Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-041
It Went Downhill When the Left Main Got Torn: An Ostial LAD Occlusion Intervention
By DASDO ANTONIUS SINAGA
Presenter
Dasdo Antonius Sinaga
Authors
DASDO ANTONIUS SINAGA1
Affiliation
AWAL BROS HOSPITAL, Indonesia1,
View Study Report
TCTAP C-041
CORONARY - Bifurcation/Left Main Diseases and Intervention
It Went Downhill When the Left Main Got Torn: An Ostial LAD Occlusion Intervention
DASDO ANTONIUS SINAGA1
AWAL BROS HOSPITAL, Indonesia1,
Clinical Information
Patient initials or Identifier Number
MR S
Relevant Clinical History and Physical Exam
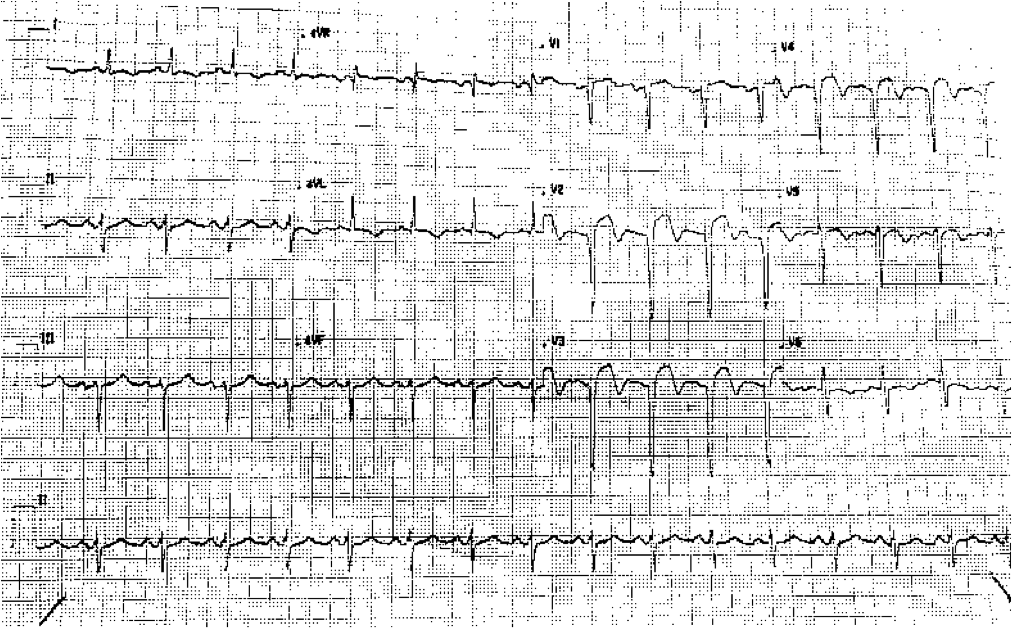
Fifty eight year old male patient with Diabetes, hyperlipidemia, hypertensive was referred with late onset Anterior STEMI, killip III, prolonged pain, bilateral rales, warm extremities. Blood pressure 128/68 mmHg, heart rate 80 bpm, ECG revealing anterior lead ST elevation with pathologic Q wave
Relevant Test Results Prior to Catheterization
HbA1C 10.2 mg/dLTrop I > 10 ug/LCrea 0.89 mg/dL
Relevant Catheterization Findings
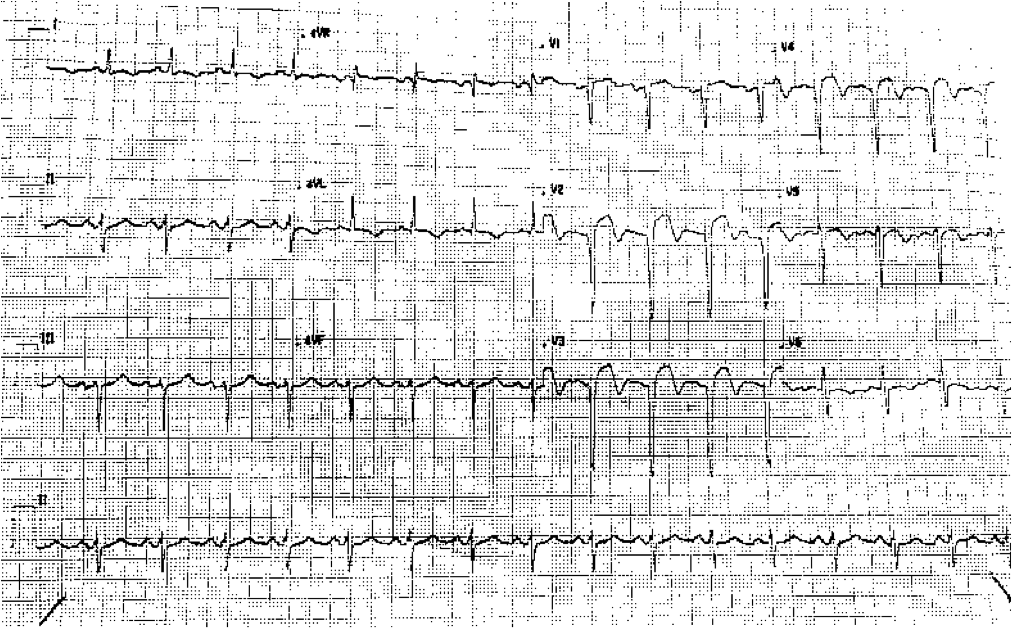
Diagnostic angiography revealed occluded ostial LAD with no significant disease at the LM and LCX.RCA was dominant with moderate disease distally, giving faint collaterals to the mid-distal LAD.






Interventional Management
Procedural Step
