Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-035
Complex Evaluation in Multivessel Coronary Artery Disease With Common Trunk Critical Involvement and Complete Revascularization During Hospitalization
By Farhat Fouladvand, Elisabetta Iardino, Bernardo Cortese, Gaetano Di Palma
Presenter
Elisabetta Iardino
Authors
Farhat Fouladvand1, Elisabetta Iardino2, Bernardo Cortese1, Gaetano Di Palma1
Affiliation
Clinica San Carlo, Italy1, Ospedale Bolognini, Italy2,
View Study Report
TCTAP C-035
CORONARY - Bifurcation/Left Main Diseases and Intervention
Complex Evaluation in Multivessel Coronary Artery Disease With Common Trunk Critical Involvement and Complete Revascularization During Hospitalization
Farhat Fouladvand1, Elisabetta Iardino2, Bernardo Cortese1, Gaetano Di Palma1
Clinica San Carlo, Italy1, Ospedale Bolognini, Italy2,
Clinical Information
Patient initials or Identifier Number
BGS 22/0371940
Relevant Clinical History and Physical Exam
We present a case of an 80 y of age man with coronary risk factors diabetes, hypertension, dyslipidemia and familiarity without previous history of cardiac disease and known nephrolithiasis and urethral stenosis. He came to our observation during the second COVID wave pandemic within the emergency department for chest discomfort during hypertensive crisis and evidence of not known complete left bundle branch block and minimal elevation of TnI-HS levels.
Relevant Test Results Prior to Catheterization
Echocardiography demonstrated septal dyskinesia with ejection fraction of 53%, no relevant valvular disease.
Relevant Catheterization Findings
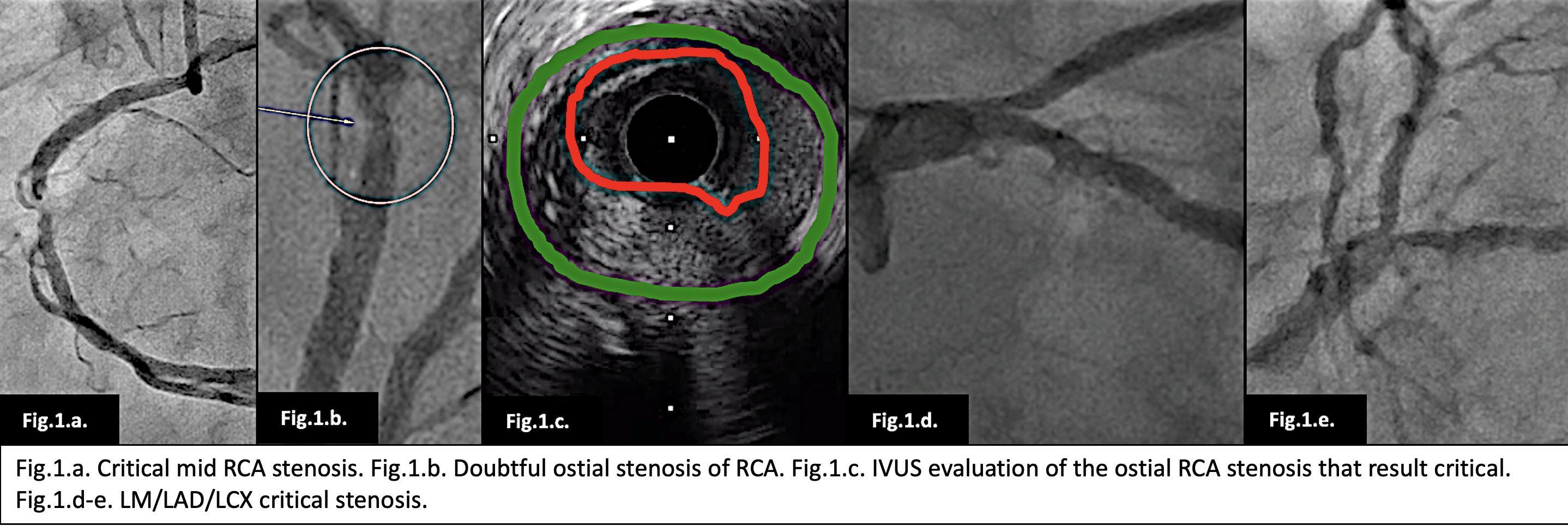
