Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-092
A Lesson Well Learnt - Acute Stent Thrombosis Resulting in Inferior Myocardial Infarction
By Tjen Jhung Lee, Azhari Rosman, Nay Thu Win, Jayakhanthan Kolanthaivelu
Presenter
Tjen Jhung Lee
Authors
Tjen Jhung Lee1, Azhari Rosman1, Nay Thu Win2, Jayakhanthan Kolanthaivelu3
Affiliation
National Heart Institute, Malaysia1, Royal Free London, United Kingdom2, Cardiovascular Sentral Kuala Lumpur, Malaysia3,
View Study Report
TCTAP C-092
CORONARY - Complications
A Lesson Well Learnt - Acute Stent Thrombosis Resulting in Inferior Myocardial Infarction
Tjen Jhung Lee1, Azhari Rosman1, Nay Thu Win2, Jayakhanthan Kolanthaivelu3
National Heart Institute, Malaysia1, Royal Free London, United Kingdom2, Cardiovascular Sentral Kuala Lumpur, Malaysia3,
Clinical Information
Patient initials or Identifier Number
450331
Relevant Clinical History and Physical Exam
54 year old gentleman with background history of DM. He presented on the 9/11/2021 for acute onset chest pain, with ECG showing ST elevation in the leads II, III and AVF. Primary angioplasty was done. He had a small and anomalous RCA which was difficult to engage, but was faintly visualized by aortic injection. The LM and LAD vessels were normal, and he had a dominant large LCX with a 99% stenosis in the mid-distal segment. Primary PCI was done with implantation of a 2.5x20mm DES.
