Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-056
Front Door, Back Door? Keep Knocking Until One Door Opens: Percutaneous Coronary Angioplasty to a Chronically Occluded Right Coronary Artery Via Multiple Antegrade and Retrograde Approaches
By Khai Chih Teh, Siti Dalila Adnan, Jayakhanthan Kolanthaivelu, Shaiful Azmi Yahaya
Presenter
Khai Chih Teh
Authors
Khai Chih Teh1, Siti Dalila Adnan2, Jayakhanthan Kolanthaivelu3, Shaiful Azmi Yahaya1
Affiliation
National Heart Institute, Malaysia1, Serdang Hospital, Malaysia2, Cardiovascular Sentral Kuala Lumpur, Malaysia3,
View Study Report
TCTAP C-056
CORONARY - Chronic Total Occlusion
Front Door, Back Door? Keep Knocking Until One Door Opens: Percutaneous Coronary Angioplasty to a Chronically Occluded Right Coronary Artery Via Multiple Antegrade and Retrograde Approaches
Khai Chih Teh1, Siti Dalila Adnan2, Jayakhanthan Kolanthaivelu3, Shaiful Azmi Yahaya1
National Heart Institute, Malaysia1, Serdang Hospital, Malaysia2, Cardiovascular Sentral Kuala Lumpur, Malaysia3,
Clinical Information
Patient initials or Identifier Number
448933
Relevant Clinical History and Physical Exam
A 32 year old male, diabetic was seen following a thrombolysed anteroseptal myocardial infarction. He has exertional angina, NYHA class II and uneventful physical examination.