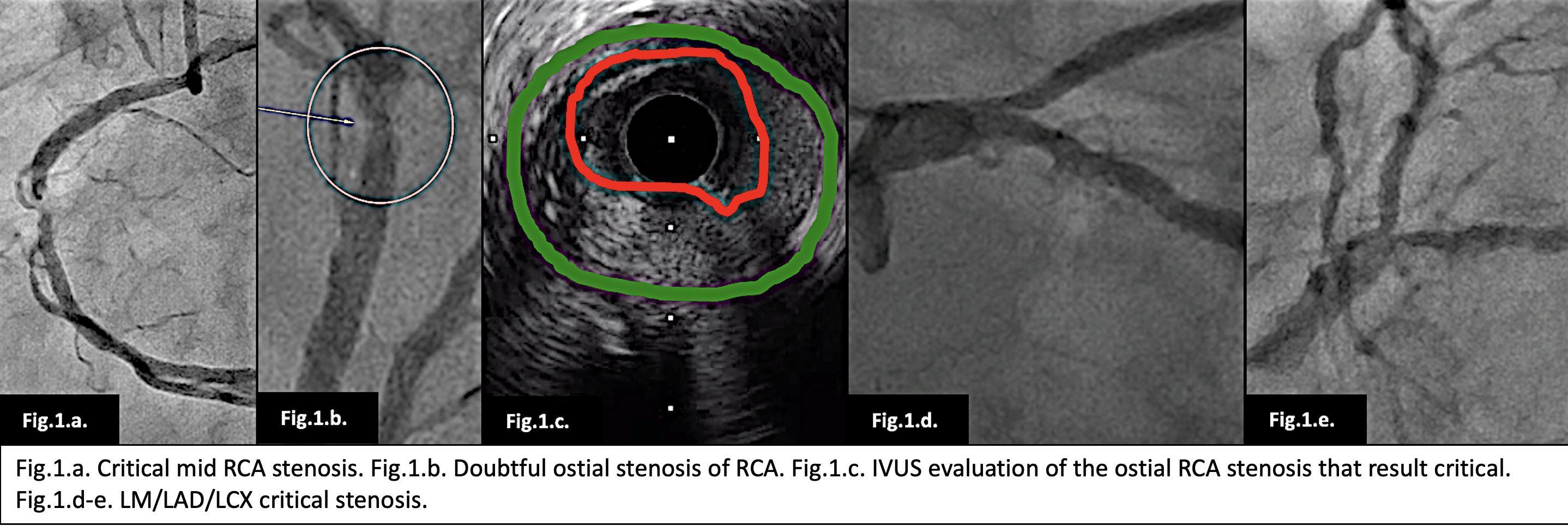
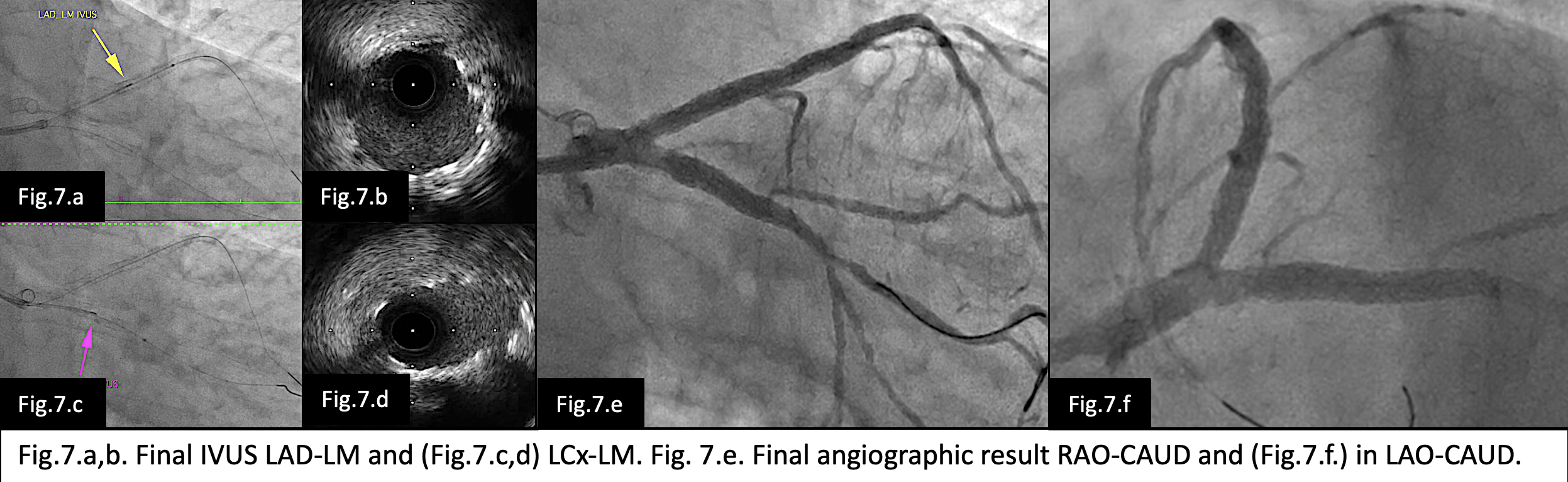
Angiography shoed critical mid RCA and ostial, LM (Medina 1.1.1) mid LAD and LCx stenosis (Fig.1). The patients definitively refused surgical revascularization choosing percutaneous one. At this point the mid (Fig.2.a.) and ostial RCA (Fig.2.b.) stenosis were fixed with DES with optimal angiographic and IVUS (Fig.2.c-d.) results. The left coronary system was studied with IVUS demonstrating significant LM/LAD/LCx stenosis and presence of circumferential calcification (Fig.3.a-b).