PCI from right radial approach, using 6Fr BL 3.0 guiding catheter, unsuccessful plain wiring to LAD due to the occlusion and challenging angulation. Then used a CrusadeR dual-lumen catheter, Balancium guidewire to LCX, and Balancium guide wire through side lumen to LAD, successfully crossed LAD occlusion, up to mid LAD. Wire was pushed distally with support of 1.0 x 6 mm balloon. After crossing, pre dilatation done with the 1.0 balloon and the 2.0 x 15 mmcompliant balloon, LAD flow improved to TIMI II.After ballooning, there was dissection at LM, the flaps going to LAD and LCX. Patient crashed on table, BP 70/40, severe chest pain, treated with saline bolus, dopamine infusion, morphine boluses and sedation. Patient agitated, both catheter and wires were disengaged, hence catheter was re-engaged, then rewired to LAD and LCX, fortunately wire still went to true lumen.Quick decision whether to do 2-stent strategy or provisional LM-lAD stenting. Considering patient's unstable condition and LCX flow was still TIMI III, decided to proceed with provision LM-LAD stenting.Implanted 2 stents with Biomatrix 3.5 x 19, Biomatrix 2.75 x 36 mm from LM to mid LAD, flow improved to TIMI III. Optimisation with IVUS, post-dilatation was done with 3.5 mm NC and 4.5 mm NC, another Biomatrix 2.75 x 19 stent was implanted at mid LAD.Rewired the LCX through stent struts, repeat IVUS study was done with good MLAs at LM-LAD. There was remaining LCX type-B dissection with TIMI III flow,left alone.
