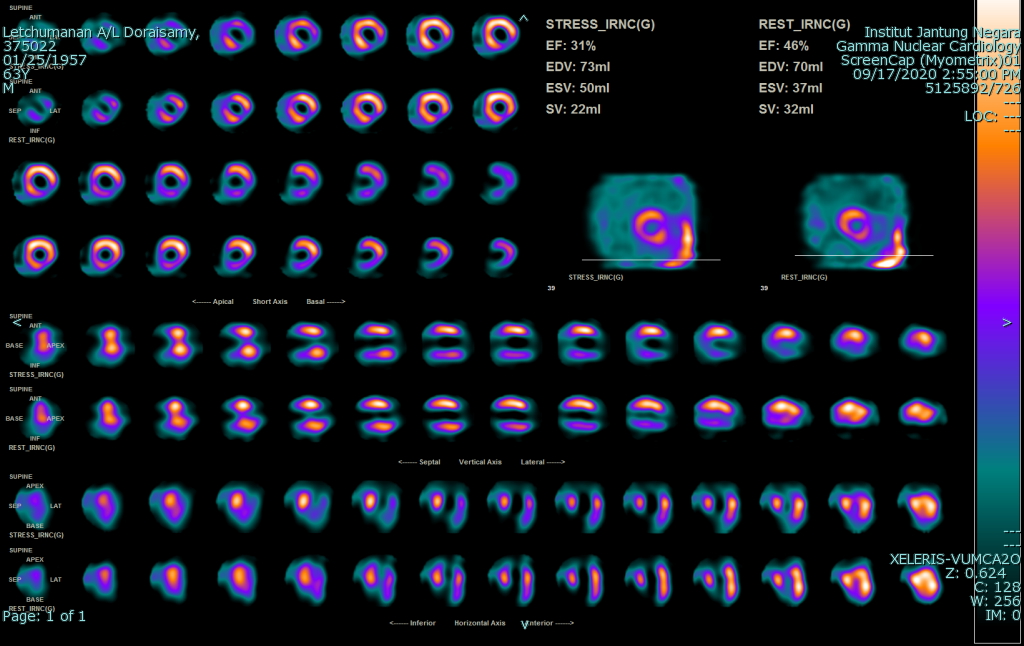
We decided to perform myocardial perfusion scan with Technetium first. It showed moderate stress induced ischaemia at LCx/RCA territory. This led us to perform graft study later.
Relevant Catheterization Findings
Graft study performed by right femoral approach showed results as below.
Native Coronary ArteriesLMS – distal 60% (calcified)LAD – severe ostio-proximal, occluded mid (calcified)- a large septal branch is seen supplied by proximal LAD segmentLCx – severe ostio-proximal, ectatic mid segment (calcified)RCA – small, CTO ostial
GraftsLIMA-LAD – patentSVG-intermediate – patentSVG-diagonal and SVG-distal LCx - stumps
Based on findings above, we planned for complex bifurcation PCI of LM-LAD-LCx.
 CAG 1.avi
CAG 1.avi
 CAG 7.avi
CAG 7.avi
 CAG 9.avi
CAG 9.avi
Native Coronary ArteriesLMS – distal 60% (calcified)LAD – severe ostio-proximal, occluded mid (calcified)- a large septal branch is seen supplied by proximal LAD segmentLCx – severe ostio-proximal, ectatic mid segment (calcified)RCA – small, CTO ostial
GraftsLIMA-LAD – patentSVG-intermediate – patentSVG-diagonal and SVG-distal LCx - stumps
Based on findings above, we planned for complex bifurcation PCI of LM-LAD-LCx.
Interventional Management
Procedural Step
In anticipation of neurosurgical procedure, we planned for PCI using stents with good short DAPT data. However, due to complexity of LM-LAD-LCx bifurcation with significant calcification, we are unable to avoid a 2-stent strategy. We opted DK-crush technique due to immense familiarity and excellent long term outcomes from recent studies.We treated LCx as main branch and LAD as side branch. 7Fr right femoral approach used. A Diamondback 360 OAS system utilized for both debulking and tackling the angulated LCx. There was difficulty to glide assist beyond into LCx, so forward sanding is done first. First runs at 80k RPM, with final crossing of lesion with a crown jump seen. Backward sanding was utilized thereon, providing better control of crown.Subsequently, ostial LCx pre-dilated with Scoreflex NC 3.0 x 15 mm and Wolverine 3.5 x 10 mm balloon. We reused the Wolverine 3.5 x 10 mm balloon for ostial LAD lesion. We secured the LM-LAD with Xience 3.5 x 18 mm stent, crushed with 3.5 mm NC and subsequently kissed with two 3.5 mm NC balloons.Then we stented LM-LCx with Resolute Onyx 3.5 x 38 mm stent. This was post-dilated with 3.5 mm NC with similar kissing using two 3.5 mm NC balloons. Final POT performed with 4.0 mm NC @ 20 atm.Final results showed excellent stent expansion with no complications encountered.
 CAG 14.avi
CAG 14.avi
 CAG 39.avi
CAG 39.avi
 CAG 40.avi
CAG 40.avi
Case Summary
Patient discharged well. Cerebral embolization was carried out successfully, and was last seen in our clinic being well in October 2021.
Calcified vessels in post-CABG patients are a common finding, owing to hardening of lesions over time. One must be expected to use all the necessary tools especially in complex PCI. We believe the usage of OAS in angulated, calcified segments is safer owing to slower speed of crown movement. As compared to intravascular lithotripsy, it also provides versatility in debulking vessels of different calibers. Finally, high-bleeding-risk patients are mandated to receive short DAPT stents. There should be no excuse, with abundance of such data in newer generation stents.
Calcified vessels in post-CABG patients are a common finding, owing to hardening of lesions over time. One must be expected to use all the necessary tools especially in complex PCI. We believe the usage of OAS in angulated, calcified segments is safer owing to slower speed of crown movement. As compared to intravascular lithotripsy, it also provides versatility in debulking vessels of different calibers. Finally, high-bleeding-risk patients are mandated to receive short DAPT stents. There should be no excuse, with abundance of such data in newer generation stents.


