Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-172
Case Report: Refractory Chest Pain After Transcatheter Aortic Valve Implantation
By Uei Lin Chen, Tsung-Yu Ko, Chih-Fan Yeh, Mu-Yang Hsieh, Ching-Chang Huang, Mao-Shin Lin
Presenter
Uei Lin Chen
Authors
Uei Lin Chen1, Tsung-Yu Ko1, Chih-Fan Yeh1, Mu-Yang Hsieh1, Ching-Chang Huang1, Mao-Shin Lin1
Affiliation
National Taiwan University Hospital, Taiwan1,
View Study Report
TCTAP C-172
STRUCTURAL HEART DISEASE - Valvular Intervention: Aortic
Case Report: Refractory Chest Pain After Transcatheter Aortic Valve Implantation
Uei Lin Chen1, Tsung-Yu Ko1, Chih-Fan Yeh1, Mu-Yang Hsieh1, Ching-Chang Huang1, Mao-Shin Lin1
National Taiwan University Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
2905780
Relevant Clinical History and Physical Exam
An 85-year-old woman presented with intermittent chest tightness and dyspnea for 6 months. She had hypertension,diabetes mellitus, paroxysmal atrial fibrillation and end-stage renal disease under regular hemodialysis. The physical examination revealed high-pitched,crescendo-decrescendo, mid-systolic murmur.
Relevant Test Results Prior to Catheterization
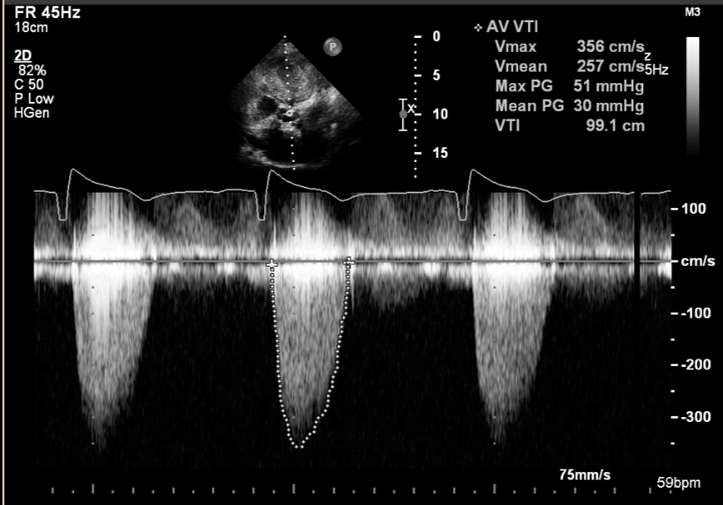
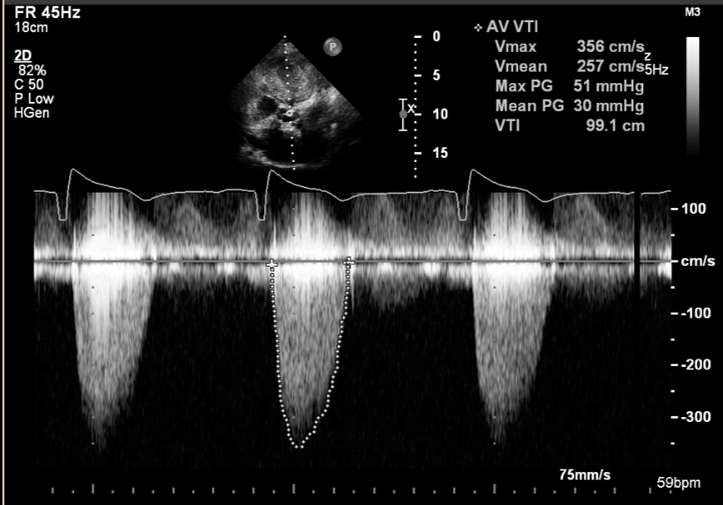
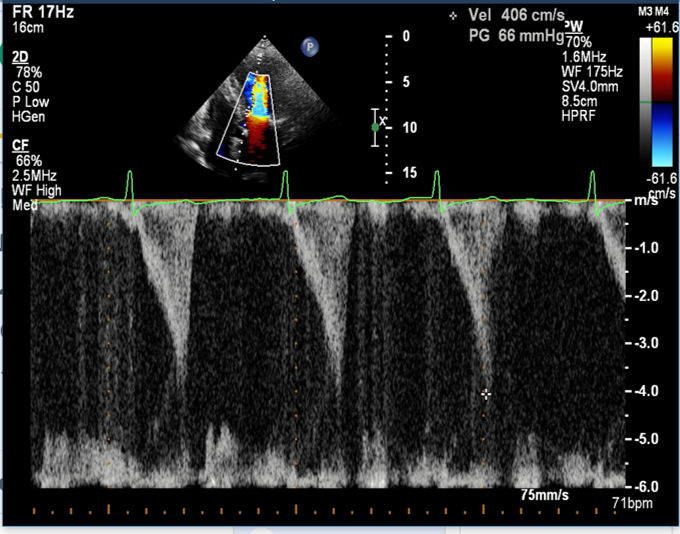
A transthoracic echocardiography revealed normal systolic function (LVEF=72%), concentric left ventricular hypertrophy without intraventricular pressure gradient and severe aortic calcification and stenosis(Vmax=356 cm/s, Mean PG=30 mmHg, AVA=0.92 cm2).