Interventional Management
Procedural Step
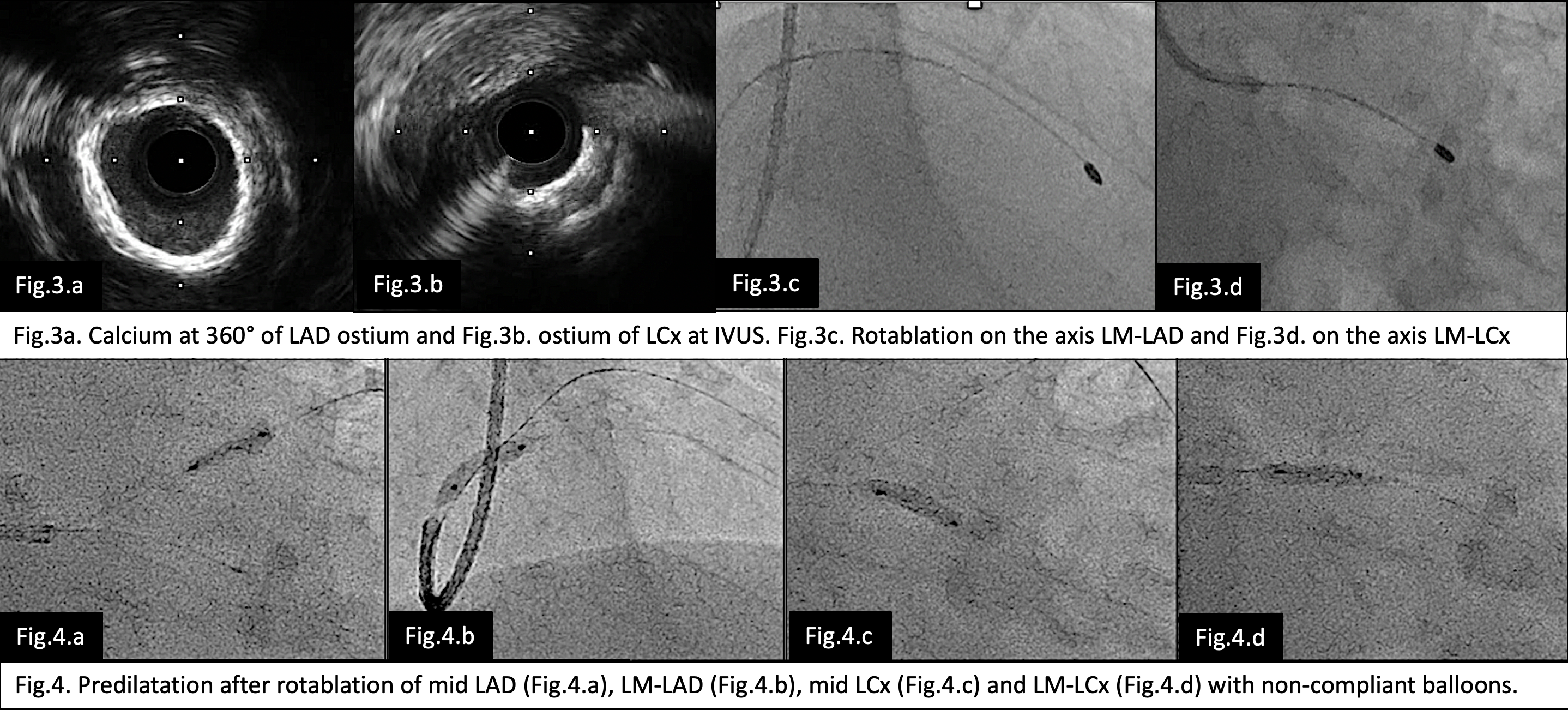
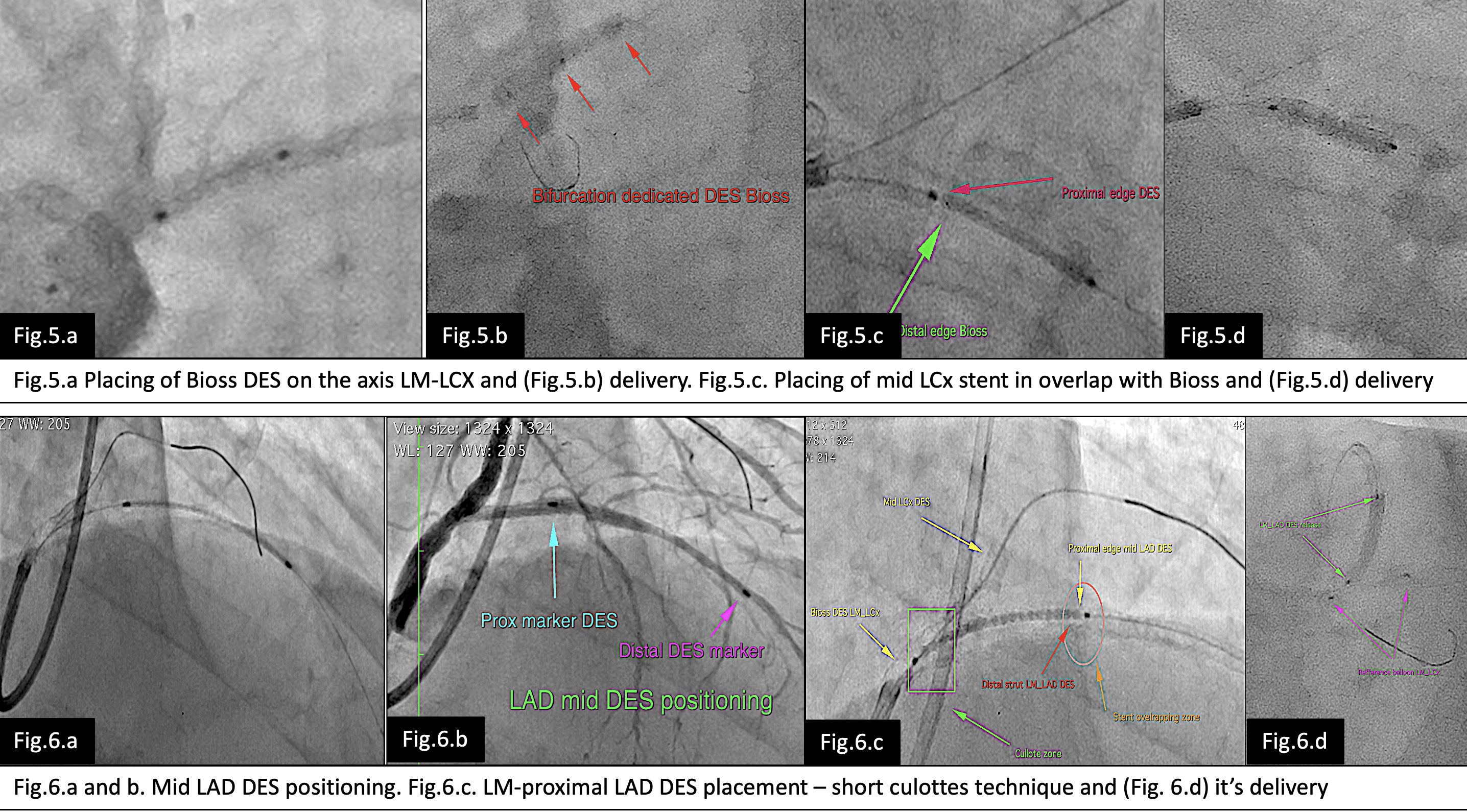
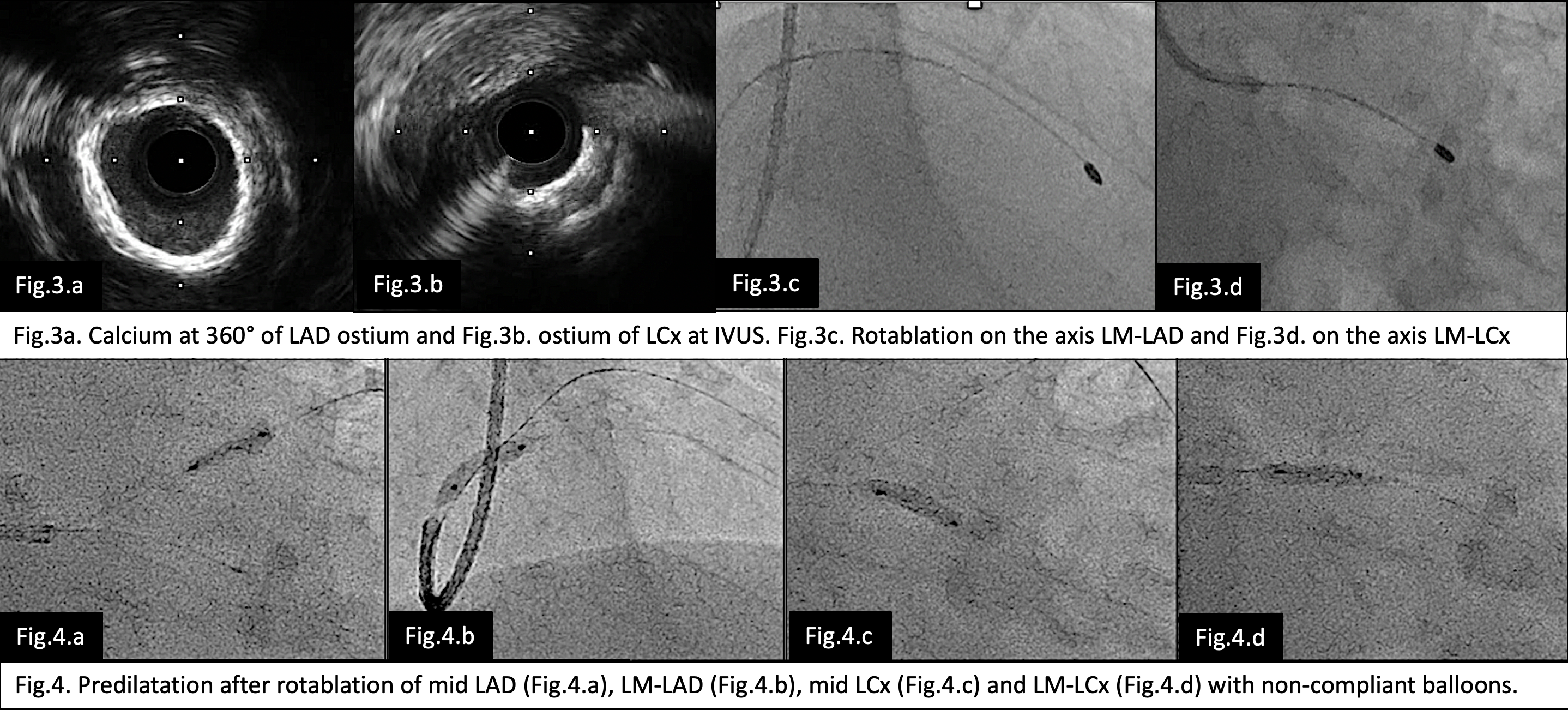
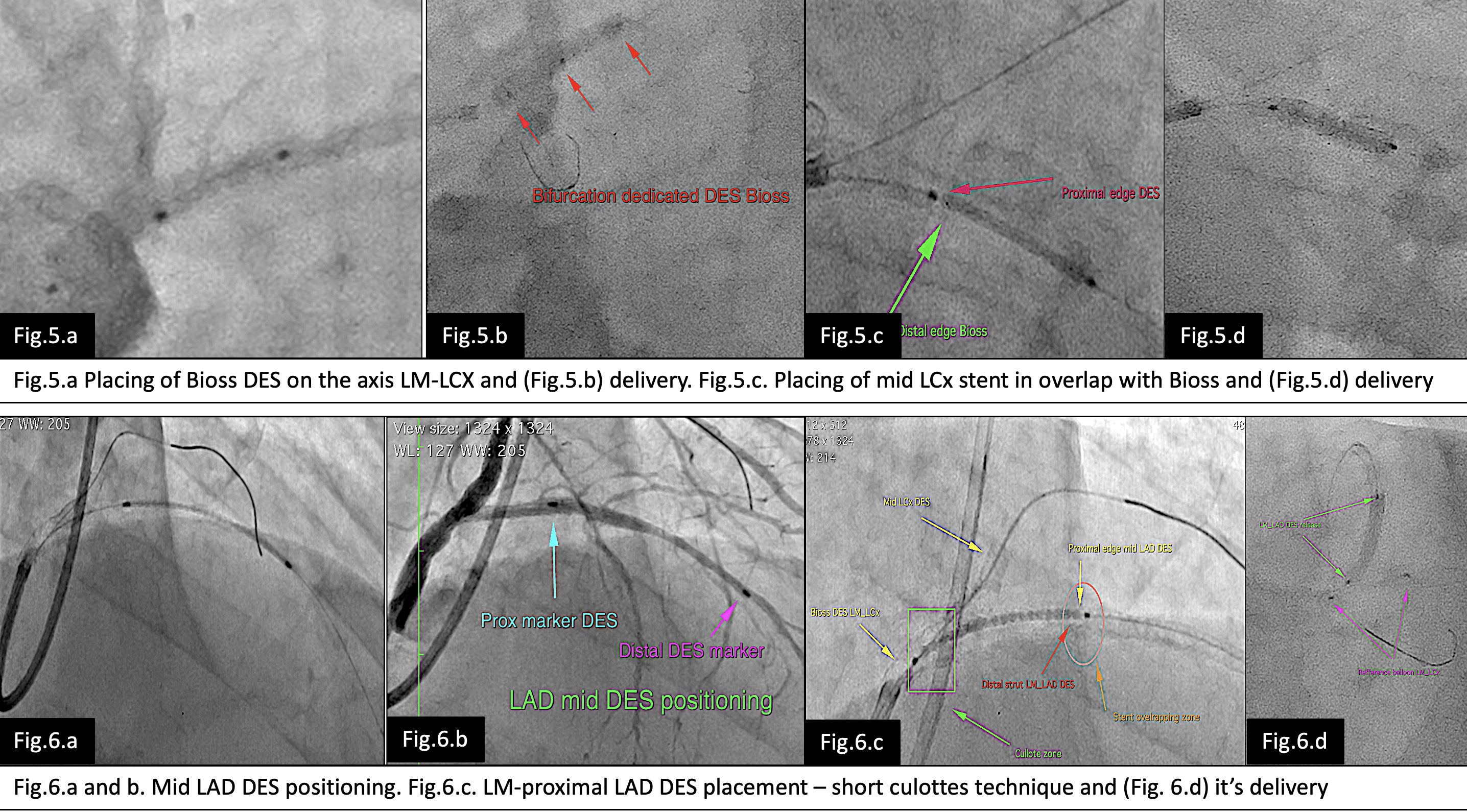
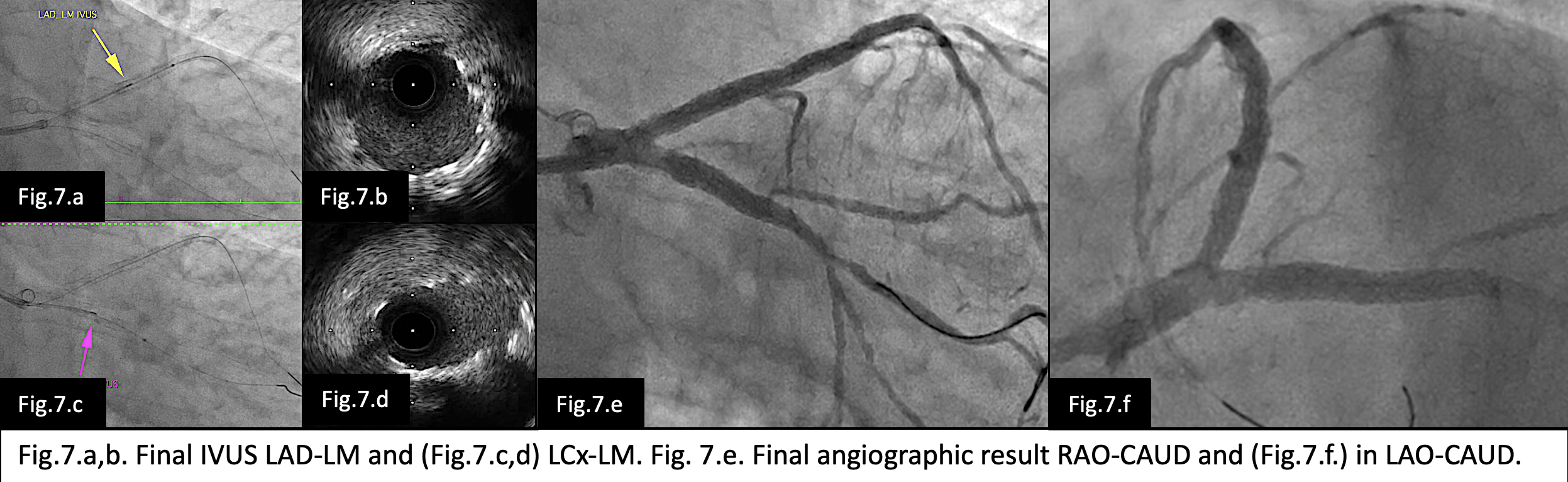
As a first step we performed rotational atherectomy on the axis LM-LAD (Fig. 3.c.) and LM-LCx (Fig. 3.d.) with 1,75 mm burr and after rewiring LAD (Renato) and LCx (Sion Blu) we repeated IVUS evaluation. Predilatation with non-compliant balloons of mid LAD and LCx and LM-LAD and LM-LCx (Fig.4.) was performed and then a bifurcation dedicated stent BIOSS was places on the axis LM-LCx (Fig. 5.a-b). The procedure continued with placing of a second DES in the mid LCx (Fig.5.c-d) and third DES in the mid LAD (Fig.6.a-b.). Then we placed a fourth DES (Fig.6.c-d.) in the axis LM-LAD (culottes with the just placed BIOSS on LM-LCx). Procedure was ended with DOT, POT, kissing balloon and final POT. Optimal result with IVUS (Fig.7.a-d) and angiography (Fig.7.e-f.) was achieved. The patient was discharged after 48 hours on DAPT and clinical follow-up was scheduled for 1st and 3th month and angiography control after 6 months.
Case Summary
Adopting the common rules and guidelines in the every day practice as in our case with NSTEMI patient rule-in/rule-out, early coronary angiography in less than 24 hours from admission, all vessels revascularization during index hospitalization, imaging in the left main treatment, stent like preparation of vessels before stenting and in some cases using of dedicated bifurcation stent can increase the success rate and reduce the complication rate.