 2 dissection video.mpeg
2 dissection video.mpeg
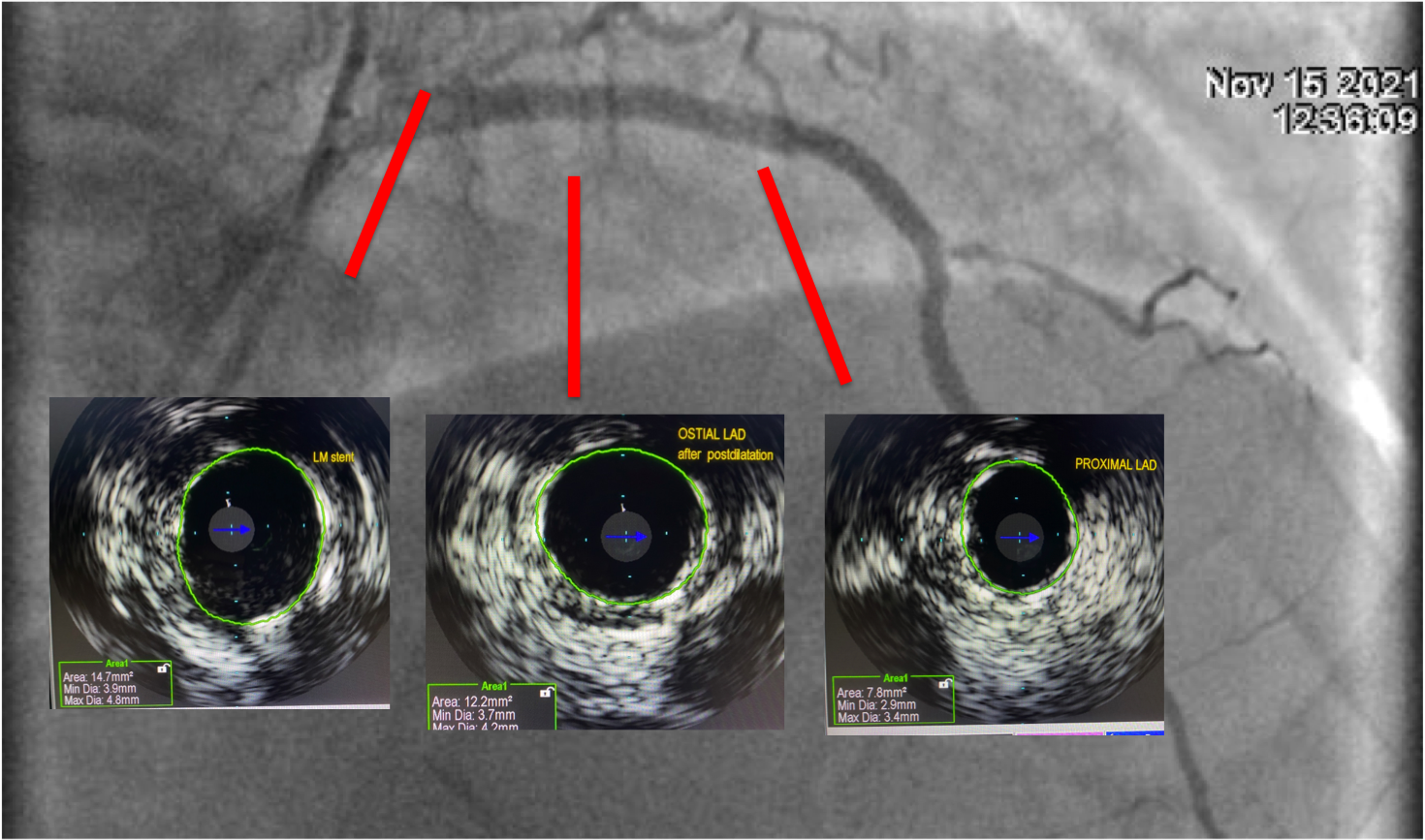
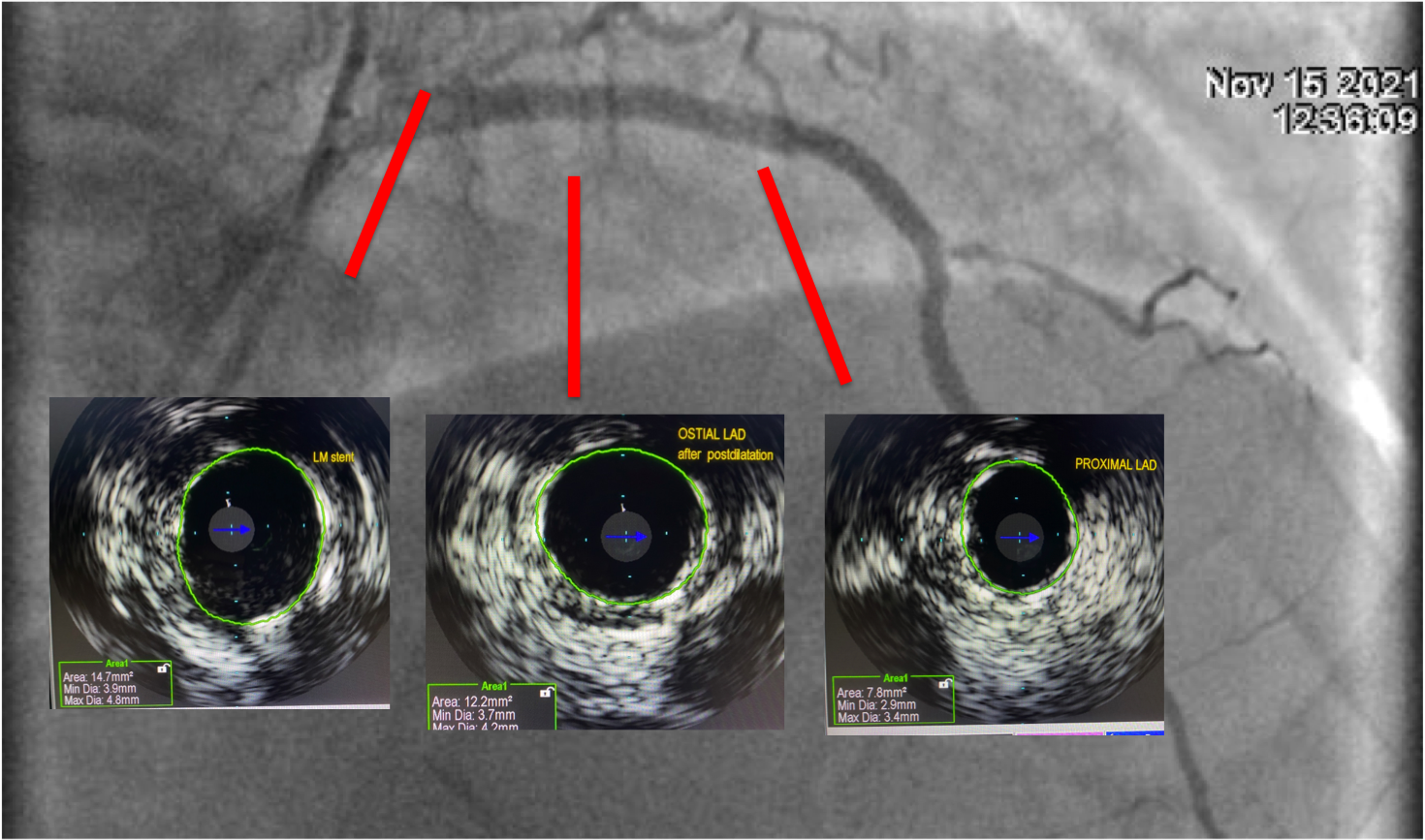
Case Summary
LAD ostium intervention was facilitated with dual lumen catheter (CrusadeR) to help wire crossing the hard thrombotic plaque. After pre dilatation, LM-LAD-LCX dissection induced by (likely) guiding catheter, caused patient deterioration. Problem identification, hemodynamic stabilisation must be conducted quickly to save the patient.In the setting of STEMI, patient's instability, provisional LM - LAD stenting was done immediately. Two-stent strategy would make the procedure more complicated, and require more time to recover the flow. Intravascular imaging would be mandatory for stent optimlsation and improve long-term result.