 PSAX.avi
PSAX.avi
Relevant Catheterization Findings
1stintervention
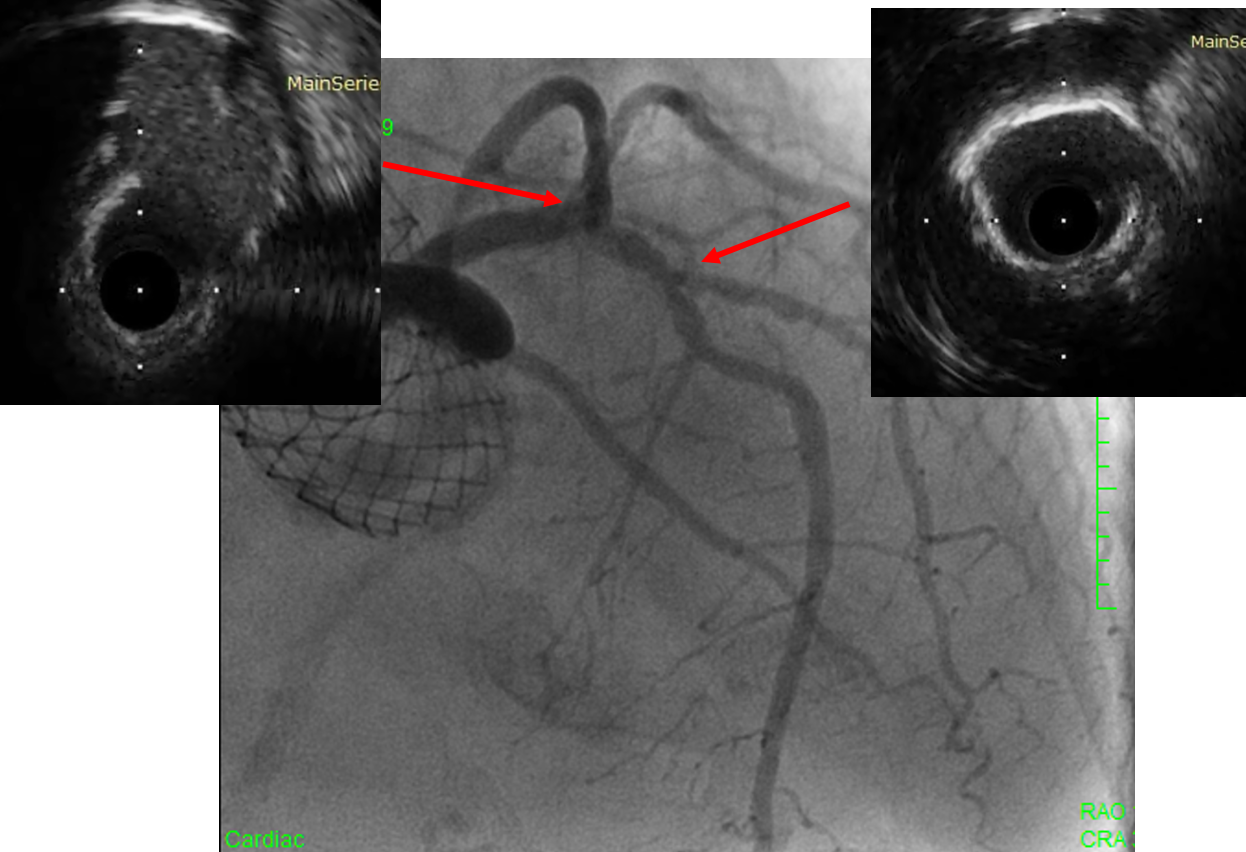
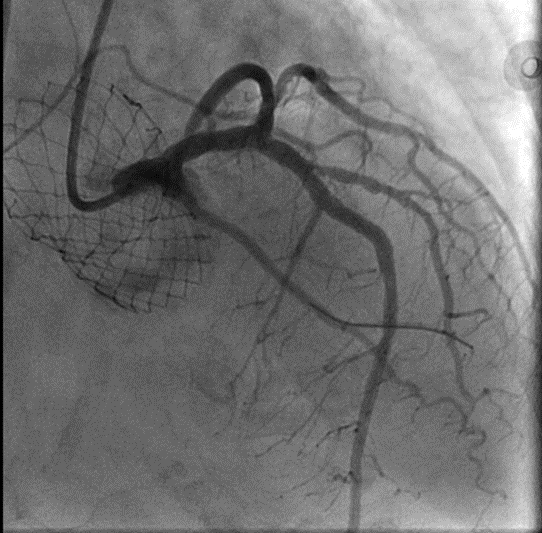
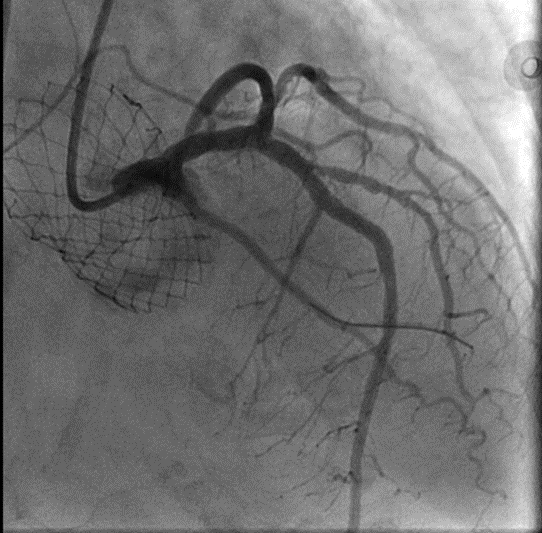
2nd interventionThe LAD ostial lesion was evaluated by IVUS, which showed large plaque burden with minimal luminal area of 3.0 mm2
 CAG1.avi
CAG1.avi
 CAG1_2.avi
CAG1_2.avi
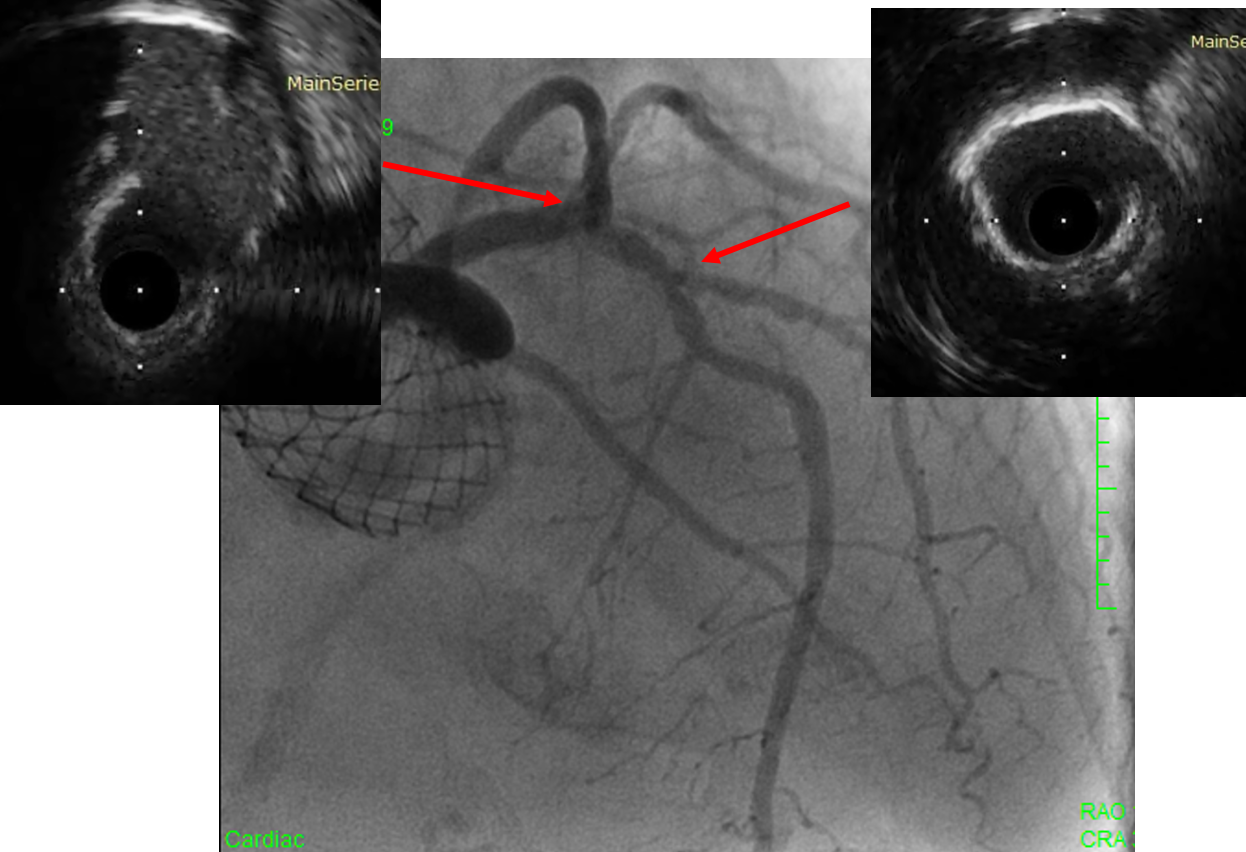