Coronary angiogram showed severe LAD disease with CTO proximal RCA. Echocardiogram showed reduced LVEF 29%; myocardial viability study showed transmurally infarcted mid- distal LAD and viable RCA.
SYNTAX II score recommends CABG but he refused surgery; we planned for PCI to CTO RCA.
Coronary angiogram showed severe LAD disease with CTO proximal RCA. Echocardiogram showed reduced LVEF 29%; myocardial viability study showed transmurally infarcted mid- distal LAD and viable RCA.
SYNTAX II score recommends CABG but he refused surgery; we planned for PCI to CTO RCA.
Relevant Test Results Prior to Catheterization
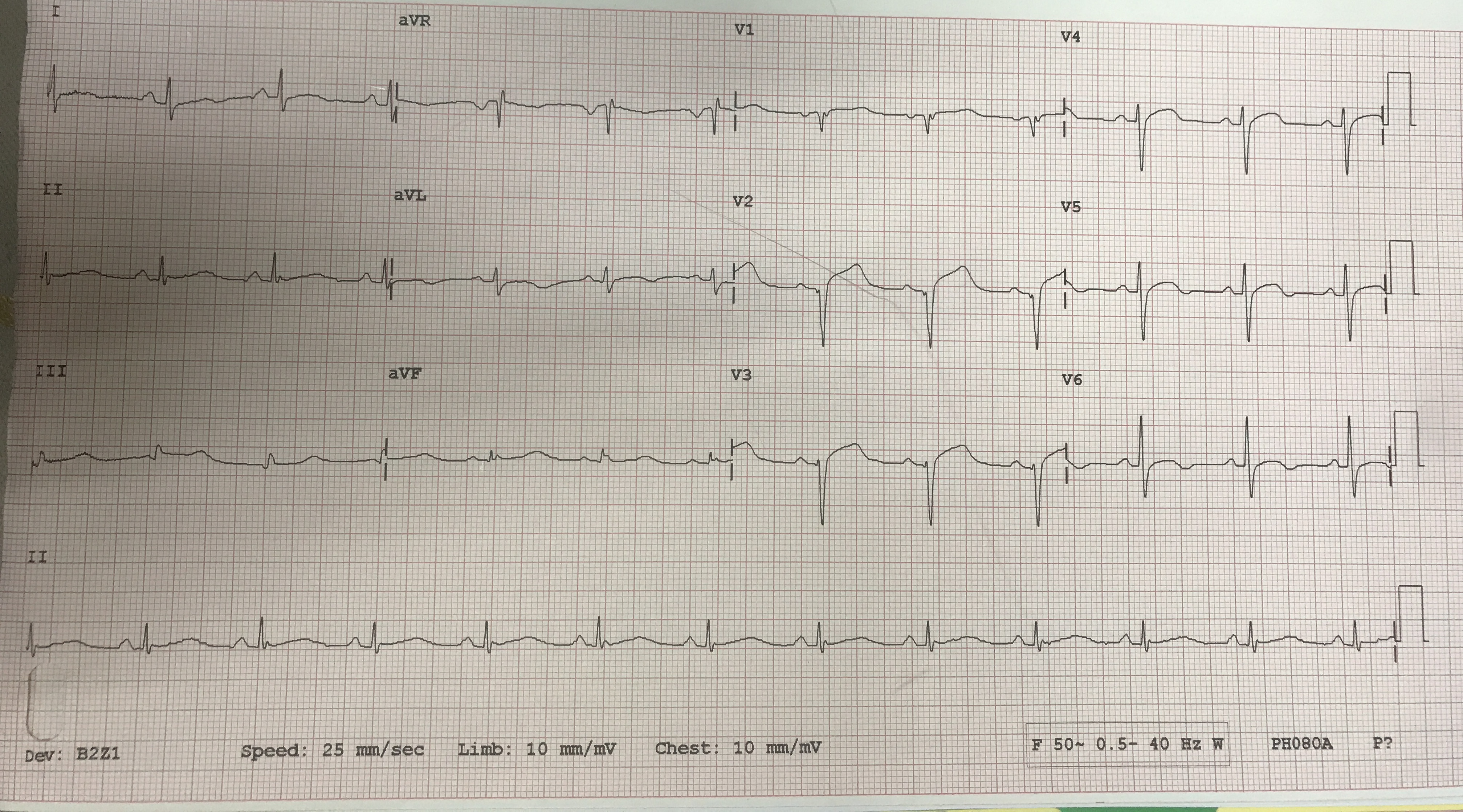
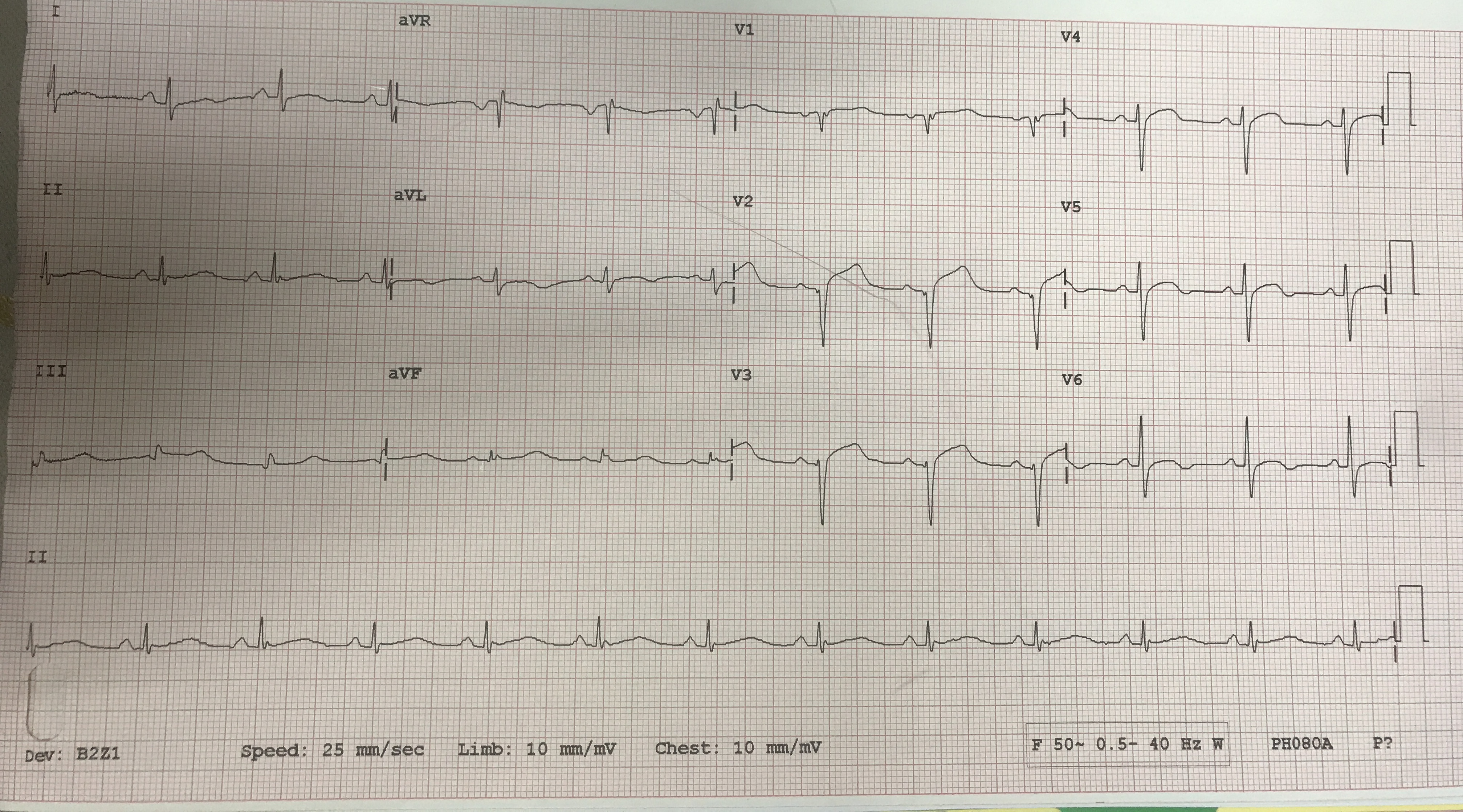
ECG: Q wave anteroseptal leadsTroponin T: 106 pg/mlECHO: LVEF 29%, TAPSE 1.5cm, mild MR and TRTechnitium viability: LVEF 15%, transmural infarction mid to distal LAD; small non transmural infarct RCA territory. Other segments all viable
Relevant Catheterization Findings
Left main: normal
LAD: tight stenosis proximal LAD; retrogrades from septal branches to distal posterior lateral branch of RCA
LCX: mild proximal disease
RCA: chronic total occlusion (CTO) proximal RCA with bridging collaterals to RV branch
J-CTO score: 2 (length > 20mm, previous failed attempt)
First attempt PCI to CTO RCA with JR 3.5 guide, FIELDER XT wire in FINECROSS catheter crossed proximal cap but entered subintimal space and failed to proceed; procedure abandoned.