Relevant Test Results Prior to Catheterization
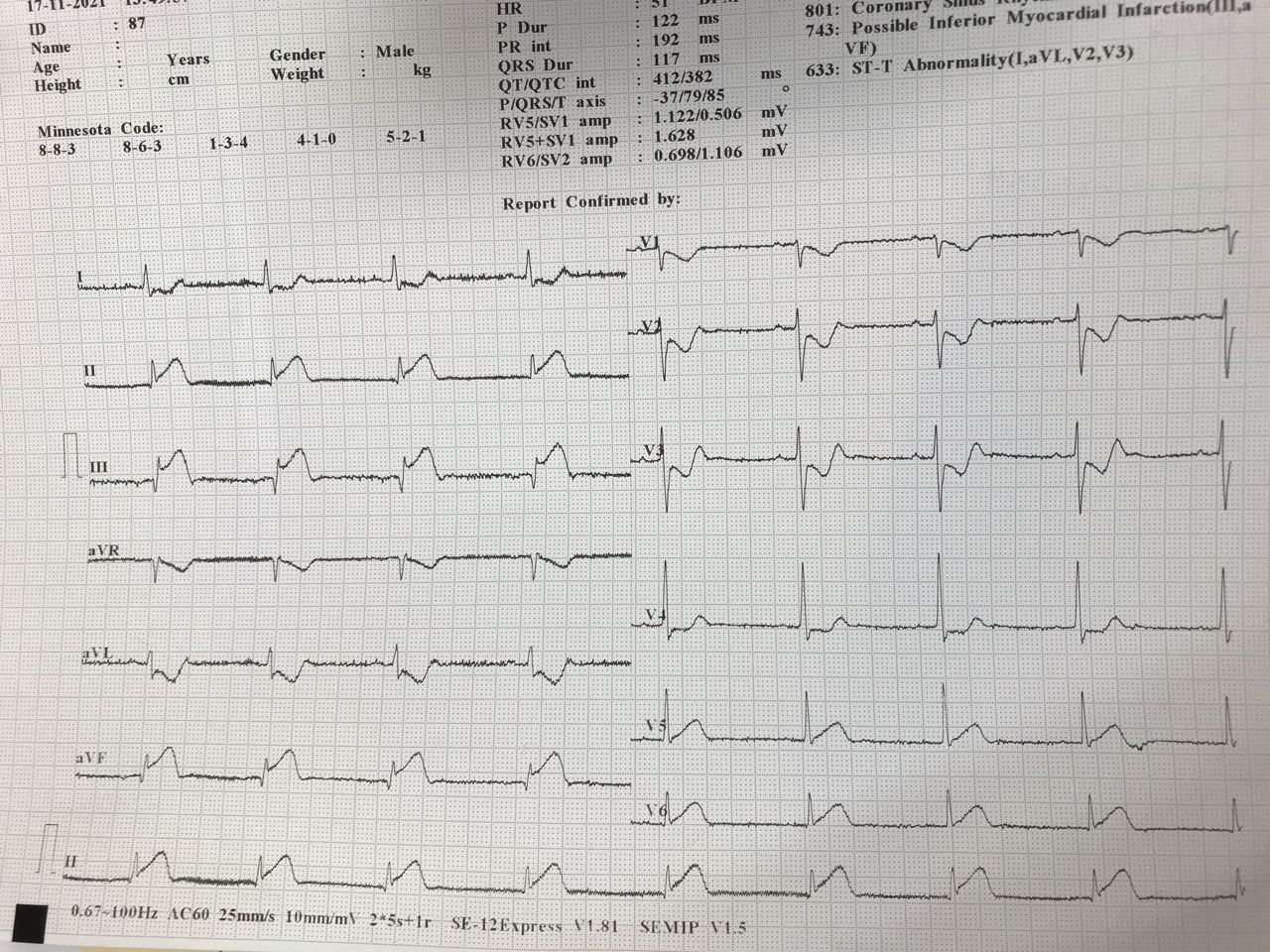
On the 17/11/2021 he presented again with typical chest pain, and ECG showed ST elevation in leads II III and AVF. A diagnosis of possible acute stent thrombosis was made, and patient was immediately brought to the ICL.
Troponin results were 2400pg/ml
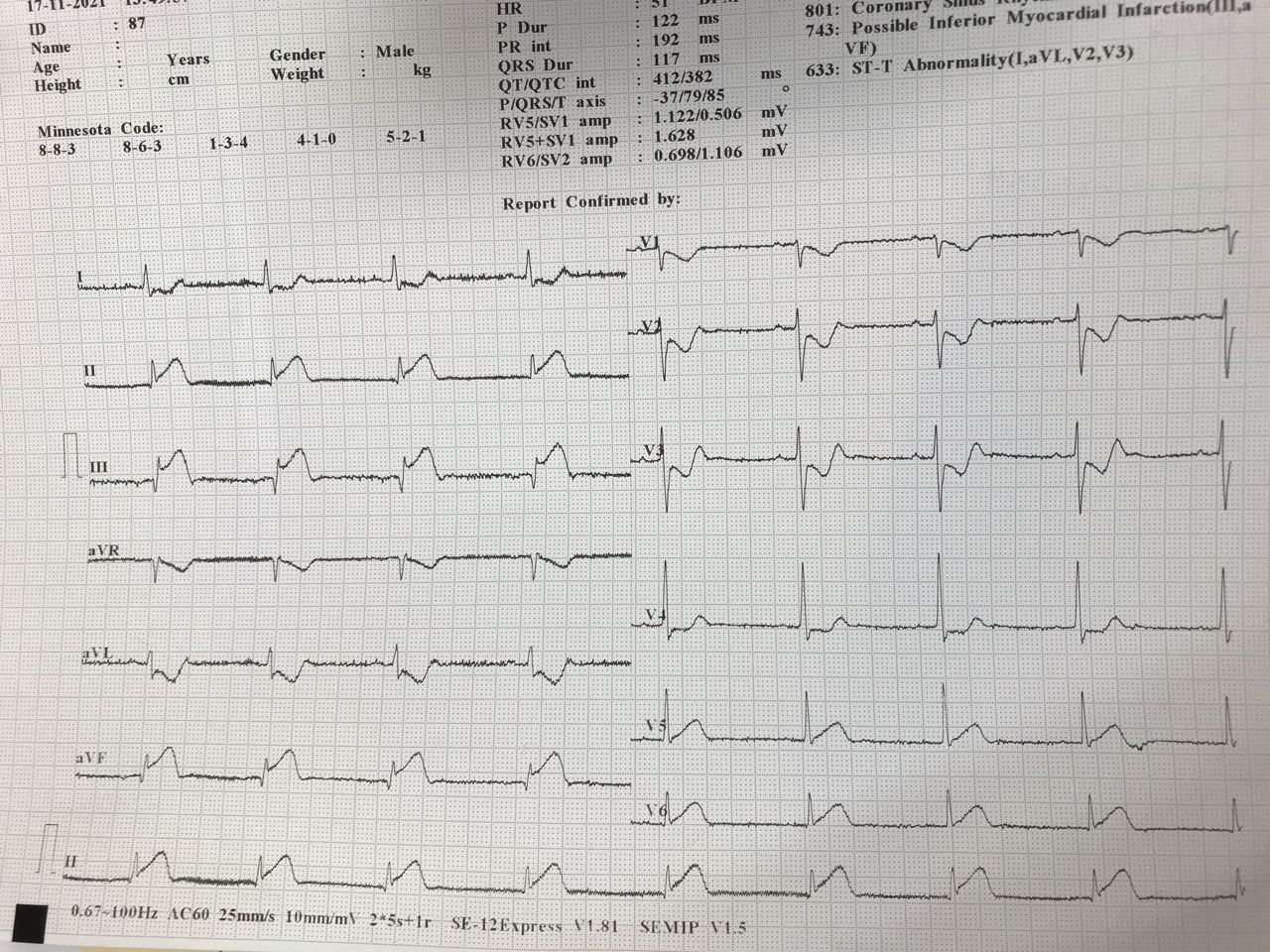
Troponin results were 2400pg/ml
Relevant Catheterization Findings
First angiogram on the 9/11/2021 showed severe 99% stenosis, which was subsequently stented with 2.5x20mm DES. The repeat angiogram, done as a primary on 17/11/2021, showed acute occlusion of the LCX vessel.The LAD and LM vessels were normal.
 1) First primary.avi
1) First primary.avi
 2) 2.5 20 DES implantation.avi
2) 2.5 20 DES implantation.avi
 3) Final first primary angioplasty.avi
3) Final first primary angioplasty.avi
Interventional Management
Procedural Step
Access was gained via the right femoral artery, as the right radial artery access was still swollen from the prior procedure. An EBU 3.5 6Fr guide provided good support, and we used a RunThrough Floppy wire into the LCX, and successfully wired through the occluded segment and stent into the distal LCX. Thrombus aspiration was performed with the EXPORT