2nd interventionThe LAD ostial lesion was evaluated by IVUS, which showed large plaque burden with minimal luminal area of 3.0 mm2
Interventional Management
Procedural Step
1stintervention
2ndintervention (7 months later, due to persistent chest pain)
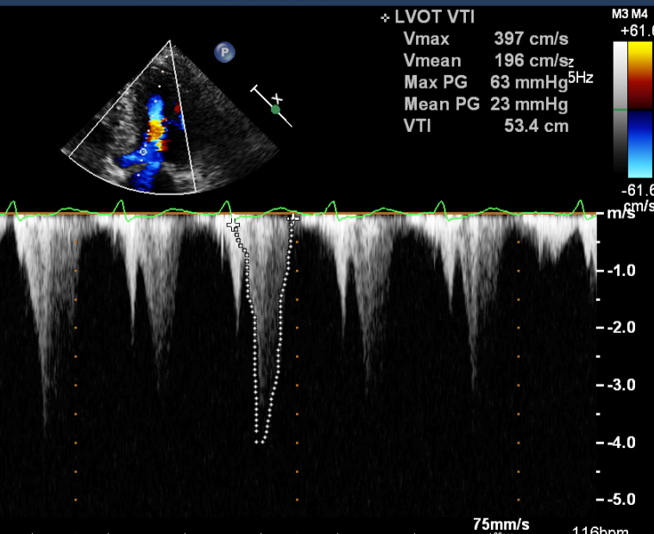
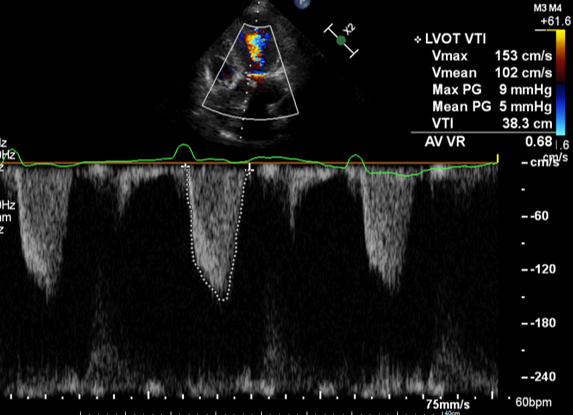
Refractory chest pain was still complained after intervention. A transthoracic echocardiography revealed significant left ventricular outflow tract obstruction (pressure gradient increased to 63 mmHg),which was not found on the pre-operative evaluation. After bisoprolol/diltiazem administration and right ventricular pacing with permanent pacemaker (DDDR), the pressure gradient decreased to 9 mmHg and her chest pain resolved.