 las diagnostic cranial.avi
las diagnostic cranial.avi
 las diagnostic RCA.avi
las diagnostic RCA.avi
 las PCI RCA first attempt.avi
las PCI RCA first attempt.avi
LAD: tight stenosis proximal LAD; retrogrades from septal branches to distal posterior lateral branch of RCA
LCX: mild proximal disease
RCA: chronic total occlusion (CTO) proximal RCA with bridging collaterals to RV branch
J-CTO score: 2 (length > 20mm, previous failed attempt)
First attempt PCI to CTO RCA with JR 3.5 guide, FIELDER XT wire in FINECROSS catheter crossed proximal cap but entered subintimal space and failed to proceed; procedure abandoned.
Interventional Management
Procedural Step
First attempt PCI CTO RCA with 6Fr Amplatz guide, FIELDER XR wire in FINECROSS microcatheter entered subintimal space and failed to progress further. Procedure abandoned with small non flow limiting dissections in mid RCA.
Reattempt PCI CTO RCA was performed a week later via right radial 6 Fr EBU 3.5 to the left coronary and right femoral Amplatz 1 7 Fr guide to the RCA. Initial antegrade approach with GAIA II wire in FINECROSS microcatheter entered existing subintimal tract again and was abandoned.
We proceeded for retrograde attempt via LAD septal branch. PCI to proximal LAD with a 4.0 x 13 COMBO stent was first performed, followed by wiring through 2nd septal with a FIELDER FC wire in FINECROSS microcatheter which successfully reached distal cap in PL branch. However microcatheter failed to deliver distally despite predilating septal with a 0.85 x 5mm balloon. Further attempts of retrograde dissection and reentry with FIELDER FC and XT in a new CARAVEL microcatheter at the distal CTO cap were unsuccessful as wire preferentially deflects in to side branches.
We then reattempted antegrade approach with GAIA III wire in microcatheter and finally crossed the lesion successfully. Predilatation with 1.0 x 5mm and 2.0 x 12mm balloons were done, followed by stenting with 3.0 x 48mm, 3.5 x 48mm and 4.0 x 40mm stents from distal to ostium RCA. Postdilatation with an NC 4.0 balloon in the proximal to ostium RCA yielded good results with TIMI III flow and no complications.
 las retrograde in septal.avi
las retrograde in septal.avi
 las antegrade cross lesion.avi
las antegrade cross lesion.avi
 las rca post pci.avi
las rca post pci.avi
Reattempt PCI CTO RCA was performed a week later via right radial 6 Fr EBU 3.5 to the left coronary and right femoral Amplatz 1 7 Fr guide to the RCA. Initial antegrade approach with GAIA II wire in FINECROSS microcatheter entered existing subintimal tract again and was abandoned.
We proceeded for retrograde attempt via LAD septal branch. PCI to proximal LAD with a 4.0 x 13 COMBO stent was first performed, followed by wiring through 2nd septal with a FIELDER FC wire in FINECROSS microcatheter which successfully reached distal cap in PL branch. However microcatheter failed to deliver distally despite predilating septal with a 0.85 x 5mm balloon. Further attempts of retrograde dissection and reentry with FIELDER FC and XT in a new CARAVEL microcatheter at the distal CTO cap were unsuccessful as wire preferentially deflects in to side branches.
We then reattempted antegrade approach with GAIA III wire in microcatheter and finally crossed the lesion successfully. Predilatation with 1.0 x 5mm and 2.0 x 12mm balloons were done, followed by stenting with 3.0 x 48mm, 3.5 x 48mm and 4.0 x 40mm stents from distal to ostium RCA. Postdilatation with an NC 4.0 balloon in the proximal to ostium RCA yielded good results with TIMI III flow and no complications.
Case Summary
This case illustrates a complex CTO PCI in a young patient with multivessel disease who refused surgery, requiring multiple approaches and strategy changes to achieve final successful results.
A stepwise approach of reattempting PCI to a previously unsuccessful vessel with proper planning and approach ( initial antegrade approach with retrograde injection, followed by retrograde attempt as a second option and then finally reattempting antegrade again successfully) ensured highest possibility of success while minimizing risks of complications.
Successful revascularization for a young patient with extensive coronary artery disease will dramatically reduce risk of future cardiac events and death.
A stepwise approach of reattempting PCI to a previously unsuccessful vessel with proper planning and approach ( initial antegrade approach with retrograde injection, followed by retrograde attempt as a second option and then finally reattempting antegrade again successfully) ensured highest possibility of success while minimizing risks of complications.
Successful revascularization for a young patient with extensive coronary artery disease will dramatically reduce risk of future cardiac events and death.