catheter, with red thrombus removed. Flow was established and IVUS was done. The earlier placed stent was underexpanded, being sized to 2.5-2.7mm in a vessel which had a diameter of 3.5-3.8mm on IVUS. The MSA was 5.2mm2. On further angiographic assessment, the LCX vessel appears to be foreshortened in the caudal view, and the true size and length better appreciated in the LAO-Cranial view. The stent was upsized with 3.0mm then3.5mm NC balloons. In the LAO-Cranial view, another 90% severe stenosis was seen in the distal LCX, for which we performed Drug Coated Balloon therapy with a 2.5x25mm DCB.
 1) Second primary.avi
1) Second primary.avi
 2) IVUS run.mp4
2) IVUS run.mp4
 3) Final second primary angioplasty.avi
3) Final second primary angioplasty.avi
Case Summary
Stent undersizing and under expansion is a risk factor for acute and subacute stent thrombosis. In this case, proper vessel sizing was difficult in the index procedure due to the atypical path of a large and dominant LCX, with the vessel and stent being viewed in a foreshortened angle in the usual Caudal/ RAO-caudal view. This emphasizes utility of IVUS when performing PCI in vessels hampered by unfavourable angiographic views. This case also points out how routine angiographic views might not highlight the distal large branches when assessing a dominant LCX.