 TAVI.avi
TAVI.avi
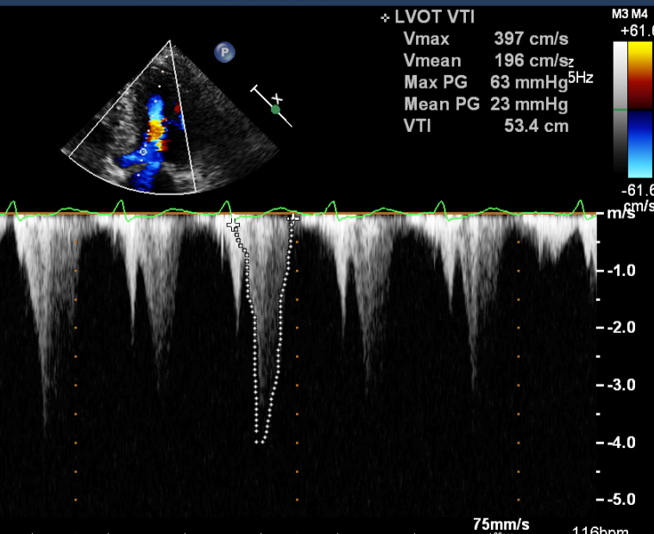
 TTE after TAVI and PCI.png
TTE after TAVI and PCI.png
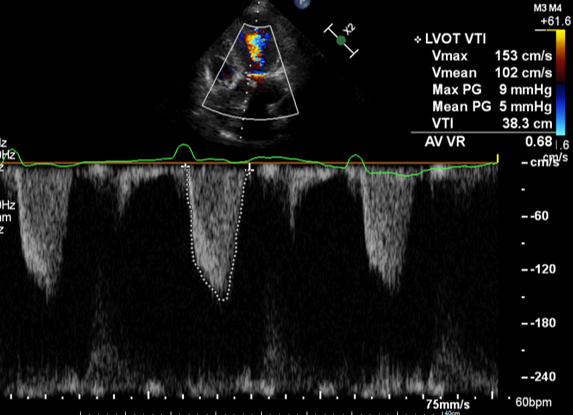
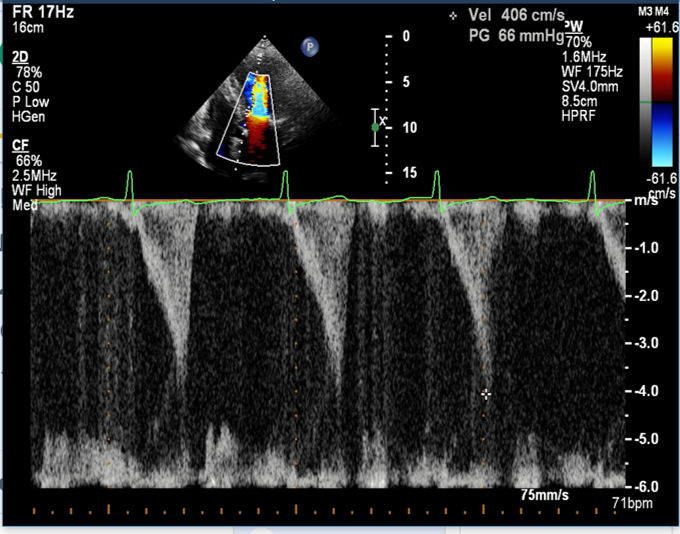
 TTE 5 years prior to TAVI (mild AS only).png
TTE 5 years prior to TAVI (mild AS only).png
2ndintervention (7 months later, due to persistent chest pain)
Refractory chest pain was still complained after intervention. A transthoracic echocardiography revealed significant left ventricular outflow tract obstruction (pressure gradient increased to 63 mmHg),which was not found on the pre-operative evaluation. After bisoprolol/diltiazem administration and right ventricular pacing with permanent pacemaker (DDDR), the pressure gradient decreased to 9 mmHg and her chest pain resolved.
Case Summary
In elderly patients with severe aortic stenosis, hypertrophic cardiomyopathy was occasionally found to coexist. Even though TAVI significantly relieves transaortic pressure gradient caused by aortic stenosis, TAVI may worsen left ventricular outflow obstruction caused by hypertrophic cardiomyopathy. Therefore, the evaluation before TAVI should include the LVmyocardium, while the hemodynamic consequence after TAVI procedures should be assessed. Treatment targeting both aortic stenosis and LV outflow obstruction should be thoroughly evaluated before the intervention in all patients.


